Abstract
Summary
Adequate vitamin D/calcium supplementation during osteoporosis (OP) treatments seems insufficient. This cohort study within a national claims database evaluated calcium/vitamin D co-prescription in postmenopausal women initiating an OP treatment. A high co-prescription rate was observed with three quarters of women supplemented with calcium and/or vitamin D in agreement with current recommendations.
Introduction
Adequate calcium/vitamin D supplementation should be taken in combination with antiresorptive drugs in OP treatment. Despite guidelines, supplementation appears to be insufficient. The objective of this study was to describe and estimate co-prescription rates of calcium/vitamin D among postmenopausal women initiating an OP treatment.
Methods
All women over 50 years with a first claim for a bisphosphonates, raloxifene, or strontium prescription filled between May and August 2010 were included in a retrospective cohort study. Data source was the health insurance claims database of the Rhône-Alpes area.
Results
Among 4,415 women, 77.0 % had co-prescription of calcium or vitamin D with initial OP treatment, of which 2,150 (49.7 %) had both calcium and vitamin D. The proportion of women with calcium and/or vitamin D (81.7 %) was significantly higher when OP treatment was a bisphosphonate compared to strontium (70.9 %) or raloxifene (67.0 %) (p < 0.05). Among women prescribed both calcium and vitamin D, 7.6 % received a bisphosphonate and vitamin D ± calcium fixed-combination pack. General practitioners prescribed two thirds of initial supplementation treatment (66.9 %). Patients were twice as likely to be prescribed supplementation when the prescriber was a rheumatologist (OR = 2; 95 % CI = 1.57–2.54).
Conclusion
Three quarters of women initiating OP treatment were supplemented with calcium and/or vitamin D in agreement with current recommendations. This represents a high co-prescription rate.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Many antiresorptive and anabolic drugs are approved for the prevention and/or treatment of postmenopausal osteoporosis (OP), including bisphosphonates, selective estrogen receptor modulators raloxifene, strontium ranelate, and the recombinant parathyroid hormone teriparatide [1–3]. Also, calcium and vitamin D are needed for normal skeletal homeostasis and considered as part of first-line treatment in every patient with newly diagnosed osteoporosis [4, 5]. Moreover, adequate calcium and vitamin D supplementation should also be taken in combination with these antiosteoporotic drugs as stated in the summary of product characteristics and in consensus guidelines for the prevention and treatment of osteoporosis [2, 6–8]. These recommendations are based on the fact that all previous clinical studies of these drugs showing fracture risk reduction have been conducted in patients receiving adequate levels of calcium and vitamin D [5]. It is also acknowledged that a high proportion of patients with osteoporosis have a higher risk of presenting with low initial levels of calcium and/or vitamin D [4, 9–11]. Finally, effectiveness of osteoporosis treatment relies on patient’s adherence to all medications including calcium and vitamin D co-medication [4, 5, 12, 13].
Despite existing recommendations, the prescription of calcium and/or vitamin D supplementation with antiosteoporotic drugs appears to be suboptimal in Europe [5, 14, 15]. However, there are only few studies on co-prescription rates in France. In a pharmacoepidemiological study conducted in a primary care setting to characterize patients with postmenopausal OP, only 8.3 % were taking calcium and vitamin D supplementation in combination with their OP treatment [16]. Conversely, in another cross-sectional study, 106 among 155 women (68 %) were taking calcium or vitamin D supplements in addition to antiosteoporotic treatment [17]. In a case–control analysis including osteoporotic women receiving specific treatment for postmenopausal OP, calcium supplementation ranged from 6.2 % in women with fracture history to 7.7 % in women without fracture history, and vitamin D supplementation ranged from 47.9 to 58.8 %, respectively [12]. No definite conclusions can be drawn from these studies that showed high variability among observed results, probably due to the variety of sources on prescription information, selection biases, and methods used. None of these studies was based on a representative sample of patients, and the evaluation of calcium and vitamin D supplementation was not their primary objective. Combined calcium/vitamin D/bisphosphonate treatments were recently developed in order to increase supplementation intake and adherence through simplified regimens because of concern for lack of use of calcium and vitamin D with biphosphonates [14, 15]. However, no data on the real proportion of combination pack prescription among patients taking OP medication are available in literature.
Given the limited data on supplementation in OP treatment in France, the objective of this observational study was first to describe and estimate the co-prescription rate of calcium and vitamin D with OP treatments among postmenopausal women initiating an antiosteoporotic drug. The secondary objective was to evaluate the prescription rate of OP treatment/calcium/vitamin D fixed-combination pack among these women.
Materials and methods
This was a retrospective descriptive cohort study using reimbursement data from the French Insurance Healthcare system.
Data source
We used data provided by the administrative Extraction, Recherches, Analyses pour un Suivi Medico-Economique database “ERASME,” the medical reimbursement database of the Caisse Nationale d’Assurance Maladie des Travailleurs Salariés. This insurance covers all the reimbursements for all patients, including drugs and tests ordered by physicians [18, 19]. We performed the study with the cooperation of the Rhône-Alpes area (Service Informationnel de l’Assurance Maladie Rhône-Alpes). Organization of data collection and database has been previously described [20, 21].
Study sample
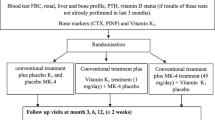
The source population was composed of all women aged 50 years and older identified in the ERASME database of the Rhône-Alpes area (about 6 million inhabitants) who filled an initial prescription for OP treatment between May 1 and August 1, 2010. A prescription date was retrieved for each identified dispensation. An initial prescription was defined as a reimbursement of bisphosphonates (i.e., etidronate, alendronate, ibandronate, risedronate, zoledronate), bisphosphonates, and calcium/vitamin D fixed-combination pack, raloxifene or strontium ranelate, with no prior reimbursement for one of these drugs during the 12 months preceding patient inclusion. The study sample included all patients with an available initial prescription date. The patients’ index date (inclusion date) for the analysis was the date of the initial prescription. Each patient was followed for 6 months from the index date.
Data collection
Age was determined at the time of the index prescription for initial OP treatment. All reimbursed prescriptions for OP treatments, calcium and vitamin D, BMD test by dual-energy x-ray absorptiometry, dates of hospital stays, and death during the follow-up period were extracted for each patient. Information on calcium/vitamin D prescription, BMD test, hospital stays during the 12-month pre-inclusion period was also retrieved from the database. For each antiosteoporotic drug, the following variables were abstracted: CIP code (Code Identifiant de Presentation, identification number assigned by the French health authorities), ATC code (anatomical therapeutic chemical classification system code and classification), date of prescription, date of prescription fulfillment, quantity delivered, and prescriber specialty.
Outcome measures
The primary outcome of the study was the number and proportion of women initiating an OP treatment who had a co-prescription of calcium and/or vitamin D. Three types of supplementation were defined at OP initiation: “calcium and vitamin D,” “calcium alone,” and “vitamin D alone.” All other cases were considered as not supplemented. A calcium/vitamin D supplementation prescription filled within the 12 months preceding index date was considered as a co-prescription when the expected duration of supplementation overlapped the initial OP prescription by at least 1 month. Any calcium/vitamin D filled within the 15 days following the inclusion was also considered as an appropriate co-prescription. Secondary outcome was the proportion of women with a prescription of bisphosphonates and vitamin D ± calcium fixed-combination pack among women receiving both calcium and vitamin D at the time of inclusion.
Statistical analysis
Results were presented as numbers and percentages of subjects for qualitative variables and as mean values with standard deviation (or median) for quantitative variables. Data on medications and BMD were described globally and by 10-year age category. Between-group comparisons were performed with χ² tests for qualitative variables. The threshold for statistical significance retained for the analyses was 0.05. Factors associated with the prescription of supplementation with calcium and/or vitamin D were evaluated by multivariate logistic regression analysis. Data were controlled, validated, and analyzed centrally using SAS® Enterprise Guide software version 4.3 (SAS Institute Inc., Cary, NC, USA) and SAS 9.2.
Ethics
Analyses performed using the database ERASME had been approved by the Commission Nationale de l’Informatique et des Libertés.
Results
Population description
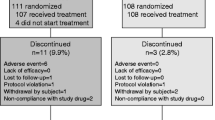
Overall, 4,415 women met the inclusion criteria and were included in the cohort. Eighty-seven women were excluded from the analysis, 60 who died during the 6-month follow-up period and 27 with vitamin D prescriptions not indicated for postmenopausal OP (alfacalcidiol and calcitriol). The remaining 4,328 women who filled a prescription for a first OP treatment between May 1 and August 1, 2010 constituted the study population. The mean age of patients was 69.2 years (SD, 10.5). A total of 4,333 OP treatments were initially prescribed. Bisphosphonates represented 60.4 % of these prescriptions (Table 1). Five patients were prescribed two different treatments concomitantly including strontium in both cases and either raloxifene or a bisphosphonate. Proportions of bisphosphonates and strontium prescription were higher for the 70–79 and >80 age groups, respectively 95.4 and 98.4 %, compared to raloxifene in the same age groups. Raloxifene was mainly prescribed in 50–59 and 60–69 age groups (86.9 % of raloxifene prescription) and decreased dramatically with age (p < 0.05; Table 1). General practitioners (GPs) prescribed two thirds of initial OP treatment (66.2 %), whereas rheumatologists and gynecologists represented around 22.2 % of prescribers. Only 10.1 % of initial OP treatment was prescribed in hospitals (Table 2). Raloxifene was more frequently (43.6 %) prescribed by gynecologists, whereas bisphosphonates were the first antiosteoporotic drugs prescribed by GPs and rheumatologists with respectively 61.1 and 69.2 % of their prescriptions (Table 2). A total of 1,709 women among 4,328 had a BMD test in the year prior to receiving their first prescription for OP treatment (39.5 %).
Supplementation at initiation of OP treatment
Among the 4,328 women initiating OP treatment, 3,331 (77.0 %) women had an initial or ongoing prescription with calcium and/or vitamin D supplementation including mainly: co-prescription of calcium and vitamin D in 2,150 (49.7 %) patients and vitamin D alone in 1,142 (26.4 %) women (Table 1). In the latter group, vitamin D3 supplementation represented 90.3 % of the prescriptions. Supplementation prescriptions represented a total of 3,518 treatments with calcium and/or vitamin D of which 91.2 % were filled concomitantly with the first OP treatment prescription or in the following 15 days. Nine hundred ninety-seven women (23.0 %) did not receive any supplementation at the time of initiating OP treatment. Type of supplementation did not significantly differ between age groups (Table 1 and Fig. 1). GPs prescribed two thirds of initial supplementation treatment (66.9 %), whereas rheumatologists (15.7 %) and gynecologists (5.7 %) represented 21.4 % of initial prescription (Table 2). Analysis of supplementation type as a function of prescriber did not show any significant difference (Table 2). The proportion of women receiving calcium and/or vitamin D (81.7 %) was significantly higher when initial OP treatment was a bisphosphonate compared to strontium (70.9 %) or raloxifene (67.0 %; p < 0.05; Table 3).
Co-prescription of calcium and vitamin D with combination pack
Among the 2,150 women with calcium and vitamin D at OP treatment initiation, 164 had prescriptions for a fixed-combination pack of bisphosphonates and vitamin D ± calcium (7.6 %). The majority of patients had separate prescriptions for OP treatments and supplementation (Table 1).
Multivariate analysis
Each variable identified as being significantly associated with a co-prescription antiosteoporotic drug, calcium, and/or vitamin D was entered into a multivariate logistic regression analysis (Table 4). This identified prescription with raloxifene or strontium as being significantly associated with absence of supplementation, whereas rheumatology specialty or hospital practitioners and presence of BMD before first OP treatment prescription were identified as significantly associated with a higher likelihood of receiving a supplementation prescription. Notably, patients were twice as likely to be prescribed supplementation when the prescriber was a rheumatologist.
Discussion
This study showed that 77.0 % of women aged 50 and older who initiated an OP treatment had concomitant supplementation with calcium and/or vitamin D in the Rhône-Alpes area of France in 2010. Half of the study population had prescriptions for both calcium and vitamin D, and one quarter of women had vitamin D alone. Among women who were prescribed both vitamin D and calcium, those with a fixed-combination pack of bisphosphonates and vitamin D ± calcium represented only 7.6 %.
These results suggest that at least three quarters of women initiating an OP treatment were supplemented according to the current French guidelines for OP management [6]. This co-prescription rate seems to be higher than that reported in other studies. Several studies conducted in France between 2004 and 2006 reported data on calcium and/or vitamin D co-prescription with OP treatment ranging from 8.33 to 68 % [16, 17, 22]. In some recent European studies, co-prescription rates in postmenopausal women were estimated at 50 % in Italy and 34.1 % in the UK [23, 24]. Similarly, low usage of calcium and vitamin D with bisphosphonate therapy was found in Spain where 46 % of patients did not receive any supplementation with OP treatment [25]. A retrospective (from 1996 to 2003) study in Canada including women and men with pharmacy claims for OP treatment showed that 37.1 % of patients received vitamin D supplements [26]. All of these estimates are lower than those found in our study. Several reasons may explain the difference. The methodology used in most studies was very different from the present study. Many collected data through patient self-report which has the risk of recall bias, and less restrictive selection criteria were used including patients with both ongoing and new OP treatment. In addition, our study used recent data and therefore differences may be due to better adherence to OP guidelines over time. Another reason may be that supplementation is reimbursed in France and not in other countries. On the other hand, a French survey on general practice in OP management found that general practitioners intended to treat 90 % of their patients with a specific OP treatment in combination with vitamin D/calcium supplement and/or other dietary measures [27]. There might be a substantial proportion of initial prescriptions that are not filled after physician’s visits.
Several studies on determinants of adherence to osteoporosis treatment highlighted that poor adherence for OP treatment is very common notably due to the patient’s perception of the treatment and its motivation to take it. Prescription of calcium plus vitamin D seems to be one of the OP treatments with the lowest adherence rate [28]. Many patients fail to start or discontinue medications because of fear of possible adverse effects or belief that treatment is not needed [29, 30]. The issue of adherence cannot be addressed in our study which was limited to the analysis of filled initial prescriptions only. In our study, reimbursements for prescriptions were used as proxies for drug intake which could lead to overestimation of drug exposure. Moreover, calcium supplementation may be underestimated in our study because reimbursement data do not capture over the counter prescription, but given the high rates of co-prescription, this is unlikely. It is more likely that women not prescribed calcium supplements already had adequate dietary calcium intakes. An epidemiological French study that evaluated dietary calcium intake in postmenopausal women over 45 years of age found in the osteoporosis group that 32.7 % of women have increased their daily dietary calcium intake following their diagnosis, and 44.5 % reported either high daily calcium intake (≥1,500 mg/day) or taking dietary calcium supplements [31]. This observation is also consistent with current OP management recommendations that encourage the preferential correction with dietary intake [2, 6, 32]. Nevertheless, one quarter of the population followed in the present study did not have supplementation prescriptions concomitantly with their OP treatment.
Supplementation with calcium and vitamin D or vitamin D alone was higher when initial OP treatment was a bisphosphonate (81.7 %). The use of fixed-combination pack of bisphosphonates, vitamin D ± calcium may partly contribute to this increase. Bisphosphonates were the most frequently prescribed OP treatment in 60.4 % of included patients. This is consistent with other French studies with findings ranging from 50.3 to 79.8 % of OP treatments prescribed [16, 17, 33]. Alternatively, as women receiving bisphophonates were older than those women taking other types of drugs, they may have had lower calcium and/or vitamin D intakes that justify more often that they were supplemented.
GPs were the main prescribers of OP treatment. GPs supplemented around 75 % of their patients versus 87 % for rheumatologists and 67 % for gynecologists. In addition, being a rheumatologist was identified in our study as a factor associated with a higher probability of supplementation prescription. The distribution of prescribers for initial OP treatment was consistent with data from another study conducted in the Rhône-Alpes area reporting that, among women with ongoing OP treatment in 2006, most received it from a GP (79.0 %), fewer from a rheumatologist (11.6 %) or a gynecologist (7.1 %) [34]. In terms of prescription patterns, it was observed that more than 90 % of supplementation treatment was filled at the same date as initial OP treatment suggesting that physicians generally prescribed the first OP treatment and supplementation at the same time.
This study has a number of strengths. The ERASME database is an exhaustive description of health care utilization of the population covered by the Régime Général in the Rhône-Alpes area [35]. The ERASME database allows having inexpensive and rapidly representative and large-sized study samples for studying OP treatments [20, 36]. This study covered 2 years of reimbursement data which provided sufficient insight to evaluate first OP treatment prescriptions. Most importantly, this is a population-based sample that is less subject to bias, whereas other studies used survey data. Regarding the limitations of the study, it was based on claims obtained from a database generated primarily for administrative purposes. Also, medical services provided in long-stay hospital or in institutions for older people cannot be tracked in this database; this a priori exclusion may have introduced a selection bias and a lower representation of older women in the study sample.
Conclusion
The main purpose of this study was to provide valid data on calcium/vitamin D supplementation at initiation of OP treatment in a large population with detailed information on prescribers and nature of co-prescription. Overall, the rate of co-prescription was high for all physician specialties, although the study results should encourage general practitioners and gynecologists to prescribe supplementation with OP treatment more systematically.
References
Brewer L, Williams D, Moore A (2011) Current and future treatment options in osteoporosis. Eur J Clin Pharmacol 67:321–331
Kanis JA, Burlet N, Cooper C, Delmas PD, Reginster J-Y, Borgstrom F, Rizzoli R (2008) European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int 19:399–428
Rachner TD, Khosla S, Hofbauer LC (2011) Osteoporosis: now and the future. Lancet 377:1276–1287
Rizzoli R, Boonen S, Brandi ML, Burlet N, Delmas P, Reginster JY (2008) The role of calcium and vitamin D in the management of osteoporosis. Bone 42:246–249
Boonen S, Vanderschueren D, Haentjens P, Lips P (2006) Calcium and vitamin D in the prevention and treatment of osteoporosis—a clinical update. J Intern Med 259:539–552
Agence française de sécurité sanitaire des produits de santé (2006) Traitement médicamenteux de l’ostéoporose post-ménopausique. Recommandations de bonne pratique. Actualisation 2006. http://www.afssaps.fr/var/afssaps_site/storage/original/application/6c7b18b541509aa9f499484099d5f8e8.pdf. Accessed 1 Apr 2011
Haute Autorité de Santé (2006) Prévention, diagnostic et traitement de l’ostéoporose. http://www.has-sante.fr/portail/upload/docs/application/pdf/osteoporose_synthese.pdf. Accessed 1 Apr 2011
U.S. Preventive Services Task Force (2011) Screening for Osteoporosis: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med 154:356–364
Syed FA, Ng AC (2010) The pathophysiology of the aging skeleton. Curr Osteoporos Rep 8:235–240
Boonen S, Rizzoli R, Meunier PJ, Stone M, Nuki G, Syversen U, Lehtonen-Veromaa M, Lips P, Johnell O, Reginster J-Y (2004) The need for clinical guidance in the use of calcium and vitamin D in the management of osteoporosis: a consensus report. Osteoporos Int 15:511–519
Mehsen N, Paccou J, Confavreux CB, David C, Leboime A, Laroche M (2010) Management of patients with incident fractures during osteoporosis treatment. Joint Bone Spine 77:S133–S138
Cotté F-E, Mercier F, De Pouvourville G (2008) Relationship between compliance and persistence with osteoporosis medications and fracture risk in primary health care in France: a retrospective case–control analysis. Clin Ther 30:2410–2422
Confavreux CB, Paccou J, David C, Mehsen N, Leboime A, Thomas T (2010) Defining treatment failure in severe osteoporosis. Joint Bone Spine 77:S128–S132
Ringe JD, Fardellone P, Kruse H-P, Amling M, van der Geest SAP, Möller G (2009) Value of a new fixed-combination pack of bisphosphonate, calcium and vitamin D in the therapy of osteoporosis: results of two quantitative patient research studies. Drugs Aging 26:241–253
Ringe JD, van der Geest SA, Möller G (2006) Importance of calcium co-medication in bisphosphonate therapy of osteoporosis: an approach to improving correct intake and drug adherence. Drugs Aging 23:569–578
Blotman F, Cortet B, Hilliquin P, Avouac B, Allaert F-A, Pouchain D, Gaudin A-F, Cotté F-E, El Hasnaoui A (2007) Characterisation of patients with postmenopausal osteoporosis in French primary healthcare. Drugs Aging 24:603–614
Lespessailles E, Cotté F-E, Roux C, Fardellone P, Mercier F, Gaudin A-F (2009) Prevalence and features of osteoporosis in the French general population: the Instant study. Joint Bone Spine 76:394–400
Fender P, Weill A (2004) Epidemiology, public health and medical rates databases. Rev Epidemiol Sante Publique 52:113–117
Coeuret-Pellicer M, Zins M (2006) Les bases de données de l’assurance maladie. Rapport. http://www.rppc.fr/LesbasesdelaCNAM.pdf. Accessed 6 May 2011
Martin-Latry K, Bégaud B (2010) Pharmacoepidemiological research using French reimbursement databases: yes we can! Pharmacoepidemiol Drug Saf 19:256–265
Latry P, Molimard M, Bégaud B, Martin-Latry K (2010) How reimbursement databases can be used to support drug utilisation studies: example using the main French national health insurance system database. Eur J Clin Pharmacol 66:743–748
Fardellone P, Mann B (2007) Co-prescription of calcium and/or vitamin D with once weekly bisphosphonate therapy: findings from a French longitudinal patient database. Osteoporos Int 18(Suppl 1):358
Adami S, Giannini S, Bianchi G, Sinigaglia L, Di Munno O, Fiore CE, Minisola S, Rossini M (2009) Vitamin D status and response to treatment in post-menopausal osteoporosis. Osteoporos Int 20:239–244
Bayly JR, Hollands RD, Riordan-Jones SE, Yemm SJ, Brough-Williams I, Thatcher M, Woodman NM, Dixon T (2006) Prescribed vitamin D and calcium preparations in patients treated with bone remodelling agents in primary care: a report of a pilot study. Curr Med Res Opin 22:131–137
Quesada JM, Mann B (2007) Low usage of calcium and vitamin D with bisphosphonate therapy in post-menopausal osteoporotic women in France and in Spain. Osteoporos Int 18(Suppl 1):354
Hanley DA, Zhang Q, Meilleur M-C, Mavros P, Sen SS (2007) Prescriptions for vitamin D among patients taking antiresorptive agents in Canada. Curr Med Res Opin 23:1473–1480
Cortet B (2009) Postmenopausal osteoporosis: general practitioners’ application of the risk factors in the AFSSAPS guidelines. Survey of 2658 general practitioners. Presse Med 38:1213–1219
Sanfelix-Genovés J, Gil-Guillén VF, Orozco-Beltran D, Giner-Ruiz V, Pertusa-Martínez S, Reig-Moya B, Carratalá C (2009) Determinant factors of osteoporosis patients’ reported therapeutic adherence to calcium and/or vitamin D supplements: a cross-sectional, observational study of postmenopausal women. Drugs Aging 26:861–869
Papaioannou A, Kennedy CC, Dolovich L, Lau E, Adachi JD (2007) Patient adherence to osteoporosis medications: problems, consequences and management strategies. Drugs Aging 24:37–55
Rossini M, Bianchi G, Di Munno O, Giannini S, Minisola S, Sinigaglia L, Adami S (2006) Determinants of adherence to osteoporosis treatment in clinical practice. Osteoporos Int 17:914–921
Fardellone P, Cotté F-E, Roux C, Lespessailles E, Mercier F, Gaudin A-F (2010) Calcium intake and the risk of osteoporosis and fractures in French women. Joint Bone Spine 77:154–158
The North American Menopause Society (2010) Management of osteoporosis in postmenopausal women: 2010 position statement of The North American Menopause Society. Menopause 17:25–54
Cortet B, Blotman F, Debiais F, Huas D, Mercier F, Rousseaux C, Berger V, Gaudin A-F, Cotté F-E (2011) Management of osteoporosis and associated quality of life in post menopausal women. BMC Musculoskelet Disord 12:7
Huot L, Couris CM, Tainturier V, Jaglal S, Colin C, Schott A-M (2008) Trends in HRT and anti-osteoporosis medication prescribing in a European population after the WHI study. Osteoporos Int 19:1047–1054
Tuppin P, de Roquefeuil L, Weill A, Ricordeau P, Merlière Y (2010) French national health insurance information system and the permanent beneficiaries sample. Rev Epidemiol Sante Publique 58:286–290
Noize P, Bazin F, Dufouil C, Lechevallier-Michel N, Ancelin M-L, Dartigues J-F, Tzourio C, Moore N, Fourrier-Réglat A (2009) Comparison of health insurance claims and patient interviews in assessing drug use: data from the Three-City (3C) Study. Pharmacoepidemiol Drug Saf 18:310–319
Acknowledgments
The authors gratefully acknowledge the contributions of Dr. Roland Nublat and Dr. Gilbert Weill, medical officers at the French Health Insurance of the Rhône-Alpes area.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Reymondier, A., Caillet, P., Abbas-Chorfa, F. et al. MENOPOST - Calcium and vitamin D supplementation in postmenopausal osteoporosis treatment: a descriptive cohort study. Osteoporos Int 24, 559–566 (2013). https://doi.org/10.1007/s00198-012-1999-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-012-1999-5