Abstract
A European Union (EU) directive on vitamins and minerals used as ingredients of food supplements with a nutritional or physiological effect (2002/46/EC) was introduced in 2003. Its implications for the use of oral supplements of calcium and vitamin D in the prevention and treatment of osteoporosis were discussed at a meeting organized with the help of the World Health Organization (WHO) Collaborating Center for Public Health Aspects of Rheumatic Diseases (Liège, Belgium) and the support of the WHO Collaborating Center for Osteoporosis Prevention (Geneva, Switzerland). The following issues were addressed: Is osteoporosis a physiological or a medical condition? What is the evidence for the efficacy of calcium and vitamin D in the management of postmenopausal osteoporosis? What are the risks of self-management by patients in osteoporosis? From their discussions, the panel concluded that: (1) osteoporosis is a disease that requires continuing medical attention to ensure optimal therapeutic benefits; (2) when given in appropriate doses, calcium and vitamin D have been shown to be pharmacologically active (particularly in patients with dietary deficiencies), safe, and effective for the prevention and treatment of osteoporotic fractures; (3) calcium and vitamin D are an essential, but not sufficient, component of an integrated management strategy for the prevention and treatment of osteoporosis in patients with dietary insufficiencies, although maximal benefit in terms of fracture prevention requires the addition of antiresorptive therapy; (4) calcium and vitamin D are a cost-effective medication in the prevention and treatment of osteoporosis; (5) it is apparent that awareness of the efficacy of calcium and vitamin D in osteoporosis is still low and further work needs to be done to increase awareness among physicians, patients, and women at risk; and (6) in order that calcium and vitamin D continues to be manufactured to Good Manufacturing Practice standards and physicians and other health care professionals continue to provide guidance for the optimal use of these agents, they should continue to be classified as medicinal products.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
European Union (EU) Directive 2002/46/EC on vitamins and minerals used as ingredients of food supplements with a nutritional or physiological effect [1] was introduced in 2003. An international expert panel discussed its implications for the use of oral supplements of calcium and vitamin D in the prevention and treatment of osteoporosis at a meeting in Barcelona on 10 November 2002. This meeting was organized with the help of the World Health Organization (WHO) Collaborating Center for Public Health Aspects of Rheumatic Diseases (Liège, Belgium) and with the support of the WHO Collaborating Center for Osteoporosis Prevention (Geneva, Switzerland). The meeting addressed the following issues:
-
1.
Is osteoporosis a physiological or a medical condition?
-
2.
What is the evidence for the efficacy of calcium and vitamin D in the management of postmenopausal osteoporosis?
-
3.
What are the risks of self-management by patients with or at risk of osteoporosis?
This report provides a summary of the discussion and consensus conclusions from the meeting.
Osteoporosis: a prevalent and serious disease
Osteoporosis is the major cause of fractures in middle-aged and elderly men and women and is a growing health care problem in Europe and the rest of the world. For Caucasians, the lifetime risk of an osteoporotic fracture at 50 years of age has been estimated to be approximately 40% for women and 13% for men [2]. These figures, however, are based on the assumption that life expectancy will remain stable; they are therefore likely to underestimate future risks. Estimates based on data from Malmö (Sweden) that do take account of future mortality trends are 47% for women and 22% for men [3]. Indeed, these latter estimates appear to be in agreement with more recent prospective data on vertebral fracture rates from the European Prospective Osteoporosis Study (EPOS), which were higher than expected (40% for women and 20% for men at age 80) [4].
Osteoporotic fractures can have devastating physical, medical, psychological, and social consequences for patients. Vertebral fractures can lead to back pain, loss of height, deformity, immobility, and increased number of bed days, and even reduced pulmonary function [5, 6, 7, 8, 9]. Their impact on quality of life can be profound as a result of loss of self-esteem, distorted body image, and depression [5, 8, 10, 11, 12, 13, 14, 15]. Vertebral fractures also significantly impact on activities of daily living [16, 17]. Hip fractures are invariably associated with chronic pain, reduced mobility, disability, and an increasing degree of dependence [18]. After sustaining a hip fracture, 10–20% of formerly community-dwelling patients require long-term nursing care [19, 20, 21, 22, 23], with the rate of nursing home admission rising with age [20, 22].
Both hip and vertebral fractures are also associated with excess mortality [24, 25, 26, 27]. In the European Prospective Osteoporosis Study, risk ratios (adjusted for age) for mortality associated with vertebral fractures were 1.9 and 1.3, respectively [27]. Data from Australia show hip fractures were associated with a 2.18 and 3.17 relative increase in mortality in women and men, respectively, while corresponding ratios for vertebral fractures were 1.66 and 2.38 [24]. A 50-year-old woman has a 2.8% risk of death related to hip fracture during her remaining lifetime, equivalent to her risk of death from breast cancer and four times higher than that from endometrial cancer [28]. Although mortality rates are higher in older patients, deaths in younger patients (aged <70 years) contribute substantially to the excess mortality and short survival associated with osteoporotic fractures [24].
The combination of the disease’s serious morbidity with its high prevalence means that osteoporosis has a major impact on health care costs. A study in Switzerland showed that the annual costs of hospitalizations (in terms of duration of stay) for osteoporotic fractures were greater than those for myocardial infarction, stroke, and breast cancer, and only slightly lower than for chronic obstructive pulmonary disease (Fig. 1) [29]. For women, the costs associated with osteoporosis were higher than for all these diseases. Across the European Community, the total annual direct hospital costs for the nearly 500,000 patients who sustain a hip fracture each year are estimated to be 4.8 billion euros [30]. Costs for medical care after hospital discharge and in particular nursing home care are also substantial [21]. Furthermore, health care expenditure is likely to rise dramatically unless policies directed at preventing the disease are implemented. Although osteoporosis is currently underdiagnosed and undertreated in women [31] and men [23], techniques for diagnosing osteoporosis are well established, and effective therapies for its prevention and treatment have been developed [32, 33]. The consequences of osteoporosis are therefore avoidable and we regard them as unacceptable.
Comparison of hospital bed utilization due to consequences of osteoporosis at any skeletal site (33,595 women and 29,574 men) compared with other common acute diseases (adapted with permission from data in [23])
Calcium and vitamin D supplementation as an essential component of management strategies for the prevention and treatment of osteoporosis
Calcium and vitamin D are crucial for bone health throughout life [34, 35, 36, 37]. Calcium intake is one of the main determinants for the development of peak bone mass during adolescence and also slows the subsequent age-related bone loss [34, 35, 36, 37]. In the presence of vitamin D deficiency, calcium absorption is impaired and there is a compensatory increase in parathyroid hormone (PTH) levels, with a consequent stimulation of bone resorption and accelerated bone loss [38, 39, 40, 41, 42, 43, 44]. Vitamin D status is usually assessed by measurement of the serum concentration of 25-hydroxyvitamin D, the main circulating metabolite. While severe vitamin D deficiency causes osteomalacia, moderate vitamin D deficiency is associated with lower calcium absorption, secondary hyperparathyroidism, high bone turnover, and bone loss [43]. The following stages have been proposed: severe vitamin D deficiency associated with osteomalacia, serum 25-hydroxyvitamin D <12.5 nmol/l (5 ng/ml); moderate vitamin D deficiency associated with secondary hyperparathyroidism and high bone turnover, serum 25-hydroxyvitamin D 12.5–25 nmol/l (5–10 ng/ml); mild vitamin D deficiency or insufficiency associated with small elevations of serum PTH and probably bone loss in the long term, serum 25-hydroxyvitamin D 25–50 nmol/l (10–20 ng/ml). However, there is no consensus on the breakpoint where insufficiency begins. Some studies suggest that the serum 25-hydroxyvitamin D level below which serum PTH starts to rise could be 80 nmol/l (32 ng/ml) [45, 46], while others situate this point at a serum 25-hydroxyvitamin D of 50 nmol/l [47, 48]. Anyway, the required serum 25-hydroxyvitamin D to prevent secondary hyperparathyroidism is higher than previously anticipated. Moreover, there is evidence that the intestinal absorption of calcium in response to vitamin D declines with age [49]. Both calcium and vitamin D deficiency or insufficiency are therefore important risk factors for osteoporosis and osteoporotic fractures [38, 50, 51, 52]. Furthermore, it is more straightforward to correct calcium and vitamin D insufficiency first, before addressing the other risk factors for osteoporosis. The elderly are at risk of vitamin D insufficiency, because they are less mobile and therefore have less sunshine exposure. The capacity of the skin to produce vitamin D3 decreases with age. Other risk groups include patients with skin conditions who have been advised to minimize sun exposure and immigrants whose style of dress tends to result in low exposure of the skin to sunlight. In addition, darker skin is a risk factor for decreased production of pre-vitamin D3.
Optimal intake of calcium and vitamin D
There is no universal consensus on optimal daily calcium intake. The Food and Nutrition Board of the Institute of Medicine, US National Academy of Sciences, states that an adequate intake of calcium for men and women aged over 50 years is 1,200 mg/day, while for younger adults 1,000 mg/day is an adequate intake [53]. Recommendations within Europe are lower, at 700–800 mg/day for all ages (800 mg for women aged 50–65 years) [54]. The European Commission has set the tolerable upper intake level for calcium intake from all sources in adults at 2,500 mg/day [55].
Vitamin D is derived from cutaneous synthesis in the presence of ultraviolet light as well as from the diet; the relative importance of each being dependent on race, geographic location, age, and social conditions such as housing and lifestyle. For example, people living in urban centers or institutions are exposed to suboptimal levels of sunlight since ultraviolet light is blocked by air pollution, clothes, tall buildings, indoor dwelling, and sunscreens. These factors reduce the skin’s ability to synthesize vitamin D [56]. European guidelines for dietary vitamin D intake are 0–400 IU daily for adults of both sexes up to age 65 years and 400 IU daily for those aged 65 years and above [54]. Adequate intake in the United States has been defined as 400 IU/day for adults from 51 to 70 years and 600 IU/day in elderly over 70 years [57]. A dose-finding study in institutionalized elderly people showed that serum 25-hydroxyvitamin D increased from 24 to 68 nmol/l with vitamin D3 400 IU/day and from 24 to 78 nmol/l with 800 IU/day [58]. In a large prevention study with vitamin D3 400 IU/day, serum 25-hydroxyvitamin D rose to 54 nmol/l in an independent elderly population and to 62 nmol/l in an institutionalized elderly population. This difference is probably caused by compliance being better in an institution [59, 60]. Different opinions exist as to whether the dose should be adapted to correct for noncompliance. However, safety is not a matter of concern. Vitamin D3 supplementation of 4,000 IU/day (100 µg/day) resulted in a serum 25-hydroxyvitamin D of about 100 nmol/l after 5 months without change of serum calcium level or calcium excretion [61]. The European Commission has set the tolerable upper intake level for adults at 50 µg/day (2,000 IU/day) [62].
Many European adults of both sexes have suboptimal dietary intake of both calcium and vitamin D [43, 45]. In a sample of urban-dwelling French men (aged 45–65 years) and women (aged 35–60 years), nearly half had a daily calcium intake below the European recommendations, while the prevalence of vitamin D deficiency (defined as a serum 25-hydroxyvitamin D level, as determined by radioimmunoassay [RIA], <12 ng/ml) was 14% [45]. The elderly, who often have low dietary intakes, are much more likely to have insufficient dietary calcium and vitamin D intakes. Mean calcium intake in a sample of elderly community-dwelling French women was 569 mg daily and 39% had vitamin D deficiency (defined as serum 25-hydroxyvitamin D level, as determined by RIA, <12 ng/ml) [63]. Similar findings have been reported in other studies, even in the absence of confounding diseases [40]. As vitamin D is needed to maintain calcium homeostasis, calcium and vitamin D insufficiency commonly coexist. For example, in a sample of elderly institutionalized women, 66% had an inadequate intake of both calcium and vitamin D (defined as <800 mg daily calcium and a serum 25-hydroxyvitamin D level [by RIA] <12 ng/ml) [64]. This suggests a rationale for combined calcium and vitamin D supplementation to improve bone health in individuals with dietary insufficiencies.
Calcium and vitamin D supplementation reduces the risk of fractures
The treatment of elderly institutionalized women with combined calcium and vitamin D supplements has been shown to reduce the risk of nonvertebral fractures in a large, multicenter, randomized, double-blind, placebo-controlled trial [65, 66, 67]. All the women in this study (n=3,270) had inadequate dietary calcium intakes at baseline (<800 mg daily) and 44% had vitamin D deficiency (serum 25-hydroxyvitamin D level [by RIA] <12 ng/ml). When corrected for assay differences by interlaboratory comparison, the percentage of vitamin D deficient elderly was much higher [43, 68].
The supplement group received 1,200 mg of calcium and 800 IU of vitamin D3 daily. At 36 months, the intention-to-treat analysis showed that supplementation reduced the incidence of hip fractures by 23% and of all nonvertebral fractures by 17.2% [66]. When the analysis was restricted to patients who actually received randomized therapy, the reduction in risk was 29% and 24%, respectively. The benefit of supplementation emerged within 12 months (Fig. 2) [65, 67]. Intervention prevented a total of 46 hip fractures and an additional 21 nonvertebral fractures (number needed to treat [NNT] to prevent any vertebral or nonvertebral fracture = 41). The reduction in hip fracture risk with supplementation was consistent with the changes in bone mineral density (BMD) reported at 18 months; the BMD of the proximal femur increased by 2.7% in the supplement group whereas in the placebo group there was a decline of 4.6%. The absence of bone loss in the supplemented group is supported by improvements in the indexes of secondary hyperparathyroidism. Most of the effect of supplementation was seen within 6 months, when mean PTH levels had decreased by 35% compared with baseline and mean serum 25-hydroxyvitamin D levels had increased by 150%. Furthermore, those women who had elevated PTH levels and low serum 25-hydroxyvitamin D levels at baseline had normal values at the end of the study, within the range 11–55 pg/ml for PTH, and 15–50 ng/ml for serum 25-hydroxyvitamin D [65, 66].
Reduction in hip fractures achieved with calcium and vitamin D supplementation (reproduced with permission from [54])
In a randomized study involving 389 subjects (aged 65 years and over), daily supplementation with calcium 500 mg and vitamin D 700 IU more than halved the incidence of nonvertebral fractures; of the 37 fractures sustained by the study population, 11 were in the calcium and vitamin D group compared with 26 in the placebo group (p=0.02) [69]. Other studies have been undertaken using higher doses of vitamin D at longer intervals (e.g., 6 months). For example, the recent study of Trivedi and colleagues [70] showed that vitamin D3 alone, 100,000 IU every 4 months, was safe and effective in decreasing the incidence of osteoporotic fractures. This was a randomized, double-blind, placebo-controlled trial in 2,686 people aged 65–85 years, living in the United Kingdom in the general community. After 5 years, 147 men and women had fractures in common osteoporotic sites; the relative risk in the vitamin D group compared with the placebo group was 0.67 (95% CI, 0.48 to 0.93; p=0.02) for first hip, wrist or forearm, or vertebral fractures [70]. However, vitamin D regimens such as this involving intermittent administration of relatively large doses (albeit physiological if used correctly) should only be available on medical prescription due to the danger of vitamin D intoxication if the tablets are taken more frequently than intended.
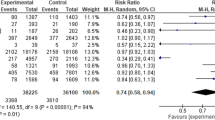
There are, however, studies with calcium, vitamin D and/or calcium, and vitamin D that have not replicated the above results. For example, Meyer and colleagues reported that intervention with 10 μg daily of vitamin D3 failed to prevent either hip or vertebral fractures over a 2-year period in a nursing home population [71]. Likewise, vitamin D (400 IU/day) given without calcium to an elderly community-dwelling population in The Netherlands did not reduce the risk of hip fractures [59]. The inconsistencies between the results of different studies are probably due to differences in the type of supplement used, the addition of a calcium supplement, the characteristics of the patients included in the studies such as degree of vitamin D deficiency at baseline, study design, and/or the study endpoints. Recent meta-analyses confirm the value of calcium and vitamin D supplementation in the prevention of postmenopausal osteoporosis, although such analyses can be criticised on the basis that they do not take into account baseline calcium and vitamin D status or the multiplicity of study designs. Calcium supplements alone were shown to have a small but definite effect on BMD and a trend toward reducing vertebral fractures [72], while the meta-analysis of trials of vitamin D supplementation demonstrated some additional effect of calcium on the reduction of nonvertebral fractures [73]. A Cochrane review concluded that calcium and vitamin D does reduce the fracture risk in some older people, although the efficacy of vitamin D alone is unclear [74]. It must be noted, however, that the large randomized controlled study of Trivedi and colleagues [70] described previously, which reported a positive effect of vitamin D alone, has been published since this meta-analysis [73] and the Cochrane review [74].
Although the effects of calcium and vitamin D in fracture prevention are generally attributed to increases in BMD, it has also been hypothesized that the effect of supplementation on calcium homeostasis might increase muscular strength, thereby reducing the risk of falls. In a study designed to test this hypothesis, involving a group of 122 elderly institutionalized women, 50% of whom had vitamin D insufficiency (serum 25-hydroxyvitamin D below 12 ng/ml) at study entry, musculoskeletal function was shown to improve significantly (p<0.01) after 3 months’ therapy with calcium and vitamin D; there was no significant improvement in women treated with calcium alone over the same time period. The incidence of falls in the women who received calcium and vitamin D was reduced by 49% (p<0.01) after 3 months, with recurrent fallers benefiting the most, whereas there was no reduction in women given calcium only [75]. Likewise, Pfeifer and colleagues observed a reduction in body sway and a reduction in falls with short-term calcium and vitamin D supplementation as compared with calcium alone in a sample of 148 elderly women [76].
On balance, there is a strong case that calcium and vitamin D supplementation is beneficial in the prevention of osteoporotic fractures in those at risk, i.e., elderly individuals with calcium and/or vitamin D insufficiency. Given the high economic burden of osteoporotic fractures and the low cost of calcium and vitamin D products, screening, and follow-up, treatment is also extremely cost-effective, as shown recently by Lilliu and colleagues [77]. These authors assessed the cost implications of a preventative treatment strategy of osteoporotic fractures with combined calcium 1,200 mg/day and vitamin D 800 IU/day for institutionalized elderly women, applying recently published unit cost data to the results of the prospective placebo-controlled clinical trial of Chapuy and colleagues described earlier [65, 66]. Across the seven European countries involved in the Chapuy trial, the total costs in the placebo group were higher than in the supplementation group, resulting in a net benefit of 79,000–711,000 euros per 1,000 women [77]. The authors note that their analysis may underestimate the net benefits of calcium and vitamin D in this setting, as treatment is also effective in decreasing the incidence of nonvertebral fractures.
Calcium and vitamin D should therefore be considered an essential component of an integrated management strategy for the prevention and treatment of osteoporosis, although maximal benefit will generally be derived from combination therapy with an antiresorptive agent. The important role of calcium and vitamin D in the management of osteoporosis is recognized by the European regulatory authorities who require that subjects in both arms of clinical trials of new drugs for osteoporosis have adequate intakes of calcium and vitamin D, which if necessary should be achieved by appropriate supplementation [78].
Calcium and vitamin D therapy needs clinical guidance
It is now widely understood that osteoporosis is a serious disease that requires medical assessment and management. Calcium and vitamin D have been shown to be effective medications for reducing fracture risk when prescribed in appropriate doses in randomized controlled trials of therapy. The panel held the unanimous view that clinical supervision of calcium and vitamin D therapy for the management of osteoporosis was necessary to ensure optimum efficacy and safety. Calcium and vitamin D for the prevention and treatment of osteoporosis should therefore continue to be a medicinal product under the European Directive 2001/83/EC.
Implications of self-management of calcium and vitamin D therapy
Awareness of personal risk of osteoporosis among women is extremely low. A survey conducted in 1999 by the International Osteoporosis Foundation (IOF) [79] in Europe and elsewhere showed that although most women were aware that osteoporosis is a serious disease, 80% of those surveyed did not believe that they personally were at risk (Fig. 3). Men are less aware than women that osteoporosis could affect them [80]. If the decision to initiate calcium and vitamin D therapy were left to individuals themselves, it seems likely that they would not receive appropriate treatment. Compliance with long-term therapy for osteoporosis, which is frequently poor, is likely to be better when a physician prescribes the medication and when physicians or other health care professionals follow up patients. The panel were also of the opinion that patients were more likely to continue long-term treatment with appropriate doses of calcium and vitamin D if they received financial reimbursement, as would be the case if these agents continued to be classified as medicinal products but not if they were reclassified as food supplements. The medical need for good compliance in achieving optimal outcome in osteoporosis is highlighted by the data of Dawson-Hughes and colleagues [81] showing that, in both men and women, calcium and vitamin D supplementation had no lasting benefits on BMD at the femoral neck 2 years after treatment withdrawal.
The IOF survey also demonstrated that the awareness of the disease, its diagnosis, and treatment is low among physicians, with only one third discussing the disease with their patients. This finding is reinforced by studies in the literature (e.g., [82]). Self-management could potentially hold back the development of new medical educational initiatives that are clearly needed to improve this situation.
Calcium and vitamin D as combination therapy
At the present time, antiresorptives such as the bisphosphonates are useful drugs in the reduction of fracture risk [83]. Most of the trials that have demonstrated a decrease in fracture risk with antiresorptives have included patients receiving calcium and vitamin D supplements. There is evidence that these agents are less effective in the presence of low calcium and vitamin D levels, i.e., their effects are blunted [84, 85, 86, 87]. In the largest and most recent of these studies [87], involving a group of hormone replacement therapy (HRT) users (n=392) participating in the Finnish OSTPRE-study, HRT prevented femoral bone loss over the 5-year study period only among the women with the highest calcium intake (>927 mg/day). When the same authors analyzed studies of calcitonin, they found that lumbar spine BMD increased by 2.1% per year with calcitonin plus calcium supplementation compared with a decrease of 0.2% per year with calcitonin alone [86]. Likewise, in a study comparing the effects of etidronate alone and etidronate plus a vitamin D supplement, significant differences in BMD favoring the supplement group were apparent at both the lumbar spine (5.2% vs 2.7%; p=0.036) and femoral neck (2.0% vs –0.4%; p=0.046) at 1 year [85]. Similar results were observed when the effects of etidronate were compared in vitamin D deficient (serum 25-hydroxyvitamin D levels <40 nmol/l) and nondeficient postmenopausal women with osteopenia [84]. Therefore, for maximum benefits to be achieved, most patients with osteoporosis should receive both calcium and vitamin D and an antiresorptive agent.
Good Manufacturing Practice (GMP) is important for product quality
As pharmaceutical products, calcium and vitamin D supplements are manufactured under Good Manufacturing Practice (GMP) guidelines. Nutritional supplements are not subjected to such rigorous manufacturing standards and their quality and batch-to-batch consistency may vary [88]. Nutritional supplements are not subjected to the rigorous requirement to demonstrate bioequivalence that is demanded of all new and generic drugs. It is well recognized that the extent of drug absorption can be influenced by the pharmaceutical formulation, and this has recently been demonstrated to apply to calcium carbonate products [89]. Of eight commercial products of calcium carbonate available in the United States (where calcium supplements are regulated as dietary supplements under food law), only two exhibited absorbability comparable to that of plain calcium carbonate. The remaining six products were substantially (by up to approximately 50%) less bioavailable.
Conclusions
In summary, we conclude that osteoporosis is a disease that requires continuing medical attention to ensure optimal therapeutic benefits. Calcium and vitamin D, when given in appropriate doses, have been shown to be pharmacologically active (particularly in patients with dietary deficiencies), safe, and effective for the prevention and treatment of osteoporotic fractures. Indeed, calcium and vitamin D are a first-line medication in the prevention and treatment of osteoporosis, although most patients will derive further benefit in terms of fracture prevention from the addition of an antiresorptive agent. The use of calcium and vitamin D in the prevention and treatment of osteoporosis is cost-effective. It is apparent that awareness of the efficacy of calcium and vitamin D in osteoporosis is still low, and further work needs to be done to increase awareness among physicians, patients, and people at risk. In order that calcium and vitamin D continues to be manufactured to GMP standards and that physicians and other health care professionals continue to provide guidance for the optimal use of these agents, they should continue to be classified as medicinal products (2001/83/EC) after implementation of the European Union directive for vitamins and minerals with nutritional or physical effects that are used as ingredients of food supplements (2002/46/EC).
Summary of conclusions
-
1.
Osteoporosis is a disease that requires continuing medical supervision to ensure its successful management.
-
2.
Calcium and vitamin D have been shown to be pharmacologically active (particularly in patients with dietary deficiencies), safe, and effective for the prevention and treatment of osteoporotic fractures in the elderly when given in appropriate doses.
-
3.
Calcium and vitamin D is an essential, but not sufficient, component of an integrated strategy for the prevention and treatment of osteoporosis in patients with dietary insufficiencies; most patients will derive further benefit in terms of fracture prevention from the addition of an antiresorptive agent.
-
4.
Calcium and vitamin D is a cost-effective medication in the prevention and treatment of osteoporosis.
-
5.
Awareness of the efficacy of calcium and vitamin D is still low, and further work needs to be done to increase awareness among physicians, patients, and people at risk.
-
6.
In order that calcium and vitamin D continues to be manufactured to GMP standards and that physicians and other health care professionals continue to provide guidance for the optimal use of these agents, they should continue to be classified as medicinal products under the European Directive 2001/83/EC.
References
European Commission (2002) Directive 2002/46/EC of the European parliament and of the Council. Official Journal of the European Communities. L183:51–57
Melton LJ, Chrischilles EA, Cooper C et al (1992) Perspective: how many women have osteoporosis? J Bone Miner Res 7:1005–1010
Kanis JA, Johnell O, Oden A et al (2000) Long-term risk of osteoporotic fracture in Malmö. Osteoporos Int 11:669–674
Ismail AA, Cooper C, Felsenberg D et al (1999) Number and type of vertebral deformities: epidemiological characteristics and relation to back pain and height loss. European Vertebral Osteoporosis Study Group. Osteoporos Int 9:206–213
Gold DT (1996) The clinical impact of vertebral fractures: quality of life in women with osteoporosis. Bone 18[Suppl 3]:185S-189S
Schlaich C, Minne HW, Brucker T et al (1998) Reduced pulmonary function in patients with spinal osteoporotic fractures. Osteoporos Int 8:261–267
Nevitt MC, Ettinger B, Black DM et al (1998) The association of radiographically detected vertebral fractures with back pain and function: a prospective study. Ann Intern Med 128:793–800
Lips P, Cooper C, Agnusdei D et al (1999) Quality of life in patients with vertebral fractures: validation of the Quality of Life Questionnaire for the European Foundation for Osteoporosis (QUALEFFO). Osteoporos Int 10:150–160
Pluijm SMF, Dik MG, Jonker C et al (2002) Effects of gender and age on the association of apolipoprotein E ε4 with bone mineral density, bone turnover and the risk of fractures in older people. Osteoporos Int 13:701–709
Hall SE, Criddle RA, Comito TL et al (1999) A case-control study of quality of life and functional impairment in women with long-standing vertebral osteoporotic fracture. Osteoporos Int 9:508–515
Gold DT (2001) The nonskeletal consequences of osteoporotic fractures: psychologic and social outcomes. Rheum Dis Clin North Am 27:255–262
Robbins J, Hirsch C, Whitmer R et al (2001) The association of bone mineral density and depression in an older population. J Am Geriatr Soc 49:732–736
Lyles KW (2001) Osteoporosis and depression: shedding more light upon a complex relationship. J Am Geriatr Soc 49:827–828
Tosteson ANA, Gabriel SE, Grove MR et al (2001) Impact of hip and vertebral fractures on quality-adjusted life years. Osteoporos Int 12:1042–1049
Oleksik A, Lips P, Dawson A et al (2000) Health-related quality of life in postmenopausal women with low BMD with or without prevalent vertebral fractures. J Bone Miner Res 15:1384–1392
Hall SE, Criddle RA, Comito TL, Prince RL (1999) A case-control study of quality of life and functional impairment in women with long-standing vertebral osteoporotic fracture. Osteoporos Int 9:508–515
Adachi JD, Ioannidis G, Olszynski WP et al (2002) The impact of incident vertebral and non-vertebral fractures on health related quality of life in postmenopausal women. BMC Musculoskelet Disord 3:11–18
Keene GS, Parker MJ, Pryor GA (1993) Mortality and morbidity after hip fractures. BMJ 307:1248–1250
Schürch MA, Rizzoli R, Mermillod B et al (1996) A prospective study of socioeconomic aspects of fracture of the proximal femur. J Bone Miner Res 11:1935–1942
Reginster J-Y, Gillet P, Sedrine WB et al (1999) Direct costs of hip fractures in patients over 60 years of age in Belgium. Pharmacoeconomics 15:507–514
Autier P, Haentjens P, Bentin J et al (2000) Costs induced by hip fractures: a prospective controlled study in Belgium. Belgian Hip Fracture Study Group. Osteoporos Int 11:373–380
Cree M, Soskolne CL, Belseck E et al (2000) Mortality and institutionalization following hip fracture. J Am Geriatr Soc 48:283–288
Kiebzak GM, Beinart GA, Perser K et al (2002) Undertreatment of osteoporosis in men with hip fracture. Arch Intern Med 162:2217–2222
Center JR, Nguyen TV, Schneider D et al (1999) Mortality after all major types of osteoporotic fracture in men and women: an observational study. Lancet 353:878–882
Trombetti A, Herrmann F, Hoffmeyer P et al (2002) Survival and potential years of life lost after hip fracture in men and age-matched women. Osteoporos Int 13:731–737
Cauley JA, Thompson DE, Ensrud KC et al (2000) Risk of mortality following clinical fractures. Osteoporos Int 11:556–561
Ismail AA, O’Neill TW, Cooper C et al (1998) Mortality associated with vertebral deformity in men and women; results from the European Prospective Osteoporosis Study (EPOS). Osteoporos Int 8:291–297
Cummings SR, Black DM, Rubin SM (1989) Lifetime risks of hip, Colles’, or vertebral fracture and coronary heart disease among white postmenopausal women. Arch Intern Med 149:2445–2448
Lippuner K, von Overbeck J, Perrelet R et al (1997) Incidence and direct medical costs of hospitalizations due to osteoporotic fractures in Switzerland. Osteoporos Int 7:414–425
International Osteoporosis Foundation (1999) Survey by Helmut Minne, November 1999. http://www.osteofound.org. Cited 3 October 2003
Colditz GA, Manson JE, Hankinson SE (1997) The Nurse’s Health Study: 20-year contribution to the understanding of health among women. J Womens Health 6:49–62
The Osteoporosis Methodology Group and the Osteoporosis Research Advisory Group (2002) Meta-analyses of therapies for postmenopausal osteoporosis. Endocr Rev 23:496–507
Häuselmann HJ, Rizzoli R (2003) A comprehensive review of treatments for postmenopausal osteoporosis. Osteoporos Int 14:2–12
Heaney RP (1993) Nutritional factors in osteoporosis. Ann Rev Nutr 13:287–316
Välimäki MJ, Kärkkäinen M, Lamberg-Allardt C et al (1994) Exercise, smoking and calcium intake during adolescence and early adulthood as determinants of peak bone mass. BMJ 309:230–235
Bonjour JP, Carrie AL, Ferrari S et al (1997) Calcium-enriched foods and bone mass growth in prepubertal girls: a randomized, double-blind, placebo-controlled trial. J Clin Invest 99:1287–1294
Lehtonen-Veromaa MKM, Möttönen TT, Nuotio IO et al (2002) Vitamin D and attainment of peak bone mass among peripubertal Finnish girls: a 3-year prospective study. Am J Clin Nutr 76:1446–1453
Boonen S, Vanderschueren D, Cheng XG et al (1997) Age-related (type II) femoral neck osteoporosis in men: biochemical evidence for both hypovitaminosis D- and androgen deficiency-induced bone resorption. J Bone Miner Res 12:2119–2126
Boonen S, Aerssens J, Dequeker J (1996) Age-related endocrine deficiencies and fractures of the proximal femur, II: implications of vitamin D deficiency in the elderly. J Endocrinol 149:13–17
Boonen S, Lesaffre E, Dequeker J et al (1996) Relationship between baseline insulin-like growth factor-I and femoral bone density in women aged over 70 years: potential implications for the prevention of age-related bone loss. J Am Geriatr Soc 44:1301–1306
Boonen S, Broos P, Verbeke G et al (1997) Calciotrophic hormones and markers of bone remodeling in age-related (type II) femoral neck osteoporosis: alterations consistent with secondary hyperparathyroidism-induced bone resorption. J Gerontol 52A:M286–M293
Reginster J-Y, Deroisy R, Pirenne H et al (1999) High prevalence of low femoral bone mineral density in elderly women living in nursing homes or community-dwelling: a plausible role of increased parathyroid hormone secretion. Osteoporos Int 9:121–128
Lips P (2001) Vitamin D deficiency and secondary hyperparathyroidism in the elderly: consequences for bone loss and fractures and therapeutic implications. Endocr Rev 22:477–501
McKenna MJ, Freaney R (1998) Secondary hyperparathyroidism in the elderly: means to defining hypovitaminosis D. Osteoporos Int 8[Suppl 2]:S3–S6
Chapuy MC, Preziosi P, Maamer M et al (1997) Prevalence of vitamin D insufficiency in an adult normal population. Osteoporos Int 7:439–443
Thomas MK, Lloyd-Jones DM, Thadhani RI et al (1998) Hypovitaminosis D in medical inpatients. N Engl J Med 338:777–783
Malabanan AO, Veronikis IE, Holick MF (1998) Redefining vitamin D insufficiency. Lancet 351:805–806
Lips P, Duong T, Oleksik AM et al for the Multiple Outcomes of Raloxifene Evaluation Study Group (2001) A global study of vitamin D status and parathyroid function in postmenopausal women with osteoporosis: baseline data from the multiple outcomes of raloxifene evaluation clinical trial. J Clin Endocrinol Metab 86:1212–1221
Pattanaungkul S, Riggs BL, Yergey AL et al (2000) Relationship of intestinal calcium absorption to 1,25-dihydroxyvitamin D[1,25(OH)2D] levels in young versus elderly women: evidence for age-related intestinal resistance to 1,25(OH)2D action. J Clin Endocrinol Metab 85:4023–4027
Villareal DT, Civitelli R, Chines A et al (1991) Subclinical vitamin D deficiency in postmenopausal women with low vertebral bone mass. J Clin Endocrinol Metab 72:628–634
Thiébaud D, Burckhardt P, Costanza M et al (1997) Importance of albumin, 25(OH)-vitamin D and IGFBP-3 as risk factors in elderly women and men with hip fracture. Osteoporos Int 7:457–462
LeBoff MS, Kohlmeier L, Hurwitz S et al (1999) Occult vitamin D deficiency in postmenopausal US women with acute hip fracture. JAMA 281:1505–1511
Yates AA, Schlicker SA, Suitor CW (1998) Dietary Reference Intakes: the new basis for recommendations for calcium and related nutrients, B vitamins, and choline. J Am Diet Assoc 98:699–706
European Commission (1998) Report on osteoporosis in the European Community: action on prevention. Luxembourg Office for Official Publications of the European Communities, p 112
European Commission Scientific Committee on Food (2002) Opinion of the Scientific Committee on Food on the tolerable upper intake level of calcium. European Commission, Brussels
Hochberg Z, Bereket A, Davenport M et al (2002) Consensus development for the supplementation of vitamin D in childhood and adolescence. Horm Res 5839–5851
Holick MF (1998) Vitamin D requirements for humans of all ages: new increased requirements for women and men 50 years and older. Osteoporos Int 8[Suppl 2]:S24–S29
Lips P, Wiersinga A, Ginkel van FC et al (1988) The effect of vitamin D supplementation on vitamin D status and parathyroid function in elderly subjects. J Clin Endocrinol Metab 67:644–650
Lips P, Graafmans WC, Ooms ME et al (1996) Vitamin D supplementation and fracture incidence in elderly persons: a randomized, placebo-controlled clinical trial. Ann Intern Med 124:400–406
Ooms ME, Roos JC, Bezemer PD et al (1995) Prevention of bone loss by vitamin D supplementation in elderly women: a randomized double-blind trial. J Clin Endocrin Metab 80:1052–1058
Vieth R, Chan P-CR, MacFarlane GD (2001) Efficacy and safety of vitamin D3 intake exceeding the lowest observed adverse effect level. Am J Clin Nutr 73:288–294
European Commission Scientific Committee on Food (2002) Opinion of the Scientific Committee on Food on the tolerable upper intake level of vitamin D. European Commission, Brussels
Chapuy MC, Schott AM, Garnero P et al (1996) Healthy elderly French women living at home have secondary hyperparathyroidism and high bone turnover in winter. EPIDOS Study Group. J Clin Endocrinol Metab 81:1129–1133
Chapuy MC, Pamphile R, Paris E et al (2002) Combined calcium and vitamin D3 supplementation in elderly women: confirmation of reversal of secondary hyperparathyroidism and hip fracture risk: the Decalyos II Study. Osteoporos Int 13:257–264
Chapuy MC, Arlot ME, Duboeuf F et al (1992) Vitamin D3 and calcium to prevent hip fractures in elderly women. N Engl J Med 327:1637–1642
Chapuy MC, Arlot ME, Delmas PD et al (1994) Effect of calcium and cholecalciferol treatment for three years on hip fractures in elderly women. BMJ 308:1081–1082
Meunier PJ, Chapuy MC, Arlot ME et al (1994) Can we stop bone loss and prevent hip fractures in the elderly? Osteoporos Int 4[Suppl 1]:S71–S76
Lips P, Chapuy MC, Dawson-Hughes B et al (1999) An international comparison of serum 25-hydroxyvitamin D measurements. Osteoporos Int 9:394–397
Dawson-Hughes B, Harris SS, Krall EA et al (1997) Effect of calcium and vitamin D supplementation on bone density in men and women 65 years of age or older. N Engl J Med 337:670–676
Trivedi DP, Doll R, Khaw KT (2003) Effect of four monthly oral vitamin D3 (cholecalciferol) supplementation on fractures and mortality in men and women living in the community: randomised double blind controlled trial. BMJ 326:469–472
Meyer HE, Smedshaug GB, Kvaavik E et al (2002) Can vitamin D supplementation reduce the risk of fracture in the elderly? a randomized controlled trial. J Bone Miner Res 17:709–715
Shea B, Wells G, Cranney A et al (2002) Meta-analysis of calcium supplementation for the prevention of postmenopausal osteoporosis. Endocr Rev 23:552–559
Papadimitropoulos E, Wells G, Shea B et al (2002) Meta-analysis of the efficacy of vitamin D treatment in preventing osteoporosis in postmenopausal women. Endocr Rev 23:560–569
Gillespie WJ, Avenell A, Henry DA et al (2001) Vitamin D and vitamin D analogues for preventing fractures associated with involutional and post-menopausal osteoporosis. Cochrane Database Syst Rev 1:CD000227
Bischoff HA, Stahelin HB, Dick W et al (2003) Effects of vitamin D and calcium supplementation on falls: a randomized controlled trial. J Bone Miner Res 18:343–351
Pfeifer M, Begerow B, Minne HW et al (2000) Effects of a short-term vitamin D and calcium supplementation on body sway and secondary hyperparathyroidism in elderly women. J Bone Miner Res 15:1113–1118
Lilliu H, Pamphile R, Chapuy M-C et al (2003) Calcium-vitamin D3 supplementation is cost-effective in hip fractures prevention. Maturitas 44:299–305
European Agency for Evaluation of Medicinal Products (1999) Note for guidance on involutional osteoporosis in women, CPMP/EWP/552/95. European Agency for Evaluation of Medicinal Products, London
International Osteoporosis Foundation (2001) Osteoporosis in the European Community: a call to action—an audit of policy developments since 1998. http://www.osteofound.org/publications/pdf.eu_report.pdf. Cited 3 October 2003
Juby AG, Davis P (2001) A prospective evaluation of the awareness, knowledge, risk factors and current treatment of osteoporosis in a cohort of elderly subjects. Osteoporos Int 12:617–622
Dawson-Hughes B, Harris SS, Krall EA et al (2000) Effect of withdrawal of calcium and vitamin D supplements on bone mass in elderly men and women. Am J Clin Nutr 72:745–750
Romagnoli E, Colangeli I, Minisola S (2000) Awareness, attitudes and opinions on osteoporosis of primary care physicians working in the metropolitan area of Rome: a brief report. Aging Clin Exp Res 12:240–244
Cranney A, Guyatt G, Griffith L et al, the Osteoporosis Methodology Group and the Osteoporosis Research Advisory Group (2002) Meta-analyses of therapies for postmenopausal osteoporosis, IX: summary of meta-analyses of therapies for postmenopausal osteoporosis. Endocr Rev 23:570–578
Koster JC, Hockeng WHL, Mulder H (1996) Diminished effect of etidronate in vitamin D deficient osteopenic postmenopausal women. Eur J Clin Pharmacol 51:145–147
Masud T, Mulcahy B, Thompson AV et al (1998) Effects of cyclical etidronate combined with calcitriol versus cyclical etidronate alone on spine and femoral neck bone mineral density in postmenopausal osteoporotic women. Ann Rheum Dis 57:346–349
Nieves JW, Komar L, Cosman F et al (1998) Calcium potentiates the effect of estrogen and calcitonin on bone mass: review and analysis. Am J Clin Nutr 67:18–24
Sirola J, Kroger H, Sandini L et al (2003) Interaction of nutritional calcium and HRT in prevention of postmenopausal bone loss: a prospective study. Calcif Tissue Int 72(6):659
Adebowale AO, Cox DS, Liang Z et al (2000) Analysis of glucosamine and chondroitin sulfate content in marketed products and the caco-2 permeability of chondroitin sulfate raw materials. J Am Nutr Assoc 3:37–44
Heaney RP, Barger-Lux MJ (2002) Not all calcium carbonate supplements are equally absorbable. 24th annual meeting ASBMR
Acknowledgements
This paper reports the conclusions from an international expert meeting organized in Barcelona on 10 November 2002, under the auspices of the World Health Organization Collaborating Center for Public Health Aspects of Rheumatic Diseases (Liège, Belgium) and supported in part by an unrestricted educational grant from Nycomed, Novartis, Shire and Orion Pharma. Dr S. Boonen is senior clinical investigator of the Fund for Scientific Research, Flanders, Belgium (F.W.O–Vlaanderen).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Boonen, S., Rizzoli, R., Meunier, P.J. et al. The need for clinical guidance in the use of calcium and vitamin D in the management of osteoporosis: a consensus report. Osteoporos Int 15, 511–519 (2004). https://doi.org/10.1007/s00198-004-1621-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-004-1621-6