Abstract
Summary
Older veterans with acute hip fracture do not receive adequate evaluation and treatment for osteoporosis, irrespective of their age and underlying health status.
Introduction
Hip fractures are a serious complication of osteoporosis, leading to high mortality and morbidity. Prior studies have found significant undertreatment of osteoporosis in women with hip fracture. We examined the rate of bone density (BMD) testing and osteoporosis treatment among a predominantly male population hospitalized with hip fractures.
Methods
We conducted a retrospective cohort study of patients age 65 years and older hospitalized in U.S. Department of Veterans Affairs (VA) hospitals with hip fracture (N = 3,347) between 1 October, 2004 and 30 September, 2006. The primary outcome was receipt of BMD testing or initiation of pharmacotherapy within 12 months of fracture.
Results
The mean age of the study population was 79.0 years (SD = 6.7), 96.5% were male, and 83.3% were white. Only 1.2% of hip fracture patients underwent BMD testing and 14.5% received osteoporosis therapy within 12 months of fracture. Among fracture patients with minimal comorbid illness (N = 756) only 1.6% underwent BMD testing and 13.0% received pharmacotherapy. In logistic regression models, treatment rates were higher for women compared to men (odds ratio, 3.30; 95% CI, 2.16–5.04) and lower for blacks compared to whites (odds ratio, 0.67; 95% CI, 0.45–0.99).
Conclusions
Evaluation and treatment of osteoporosis among patients with fractures is suboptimal even in an integrated healthcare delivery system with generous pharmaceutical coverage. This study suggests that the undertreatment of osteoporosis demonstrated in the private sector is also present within the VA.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Hip fractures in the elderly are commonly associated with low-impact trauma combined with underlying osteoporosis. Bergström et al. found that 53% of hip fractures in individuals 50 years of age or older and 80% of hip fractures in those 75 years of age or older are the result of low-impact trauma, suggesting underlying osteoporosis [1]. Hip fractures not only cause loss of function and excess mortality [2–4], but they predict additional fractures in the survivors [5–7]. For this reason, existing guidelines recommend that all patients with low-impact trauma undergo treatment for osteoporosis [8]. A number of analyses conducted over the last 15 years suggest that less than 20% of patients experiencing low-impact hip fractures are prescribed therapy for osteoporosis [9–19]. However few of these studies contained significant numbers of men with fractures. Moreover, few of these analyses were able to comprehensively evaluate use of pharmacotherapy because many were conducted in settings with incomplete access to patient pharmacy records.
The Veterans Administration Healthcare System (VA) is the largest integrated delivery system in the USA and treats more than 2,000 hip fracture patients every year. However data assessing the evaluation and treatment of veterans experiencing hip fracture are very limited. In fact, with the exception of three small studies evaluating a total of 394 patients admitted with a hip fracture to nine VA Medical Centers in the Midwest and North Carolina between 1993 and 2001, data examining the treatment of hip fractures in the VA are not available [17–19]. The VA affords a unique opportunity to evaluate hip fracture evaluation and treatment patterns because of its comprehensive administrative data files and the generous pharmaceutical benefits that are available to most patients.
We conducted a retrospective cohort study to evaluate contemporary management of patients treated for acute hip fracture within the VA. In particular, we set out to examine the frequency of bone mineral density evaluation and initiation of osteoporosis pharmacotherapy within 1 year of a hip fracture among older veterans.
Methods
Data sources
We used computerized patient information from three VA administrative databases: the patient treatment file (PTF) and outpatient care file (OPC) databases maintained by the VA Automation Center in Austin, Texas and the pharmacy benefits management (PBM) database maintained by the VA Information Resource Center at the Hines VA Medical Center in Oak Brook, Illinois. The PTF and OPC databases are a set of linked databases that provide information on all inpatient and outpatient encounters at VA facilities and have been used extensively in health services research. The PTF contains discharge abstract data for all patients hospitalized in VA medical centers. Key data elements include patient demographics, admission dates, primary and secondary diagnoses and procedures performed during hospitalization as defined by International Classification of Diseases Ninth Clinical Modification (ICD-9-CM) codes. The OPC contains administrative data on all outpatient encounters at VA clinics. Data elements include dates of visits, type of clinic (e.g., primary care, mental health), diagnoses defined by ICD-9-CM codes, and procedures performed at each encounter defined by Current Procedural Terminology (CPT) codes. All encounters include patient unique identifiers that allow merging of information across the databases. The PBM database contains patient-level information on all outpatient prescriptions filled in an outpatient VA pharmacy.
Patients
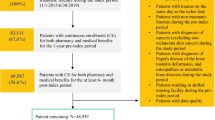
We identified all patients 65 years of age and older with no prior diagnosis of osteoporosis and taking no osteoporosis medications admitted to VA hospitals with acute hip fracture between 1 October, 2004 and 30 September, 2006 (N = 4,397). We limited the analysis to patients 65 years of age or older because most hip fractures in this age group are caused by low-impact trauma and thus can be assumed to be related to underlying osteoporosis [1]. We excluded patients with a prior diagnosis of osteoporosis and patients who were receiving osteoporosis therapy during the 6 months preceding the fracture because we were mainly interested in studying the osteoporosis evaluation and treatment process triggered by an acute fracture in patients who were not already recognized as having osteoporosis. We also excluded patients who died within 3 months of fracture (N = 1,101) because we theorized that the severity of illness in this patient population at the time of fracture might have discouraged providers from initiating osteoporosis treatment. We also excluded patients with metastatic cancer (N = 102) because bisphosphonates may be used for the treatment of bone metastases rather than osteoporosis in this group, making it difficult to discern whether bisphosphonate therapy in this population was started because of recognition of osteoporosis or to treat the underlying malignancy.
Data elements
We identified patients hospitalized with hip fracture using ICD-9 codes 820.0 (820.00–820.09), 820.1 (820.10–820.19), 820.2 (820.20–820.22), 820.3 (820.30–820.32), 820.8, and 820.9. Patients with a prior diagnosis of osteoporosis identified in either the PTF or OPC files (ICD-9 codes 733.00 to 733.09) were excluded.
Subsequent measurement of bone mineral density (BMD) testing following the index fracture was assessed using appropriate ICD-9 (88.98) and CPT (76977, 77079, 77080, 77081, 77082, 78350, 78351) codes for dual energy x-ray absorptiometry (DXA), quantitative computed tomography, and heel ultrasonography.
Initiation of osteoporosis therapy was assessed by searching the PBM files for each patient for bisphosphonates, estrogen, raloxifene, calcitonin, and teriparatide prescriptions. Data on the use of calcium and/or vitamin D was not collected since standard of care for osteoporosis following a fracture typically includes an antiresorptive or an anabolic agent in addition to calcium and vitamin D. Moreover, calcium and vitamin D are commonly purchased by patients without a prescription and thus use of these agents is not reliably captured by pharmacy data.
Additional data elements extracted from the PTF and OPC databases were age, sex, race, VA hospital, and primary and secondary diagnoses. Comorbidities were defined based on algorithms described by Quan et al. [20, 21], and identified based on diagnoses present on all VA encounters within the 12 months preceding the date of admission with hip fracture.
Statistical analysis
We began by estimating the frequency of initiation of osteoporosis therapy and of bone mineral density testing within 1 year of fracture in our population of patients who were fractured. We also calculated the proportion of patients who sustained a hip fracture in the 2 years preceding the index fracture and in the 2 years following it. We then stratified our study sample into those who did receive pharmacologic therapy for osteoporosis and those who did not receive therapy and we used bivariate methods (chi-square tests and two-sample t tests) to compare the demographic characteristics (e.g., age, race, sex) and prevalence of comorbid illness among the two groups.
Because we hypothesized that some clinicians might be reluctant to treat osteoporosis among patients with multiple comorbid conditions (i.e., clinicians might decide not to treat osteoporosis in patients with severe underlying illness), we conducted additional analyses to examine whether treatment rates might differ among hip fracture patients with higher and lower burden of comorbidities. We thus stratified our cohort into a subgroup of patients with less severe comorbidities and a subgroup with more severe comorbidities. This stratification was based upon the clinical judgment of the investigators. The cohort of patients with less severe comorbidity included all patients with no coexisting comorbidities as well as patients whose comorbidities were limited to uncomplicated hypertension, uncomplicated diabetes, arthritis, depression, hypothyroidism, obesity, or rheumatoid arthritis/collagen vascular disease. The cohort of patients with more severe comorbidities included the rest of the patients. We estimated the frequency of initiation of osteoporosis therapy and of bone mineral density testing within 1 year of fracture in both groups and we used chi-square tests and two-sample t tests to examine differences in demographics and in the rates of osteoporosis evaluation and treatment between the two groups.
We used logistic regression to examine the association between patient characteristics and treatment of osteoporosis within 12 months of fracture. The models constructed included variables for patient sex, age, race, the number of comorbidities (obtained by computing the total number of comorbidities listed for each patient), and individual comorbidities and accounted for clustering by hospital.
All analyses were conducted using SAS for Windows, version 9.2 (SAS Institute Inc., Cary, NC).
The institutional review board at the University of Iowa, Carver College of Medicine, and the VA Medical Center, Iowa City, Iowa, approved this study.
Results
We identified 4,397 patients 65 years of age or older (Fig. 1) who were admitted to the VA with a hip fracture between 1 October, 2004 and 30 September, 2006 and who did not have a previous diagnosis of osteoporosis and were not receiving osteoporosis therapy. One thousand one hundred and one (25.0%) patients were excluded because they died within 3 months of the fracture and 102 (2.3%) were excluded because they had metastatic cancer, leaving a final cohort of 3,347 (76.1%) patients. A description of our study cohort is found in Table 1. Men constituted 96.5% of our population, 83.3% were Caucasians and the average age was 79.0 years.
Only 30 subjects (0.9% of our study population) had experienced a hip fracture in the 2 years preceding the index fracture and 285 (8.5% of our study population) experienced a recurrent hip fracture during the 2 years following the index fracture.
Forty-two patients (1.2%) of the final cohort underwent bone mineral density testing by DXA, quantitative CT or heel ultrasonography, and 487 (14.5%) received osteoporosis therapy in the form of a bisphosphonate, estrogen, raloxifene, calcitonin, or teriparatide within 1 year of fracture. The demographic characteristics of patients who received treatment for osteoporosis were generally similar to the characteristics of patients who did not receive osteoporosis therapy. In particular, patient age, race, and number of comorbid conditions were similar among patients who did and did not receive treatment (Table 1). Men who were fractured were significantly less likely to receive therapy when compared with women (13.9% versus 33.6%, p value < 0.0001), and blacks were significantly less likely to receive therapy when compared to whites (10.1% versus 15.0%, p value 0.01). The mean number of comorbid conditions (as identified using the algorithms of Quan et al.) was similar among patients who did and did not receive therapy, though dementia was significantly less common among fracture patients who received treatment when compared to those who did not (6.6% versus 10.4%, p value <.01).
In stratified analyses, rates of osteoporosis testing and treatment were no higher among patients with less severe comorbidity when compared to patients with more severe comorbidity (Table 2).
In logistic regression models, the odds of receiving therapy for osteoporosis within 1 year of fracture was significantly higher for women as compared to men (odds ratio, 3.30; 95% CI, 2.16–5.04) and significantly lower for blacks as compared to whites (odds ratio, 0.67; 95% CI, 0.45–0.99; Table 3).
Discussion
This study shows that, in an analysis of contemporary data from a large integrated healthcare delivery system, older patients with hip fractures do not receive adequate evaluation and treatment for osteoporosis, irrespective of age and the number of coexisting medical conditions. In aggregate, only 1.2% of hip fracture patients underwent bone mineral density testing and 14.5% received osteoporosis therapy within 1 year of fracture. Even among patients with a relatively modest burden of comorbid illness, we found that only 1.6% of patients underwent bone mineral density testing and 13.0% received therapy. While measurement of bone mineral density is not always necessary to make a diagnosis of osteoporosis after a low-trauma fracture, pharmacotherapy is recommended in most patients with hip fracture, yet our study shows that few veterans received osteoporosis therapy. Moreover, men and patients with dementia are less likely to receive treatment for osteoporosis after a hip fracture. These results suggest a substantial opportunity for improvement in the management of fragility fractures in the VA.
Our results are consistent with prior studies from an array of different practice settings suggesting undertreatment of osteoporosis among fracture patients [9–19]. For example, in a systematic review of 37 studies from the USA, the UK, Canada, Australia, Europe, New Zealand, Israel and South Africa, Elliot-Gibson et al. found that only 0.5–38% of fracture patients received bisphosphonate therapy and that treatment rates exceeded 10% in six studies only [15].
Likewise, in a study of veterans with hip fracture Kamel et al. found that of 232 patients with a hip fracture admitted to seven Midwestern VA Medical Centers between 1998 and 2001, only 4.5% were treated with a bisphosphonate [17]. In two smaller studies using older data, Riley et al. and Colo'n-Emeric et al. reported equally low rates of osteoporosis evaluation and treatment in veterans with hip fractures [18, 19]. While confirming results from previous similar analyses using VA data [17–19], the current study had access to a larger database covering the whole VA healthcare system and not limited to certain geographic areas, and had a more complete access to pharmacy records making the findings more generalizable. Moreover, our findings are striking in that, in using contemporary data, we have found continued undertreatment of fragility fractures despite widespread recognition that this is a problem.
Studies attempting to elucidate the barriers to osteoporosis treatment following a low-trauma fracture indicate a lack of awareness among physicians and patients that a low-trauma fracture is often indicative of underlying osteoporosis [22, 23]. Another major barrier is the unwillingness of the physicians involved in the care of these patients to assume the responsibility for evaluating and treating osteoporosis [22–25].
Our finding that women were approximately three-times more likely to receive osteoporosis therapy than men is consistent with prior literature [26–28]. In a national population-based cohort study, Roerholt et al. found that 39.6% of women versus 16.5% of men receive therapy after a vertebral fracture and that 9.2% of women versus 4.1% of men receive therapy after a hip fracture [26]. While a precise explanation for the discrepancy in treatment rates between women and men has not been identified, there is a well recognized tendency by both medical professionals and patients to consider osteoporosis a disease of women [29, 30]. The under-recognition and undertreatment of osteoporosis in men is important since 40% of all osteoporotic fractures and 30% of hip fractures occur in men [31] and there is increasing data that osteoporosis treatment is effective in men and women alike [32–35]. Our finding of undertreatment of osteoporosis is all the more striking given that our study was conducted in a healthcare system where the patient population is overwhelmingly male and with a well-established track record of translating research findings into quality improvement. At the same time it is possible that by focusing quality improvement efforts on diseases that are most common among men (e.g., hypertension, heart disease, lung cancer), the VA has been slower than other study settings in embracing osteoporosis diagnosis and treatment of osteoporosis. The VA has taken a number of concrete steps to improve quality including the creation of the Quality Enhancement Research Initiative (QUERI) program in 1998 specifically to implement findings from research into routine clinical practice. Under this program, there are nine centers focused on nine high-prevalence or high-risk diseases among veterans (chronic heart failure, diabetes mellitus, HIV/AIDS, ischemic heart disease, mental health, polytrauma and blast-related injuries, spinal cord injury, stroke, and substance abuse). Each QUERI center follows a standard process that consists of a series of activities aiming at systemizing quality improvement at the VA. This process starts by identifying high-risk and high-volume health conditions, the best evidence-based practices related to these conditions, and the variations between prevailing VA practices and the best practices. Subsequently, interventions are identified and implemented in order to promote the best practices, and steps are taken to study the effect of these interventions on outcomes. While only limited outcome data is available at this time, it is projected that the interventions that have been implemented through the diabetes mellitus and ischemic heart disease QUERI centers, for example, will prevent around 16,000 cardiovascular events and 10,000 deaths over 20 years [36].
Osteoporosis has not been a traditional research or quality improvement focus within VA and, from a population health perspective this has made sense given the epidemics of diabetes, hypertension, cardiovascular disease, and substance abuse facing confronting the VA. At the same time, there is growing evidence that appreciation of osteoporosis as a threat to veterans' health is increasing. A recent report published by the Department of Veterans Affairs in July 2010 recognizes the under-diagnosis and undertreatment of osteoporosis in veterans with hip or vertebral fractures, and proposes to improve osteoporosis care in veterans with fractures through a program that focuses on provider education, patient education, and regular surveillance. Some elements of this program were initiated in summer 2010 [37]. While further research and surveillance are needed to assess the impact of these initiatives, it is our hope that these initial efforts will translate into a VA wide program that aims to deliver adequate osteoporosis care to all veterans with low-impact fractures. As a matter of fact, the VA may benefit from the experience of other integrated health delivery systems that have demonstrated significant improvements in osteoporosis care with interventions aiming at increasing patient and physician awareness of the risk of osteoporosis in the setting of a low-trauma fracture, and at facilitating testing and treatment for osteoporosis following discharge from the hospital. More specifically, in a study involving patients from a nonprofit health maintenance organization in the USA, Feldstein et al. showed that an electronic reminder delivered to the primary care provider significantly increased (6% to 51%) the proportion of patients receiving BMD testing or an osteoporosis medication following a fracture [38]. In a large integrated healthcare system in Alberta, Canada, Majumdar et al. demonstrated a significant increase in the rates of bisphosphonate therapy (from 7% to 22%) when hip fracture patients received telephone-based education and their primary care physicians were provided with evidence-based practice guidelines and electronic reminders in relation to the recent fracture in their patients [39]. The same group also showed an even better improvement in the rates of bisphosphonate therapy (from 22% to 51%) when a case manager provided one-on-one education to patients after hip fracture, arranged for BMD testing and provided a prescription for bisphosphonate to those with a low BMD [40].
Given the great similarities between these study settings and the VA system, in terms of the availability of specialty-based case managers and an electronic medical record that is capable of delivering electronic reminders and “best practice” recommendations to providers, we believe that results from these trials can be used to design a program within the VA that aims at enhancing osteoporosis awareness among veterans with low-trauma fractures and their providers and at improving osteoporosis care delivered to these veterans.
In our cohort, 8.5% of patients suffered a recurrent hip fracture in the 2 years following the index fracture, consistent with previously reported fracture recurrence rates that range between 4 and 10%. In 91 male veterans and 118 community-dwelling men with a hip fracture followed for up to 36 months, Colón-Emeric et al. identified 17 recurrent hip or pelvis fractures (8%) [7]. Likewise, Johnell et al. identified 50 new hip fractures within 2 years of a prior hip fracture in a cohort of 1,150 patients (~4%), with a comparable risk of fracture recurrence between men and women [41].
An interesting finding of this study is the fact patients with dementia are less likely to receive therapy for osteoporosis following a hip fracture. This finding has previously been noted by Jones et al. who found that patients with dementia were less than half as likely as cognitively intact patients to receive osteoporosis therapy after a hip fracture [42]. This may be due to the decreased functional and cognitive capacity and to the shorter life expectancy in patients with dementia, making physicians less inclined to deliver aggressive or complex medical therapy. As a matter of fact, several studies have demonstrated reluctance among physicians to treat patients with dementia, mostly because of the perceived futility of such an intervention [22, 23].
It is important to acknowledge potential limitations of this work. First, our analysis was limited to the evaluation and treatment of osteoporosis conducted within the VA. We were unable to evaluate care that was provided outside of the VA and we suspect that some veterans may have received BMD evaluation outside the VA, thus partly accounting for the low testing rates seen in this study. That said, osteoporosis medications are relatively expensive and VA pharmacy benefits are relatively generous making it unlikely that significant numbers of patients in our study would be choosing to pay for therapy out of pocket, especially that the study evaluates treatment rates prior to 2008, when alendronate became available in less-expensive generic forms. In addition, and since it is well known that the rates of osteoporosis treatment following a hip fracture are equally low outside the VA, it is highly improbable that these patients received treatment for osteoporosis from non-VA sources. Second, our data were abstracted from administrative records, so some important clinical details were lacking, in particular with regard to falls.
In summary, we found that only a small number of older veterans with hip fracture receive evaluation and/or treatment for osteoporosis, irrespective of their age and overall health status. Our findings suggest significant opportunities for improving care of veterans experiencing hip fracture and highlight the need to introduce effective nationwide programs linking fracture care to osteoporosis management in the VA.
References
Bergström U, Bjornstig U, Stenlund H, Jonsson H, Svensson O (2008) Fracture mechanisms and fracture pattern in men and women aged 50 years and older: a study of a 12-years population-based register, Umea, Sweden. Osteoporos Int 19:1267–1273
Abrahamsen B, van Staa T, Ariely R, Olson M, Cooper C (2009) Excess mortality following hip fracture: a systematic epidemiological review. Osteoporos Int 20:1633–1650
Beringer TR, Clarke J, Elliott JR, Marsh DR, Heyburn G, Steele IC (2006) Outcome following proximal femoral fracture in Northern Ireland. Ulster Med J 75:200–206
Koval KJ, Zuckerman JD (1994) Functional recovery after fracture of the hip. J Bone Joint Surg Am 76:751–758
Klotzbuecher CM, Ross PD, Landsman PB, Abbott TA III, Berger M (2000) Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res 15:721–739
van Staa TP, Leufkens HG, Cooper C (2002) Does a fracture at one site predict later fractures at other sites? A British cohort study. Osteoporos Int 13:624–629
Colón-Emeric CS, Sloane R, Hawkes WG (2000) The risk of subsequent fractures in community dwelling men and male veterans with hip fracture. Am J Med 109:324–326
National Osteoporosis Foundation (2010) Clinician's guide to prevention and treatment of osteoporosis. National Osteoporosis Foundation, Washington, DC
Juby AG, De Geus-Wenceslau CM (2002) Evaluation of osteoporosis treatment in seniors after hip fracture. Osteoporos Int 13:205–210
Follin SL, Black JN, McDermott MT (2003) Lack of diagnosis and treatment of osteoporosis in men and women after hip fracture. Pharmacotherapy 23:190–198
Torgerson DJ, Dolan P (1998) Prescribing by general practitioners after an osteoporotic fracture. Ann Rheum Dis 57:378–379
Kamel HK, Hussain MS, Tariq ST, Perry HM III, Morley JE (2000) Failure to diagnose and treat osteoporosis in elderly patients hospitalized with hip fracture. Am J Med 109:326–328
Andrade SE, Majumdar SR, Chan A, Buist DSM, Go AS, Goodman M, Smith DH, Platt R, Gurwitz JH (2003) Low frequency of treatment of osteoporosis among postmenopausal women following a fracture. Arch Intern Med 163:2052–2057
Siris ES, Bilezikian JP, Rubin MR, Black DM, Bockman RS, Bone HG, Hochberg MC, McClung MR, Schnitzer TJ (2003) Pins and plasters aren't enough: a call for the evaluation and treatment of patients with osteoporotic fractures. J Clin Endocrinol Metab 88:3482–3486
Elliot-Gibson V, Bogoch ER, Jamal SA, Beaton DE (2004) Practice patterns in the diagnosis and treatment of osteoporosis after a fragility fracture: a systematic review. Osteoporos Int 15:767–778
Harrington JT, Broy SB, Derosa AM, Licata AA, Shewmon DA (2002) Hip fracture patients are not treated for osteoporosis: a call to action. Arthritis Rheum 47:651–654
Kamel HK, Bida A (2004) Secondary prevention of hip fractures in veterans: can we do better? J Am Geriatr Soc 52:647–648
Riley RL, Cames ML, Gudmundsson A, Elliott ME (2002) Outcomes and secondary prevention strategies for male hip fractures. Ann Pharmacother 36:17–23
Colo'n-Emeric C, Yballe L, Sloane R, Pieper CF, Lyles KW (2000) Expert physician recommendations and current practice patterns for evaluating and treating men with osteoporotic hip fracture. J Am Geriatr Soc 48:1261–1263
Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, Saunders LD, Beck CA, Feasby TE, Ghali WA (2005) Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 43:1130–1139
Elixhauser A, Steiner C, Harris DR, Coffey RM (1998) Comorbidity measures for use with administrative data. Med Care 36:8–27
Kaufman JD, Bolander ME, Bunta AD, Edwards BJ, Fitzpatrick LA, Simonelli C (2003) Barriers and solutions to osteoporosis care in patients with a hip fracture. J Bone Joint Surg Am 85-A:1837–1843
Levinson MR, Clay FJ (2009) Barriers to the implementation of evidence in osteoporosis treatment in hip fracture. Int Med J 39:199–202
Sheehan J, Mohamed F, Reilly M, Perry IJ (2000) Secondary prevention following fractured neck of femur: a survey of orthopaedic surgeons practice. Ir Med J 93:105–107
Simonelli C, Killeen K, Mehle S, Swanson L (2002) Barriers to osteoporosis identification and treatment among primary care physicians and orthopedic surgeons. Mayo Clin Proc 77:334–338
Roerholt C, Eiken P, Abrahamsen B (2009) Initiation of anti-osteoporotic therapy in patients with recent fractures: a nationwide analysis of prescription rates and persistence. Osteoporos Int 20:299–307
Kiezbak GM, Beinart GA, Perser K, Ambrose CG, Sift SJ, Heggeness MH (2002) Undertreatment of osteoporosis in men with hip fracture. Arch Intern Med 162:2217–2222
Panneman MJ, Lips P, Sen SS, Herings RM (2004) Undertreatment with anti-osteoporotic drugs after hospitalization for fracture. Osteoporos Int 15:120–124
Al Attia H, Adams B (2007) Osteoporosis in men: are we referring enough for DXA and how? Clin Rheumatol 26:1123–1126
Madeo B, Zirilli L, Caffagni G, Diazzi C, Sanguanini A, Pignatti E, Carani C, Rochira V (2007) The osteoporotic male: overlooked and undermanaged? Clin Interv Aging 2:305–312
Johnell O, Kanis JA (2006) An estimate of the worldwide prevalence and disability associated with osteoporotic fracture. Osteoporos Int 17:1726–1733
Ringe JD, Farahmand P, Faber H, Dorst A (2009) Sustained efficacy of risedronate in men with primary and secondary osteoporosis: results of a 2-year study. Rheumatol Int 29:311–315
Kaufman JM, Orwoll E, Goemaere S, San Martin J, Hossain A, Dalsky GP, Lindsay R, Mitlak BH (2005) Teriparatide effects on vertebral fractures and bone mineral density in men with osteoporosis: treatment and discontinuation of therapy. Osteoporos Int 16:510–516
Lyles KW, Colón-Emeric CS, Magaziner JS, Adachi JD, Pieper CF, Mautalen C, Hyldstrup L, Recknor C, Nordsletten L, Moore KA, Lavecchia C, Zhang J, Mesenbrink P, Hodgson PK, Abrams K, Orloff JJ, Horowitz Z, Eriksen EF, Boonen S, Recurrent Fracture Trial HORIZON (2007) Zoledronic acid and clinical fractures and mortality after hip fracture. N Engl J Med 357:1799–1809
Orwoll E, Ettinger M, Weiss S, Miller P, Kendler D, Graham J, Adami S, Weber K, Lorenc R, Pietschmann P, Vandormael K, Lombardi A (2000) Alendronate for the treatment of osteoporosis in men. N Engl J Med 343:604–610
McQueen L, Mittman BS, Demakis JG (2004) Overview of the Veterans Health Administration (VHA) Quality Enhancement Research Initiative (QUERI). J Am Med Inform Assoc 11:339–343
Department of Veterans Affairs Office of Inspector General (2010) Healthcare Inspection Management of osteoporosis in veterans with fractures; Rpt # 09-03138-191. http://www4.va.gov/oig/54/reports/VAOIG-09-03138-191.pdf. Accessed 12 November 2010.
Feldstein A, Elmer PJ, Smith DH, Herson M, Orwoll E, Chen C, Aickin M, Swain MC (2006) Electronic medical record reminder improves osteoporosis management after a fracture: a randomized, controlled trial. J Am Geriatr Soc 54:450–457
Mjumdar SR, Johnson JA, McAlister FA, Bellerose D, Russell AS, Hanley DA, Morrish DW, Maksymowych WP, Rowe BH (2008) Multifaceted intervention to improve diagnosis and treatment of osteoporosis in patients with recent wrist fracture: a randomized controlled trial. CMAJ 178:569–575
Majumdar SR, Beaupre LA, Harley CH, Hanley DA, Lier DA, Juby AG, Maksymowych WP, Cinats JG, Bell NR, Morrish DW (2007) Use of a case manager to improve osteoporosis treatment after hip fracture. Results of a randomized controlled trial. Arch Intern Med 167:2110–2115
Johnell O, Kanis JA, Odén A, Sernbo I, Redlund-Johnell I, Petterson C, De Laet C, Jönsson B (2004) Fracture risk following an osteoporotic fracture. Osteoporos Int 15:175–179
Jones G, Warr S, Francis E, Greenaway T (2005) The effect of a fracture protocol on hospital prescriptions after minimal trauma fractured neck of the femur: a retrospective audit. Osteoporos Int 16:1277–1280
Acknowledgments
Dr. Vaughan-Sarrazin is a Research Scientist in the Center for Comprehensive Access and Delivery Research and Evaluation (CADRE) at the Iowa City VA Medical Center, which is funded through the Department of Veterans Affairs, Veterans Health Administration, Health Services Research and Development Service. Dr. Cram was supported by a K23 career development award (RR01997201) from the NCRR at the NIH and the Robert Wood Johnson Faculty Scholars Program. He is currently supported by R01 HL085347-01A1 from NHLBI, R01 AG33035 from NIA, and the Department of Veterans Affairs.
Conflicts of interest
All authors took part in the conception and design of the study; analysis and interpretation of data; drafting of the article or revising it critically for important intellectual content and final approval of the version to be published. The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shibli-Rahhal, A., Vaughan-Sarrazin, M.S., Richardson, K. et al. Testing and treatment for osteoporosis following hip fracture in an integrated U.S. healthcare delivery system. Osteoporos Int 22, 2973–2980 (2011). https://doi.org/10.1007/s00198-011-1536-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-011-1536-y