Abstract
Summary
Metacarpal thickness (T), width (W), length (L) and medullary diameter (M) were measured in 3,121 X-rays from 231 healthy Caucasian children aged 3 to 19 years and analysed for bone age, age, height, weight and gender-related characteristics, showing highly differentiated growth patterns with prepubertal dips. Reference data for the four metacarpal measures are presented.
Introduction
The aim of the study was to create and explore a reference database for metacarpal T, W, L and M in children.
Methods
Three thousand one hundred twenty-one left-hand X-rays (1,661 from boys) from 231 healthy Caucasian subjects (119 boys) aged 3 to 19 years were analysed by BoneXpert, a programme for automatic analysis of hand X-rays and bone age (BA; in years).
Results
In boys, growth of T, W and L shows a prepubertal decrease from BA 7 to 13 and then accelerates again. In girls, the same is seen only for T starting from BA 8 to 11, whereas W and L grow at a declining rate. M shows steady growth until BA 10.5 in girls and BA 13.5 in boys and then grows smaller in both. W is greater in boys from BA 6 onwards, while L is greater in girls from BA 9 to 13 and T from BA 11 to 14. BA is reflected best by L until start of puberty and by T and L thereafter.
Conclusion
T, W, L and M show highly differentiated growth patterns. These reference data provide a basis for further research into skeletal development and the management of hormone therapies in children.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The advance of computerised image analysis methods has revived interest in the study of bones by radiogrammetry. Recent radiogrammetric studies have mostly focussed on composite indices which have been formulated to correlate with the mass and hence strength of long bones [1–4]. Comparatively little attention has been given to the parameters that make up such indices. However, studying the dimensions of long bones can tell us more about the skeleton than just its mass, particularly during skeletal development. Having a large reference database on metacarpal thickness (T), width (W), length (L), medullary diameter (M = W – 2 × T) and bone age in children from age 3 to 19 should be of use to many lines of research in paediatrics, especially since hand X-rays are routinely taken for bone age assessment in many conditions and a wealth of retrospective material is available.
A search for previous literature on the dimensions of metacarpals in children takes us many years back. In 1968, Bonnard reported on metacarpal thickness and width in 1,682 X-rays from 175 Caucasian children from 3 months to 11 years of age [5]. His data were based on a subset of the then ongoing study of children born 1954–1955, which has come to be known as the First Zurich Longitudinal Study (1ZLS) [6, 7]. The present paper can be regarded as an update and expansion of Bonnard’s work. It follows the progress of metacarpal growth in 231 Caucasian children from the 1ZLS from early childhood through to late puberty, adding medullary diameter and length as further parameters and analysing them not only in relation to chronological age (CA; in years) but also to bone age (BA; in years) and height. Garn’s extensive studies on cortical bone are summarised in [8]. The present paper reconsiders many of his findings, adding the BA to the CA perspective.
Besides presenting reference data for T, W, L and M, we discuss their inter-gender differences as well as interrelationships and correlations with body height, weight, CA and BA as well as possible underlying endocrine and developmental processes.
The BA, T, W, L and M values for this study were all produced fully automatically by BoneXpert.
Materials and methods
Data
Three thousand three hundred seventy-nine X-rays were taken in total, covering all children of the 1ZLS from age 3 up to 18 years and thereafter only those still growing and hence with delayed BA. To minimise the resulting selection bias, we excluded all images from boys aged >19.5 years and girls aged >18.5 years (145 images from girls, 94 from boys). Sixteen images were excluded due to outliers in longitudinal charts of T (n = 14) and W (n = 2). These were attributable to poor image quality resulting from poor contrast or movement artefacts, for example. There were no further quality checks on the image material. The commercial version of BoneXpert is intended for clinical use on Digital Imaging and Communications in Medicine (DICOM) files only, and its application to original X-ray images here was exceptional. Poor image quality should thus be an even smaller concern in clinical practice than it was in this study. We had no images of children aged less than CA 2.5 because these X-rays had been performed on a film that had not stood the test of time and had decayed. This left us with only three images with BA < 3, which we therefore excluded. Some of the images from CA bins 4 to 6 had had to be discarded for the same reason. The remaining 3,121 images from 231 children—1,460 from 112 girls and 1,661 from 119 boys—were all included in this study. Ninety-four percent of the images were taken within 2 weeks and 99% within 1 month of the child’s birthday. X-rays were taken with 74 cm focus distance, 50 kVp tube voltage and a dose of 10 mAs.
Equipment
All films were scanned in 300 dpi with 12 bits/pixel using a Vidar Diagnostic Pro Advantage scanner (Vidar, Hemdon, VA, USA) with software version TWAIN 5.2. The scanner was adjusted to respond approximately linearly to the optical density of the film.
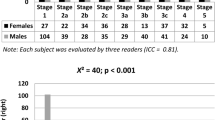
BoneXpert was developed from a database of 1,559 hand X-rays compiled from a number of studies on Caucasian children in the age range of 2–18 years. Its BA rating function, which supplies Greulich Pyle as well as Tanner Whitehouse ratings, has been refined and validated in clinically relevant and healthy populations [9–13], including the 1ZLS [14, 15]. It uses a statistical model to reconstruct the shape and X-ray opacity of the radius, ulna and short (RUS) bones (RUS bones of the hand, as used in the Tanner Whitehouse rating system). Figure 1 shows an example of the reconstruction of the bones and the dots relevant to the metacarpal measurements. Following image reduction to 150 dpi/8 bits, the boundaries of the metacarpals (and other bones) are determined. For more mature bones, the diaphysis and the fused epiphysis are delineated by a common boundary, while for the less mature bones, they each has a separate boundary. The diaphyseal boundary is computed as 64 points which correspond to the same anatomical locations across subjects [10, 16]. The bone axis is defined by two points corresponding to the proximal and distal ends of the diaphysis. L is measured along this axis and it includes the epiphysis. A region of interest (ROI) is centred 44% of L from the proximal end of the bone and extends 25% of L. In this region, the inner and outer borders of the cortical bone boundary are determined as shown in Fig. 1. The outer boundary is defined as a connected path running through locations with maximal gradient, while the inner boundary is the path of maximal intensity. Average values of W and T are determined from the ROI of each bone [4], with T being calculated as the average of radial and ulnar thickness. The entire measurement process is fully automatic, i.e. it is not possible to manipulate the measurement region manually.
Currently, BoneXpert is a Windows-based application. The DICOM image can be sent directly from the hospital’s picture archiving and communication system (PACS) to the PC where the automated method is installed. Full integration into a PACS environment is currently under preparation.
BoneXpert’s precision in measuring BA and metacarpal dimensions was determined on the basis of a subset of the present database for which right hand X-rays were also available: 1,666 right and left-hand X-ray pairs from girls with BA range 2–15 years and boys with BA range 2–17 years. The results for BA are given in [14], while the results for T, W, L and M are presented here. The observed variation in measurement of T, W and L can be modelled as being composed of two variance components: (1) two times the precision variance, i.e. the measurement uncertainty, of BoneXpert and (2) a genuine difference in T, W and L of the two hands. Based on the conservative assumption that any differences found between the left and right hand of an individual would be entirely attributable to imprecision of BoneXpert, we have calculated the upper limit on the contribution of the precision error of BoneXpert T, W and L measurement by plotting the difference between the left and right hand measurements against the average of left and right hand (Bland–Altman plot) and calculating the root mean square error (RMSE) of the line of fit. The precision error is conventionally quoted as the precision on a single measurement, which in this case is the RMSE divided by √2. The precision error (absolute value and percentage) was 0.05 mm (3.5%) for T, 0.12 mm (1.8%) for W, 0.21 mm (0.4%) for L and 0.12 mm (3.1%) for M.
Statistical analyses
All statistics were performed using the JMP 7 software package of SAS. T, W and L were computed from their average values in metacarpals 2–4 following the method proposed by Rosholm et al. [17], which avoids the less regular structure of metacarpals 1 and 5. M was calculated as W – 2 × T. Metacarpal dimensions were found to be normally distributed in 305 out of the 360 data subsets under study according to the Shapiro–Wilk test. Non-normal distributions appeared to be randomly interspersed among normal distributions through the age range, and it was therefore decided to assume normality throughout and dispense with the LMS method. The means and standard deviations of T, W, L and M were calculated by gender and BA bin, by gender and CA bin and by gender and height bin, two matrices of four metacarpal parameters by 33 bins (16 female) each for the BA and CA-related data and one matrix of 24 bins (12 female) for the height-related data. Inter-gender differences were calculated by BA bin. p values for differences in growth rates were determined by means of two-tailed t tests. Where differences were followed over multiple time intervals, p values were calculated according to the “repeated measures” method. Correlations with BA in children of equal age were calculated by CA and gender bin, giving 33 values of Spearman’s rank correlation coefficient for T, W, L and M, respectively. Correlations with height or weight were analogously calculated by BA and gender bin. Such correlation calculations presuppose a normal distribution of residuals of the linear fit. This was tested using the Shapiro–Wilk test and found to be true in nearly all cases. All-age correlations with BA and CA were calculated by gender and expressed in terms of the coefficient of determination r 2. The usual procedure to avoid making type 1 errors when addressing many different questions is to determine significance levels based on Bonferroni’s rule. However, due to the explorative nature of this study, we quote p values for each finding individually and dispense with making significance statements.
Data outside the intended BA ranges of BoneXpert (BA > 17 in boys and BA > 15 in girls) are demarcated in the figures and tables and should not be used for reference purposes.
Results
Tables 1, 2 and 3 give the reference values with standard deviations as well as relative annual growth rates of T, W, L and M in boys and girls by BA, CA and height bin, respectively. The resulting curves are depicted in Fig. 2. In the following, the word “growth” is used in the sense of growth rate.
T, W, L and M versus a BA, b CA and c height in boys and girls depicted as splines (lambda = 10). Coefficients of determination r2 are indicated on the left side for boys and on the right side for girls. For means and SD values, see Table 1
T, W and L in boys show relatively high growth rates from BA 4 to 7 followed by a phase of attenuated growth until BA 13 (rates of growth differ with p < 0.0001 for T, W and L, respectively; Table 4). Then their growth accelerates again during the pubertal growth spurt up to BA 15 (p < 0.0001 for T, W and L, respectively). This pattern is most pronounced for T in boys. In girls, the triphasic pattern is only seen for T (p < 0.0001, p < 0.0001), with a prepubertal dip from BA 8 to 11. W and L in girls decline in growth rate through the entire interval sequence (p < 0.0001, p < 0.0001). T grows at a consistently higher rate than W from BA 4 until after the pubertal spurt (BA 14 in girls, BA 15 in boys) in both genders (p < 0.0001 in either case) and at a higher rate than L in both genders during the pubertal spurt (p < 0.0001 in either case) and in girls from BA 4 to 8 (p < 0.0001).
T, W and L all level off earlier in girls than in boys: Successive BA bins cease to be significantly different (p < 0.05) in girls beyond 14 for T, 11 for W and 13 for L and in boys beyond BA 18 for T, 14 for W and 15 for L. From BA 18 in boys and BA 17 in girls, there is even a slight decrease in W and from BA 18 in girls also a slight decrease in L. This is due to the data beyond BA 18 in boys and BA 17 in girls being biased towards early maturers, as explained in the “Materials and methods” section and discussed below. By contrast, T shows undiminished growth up to the end of the BA range in both genders.
M in girls shows a steady increase until BA 10.5 (CA 11) followed by an equally steady decrease until BA 16, when it is approximately the same as at BA 3. In boys, M increases steadily and at a faster rate than in girls (p < 0.002 for the interval 4 < BA < 10) until around BA 13.5 (CA 13.5) and then shows a moderate decrease until BA 17, when it is approximately the same as at BA 10. The sharp decrease of M starting at BA 17 in girls and BA 18 in boys is due to the bias towards early maturers mentioned above.
W is larger in boys than in girls from BA 6 onwards and remains so. T and L show no significant differences between the sexes until BA 9. L is greater in girls from BA 9 to 13 (p < 0.0001) and T from BA 11 to 14 (p < 0.004). Boys first catch up on L, around BA 13–14, and around BA 14–15 on T and then surpass girls in both parameters (T p < 0.0004 at BA 15, L p < 0.0002 at BA 14). M is consistently greater in boys, the greatest difference being reached at BA 14 (4.3 versus 3.5 mm).
T, W, L and M correlate better with BA than with CA (Fig. 2). Figure 3 shows how the correlations of T, W, M and L with BA progress over time in boys and girls. L is a strong indicator of skeletal maturity for the greatest part of childhood up to the pubertal spurt in both genders, while the predictive power of T is only strong during puberty and here especially in girls. The correlation of W with BA is moderately positive and higher in boys than in girls up to puberty. Thereafter, it steadily diminishes. M shows first a weak positive correlation with BA which then turns to weak negative at puberty in both genders.
Correlations of T, W, M and L with height are shown in Fig. 4a. L shows a strong positive correlation with height in both genders throughout growth. In girls, W shows a stronger correlation with height than T does, while in boys the correlations of T and W with height are approximately equal and at an intermediate level between W and T in girls.
Correlations with weight (Fig. 4b) show overall less spread between the four metacarpal parameters than correlations with height. W correlates more with weight than T does in both genders. The correlation with L rises above the others in boys before and through puberty.
Discussion
The present study reports the reference values for T, W, L and M from the First Zurich Longitudinal Study in relation to BA, CA and height. In the following, these parameters are primarily discussed in relation to BA, with which they correlate better overall than with CA (Fig. 2).
The prepubertal dip
The slowing down in growth of T in both genders (and of L and W in boys) from around BA 7 (CA 6) in boys and BA 8 (CA 6) in girls up to puberty, shown in Table 1 and Fig. 2, has already been described by Gasser for height in relation to CA in the same children [7]. We have to date found no indication as to the mechanism underlying this “prepubertal dip”, which is relatively more pronounced with regards to changes in T than to height velocity. In boys, the subsequent increase in T is largely attributable to periosteal expansion and is thus associated with a strong increase in W. It is thought to be regulated by testosterone directly (via the androgen receptor) as well as by growth hormone (GH) and insulin-like growth factor [18], but also secondarily through the increase in muscle peak force [19]. From BA 15 onwards, growth in T is reinforced by endosteal apposition also in boys (Tables 1 and 2; Fig. 2). In girls, the increase in T results more from endosteal bone formation, whereas periosteal apposition is inhibited. Both these effects are attributed to oestrogen [18]. There appear to have been no investigations of the endocrine mechanisms underlying endosteal apposition in boys. A report on the effects of GH treatment on metacarpal dimensions also measured with BoneXpert in 178 prepubertal growth hormone-deficient children is given in [20] on the background of the present reference data.
The upper BA range
Towards the end of the BA range, Fig. 2a shows a decrease in W and M in both genders and in L in girls, as well as an undiminished increase in T in both genders, all of which manifest themselves only versus BA but not versus CA or height. These phenomena are attributable to the bias that results from the accumulation of subjects at the high end of the BA range. BA bins 18 and 19 and female BA bins 17 and 18 are overpopulated with early maturers due to the exclusion of all X-rays taken after CA 18.5 in girls and CA 19.5 in boys. These X-rays were from late maturers who were still growing at cutoff age. The strong downward deviation of W and M at BA 19 in boys and BA 18 in girls cannot be accounted for by the moderate degree of acceleration (CA 18.4 ± 0.7 years in the BA 19 bin for boys and 17.2 ± 1.0 years in the BA 18 bin for girls) in these early maturers alone. At least for boys the data suggest that on approaching skeletal maturity, children with accelerated development typically show reduced subperiosteal apposition and increased endosteal apposition, and this is not only for BA but also for CA.
However, this does not explain why so few from the BA 18 bin in boys enter the BA 19 bin and why this effect is also observable in girls in the BA 17 and 18 bins (Table 1). We attribute this to BoneXpert’s inability to distinguish reliably between these two BA bins. This has no effect on its BA rating reliability and precision in the intended ranges of BA 3 to 17 in boys and 3 to 15 in girls (the Tanner–Whitehouse BA system has the same upper age limit). It was decided not to exclude any BA bins beyond the intended range, since this would have produced bias effects in CA-based analyses also within the approved range. Besides, being biased towards early maturers, these BA bins are instructive in themselves, as discussed above. We recommend using the CA-based reference values for persons with a BA above the intended application range of BoneXpert.
Gender dimorphism
A comparison between the sexes shows that already from BA 6 onwards boys have significantly wider metacarpals than girls, even during the female pubertal spurt (Table 1; Fig. 2). By BA 18, W is around 15% greater in boys. W is a stronger manifestation of sexual dimorphism than height, which is on average around 8% greater in males by maturity.
Our findings on W are in good agreement with Bonnard’s [5]. Bonnard’s data are from a subset of the children included in the present study, but starting at 3 months age. A direct comparison of our raw data with those of Bonnard and Garn was not possible due to methodological differences. Thickness and width were measured by Bonnard at the smallest diameter of metacarpals 2–4 and by Garn at the midshaft of metacarpal 2 [8], which tends to be the largest. BoneXpert averages T and W over a 25% section of metacarpals 2–4, as described in the “Materials and methods” section. These methodological differences should nevertheless permit the study of inter-gender differences and of relative changes in the course of skeletal growth.
Initially there is no significant difference between the sexes with respect to length and thickness. Girls’ metacarpals become longer than boys’ from BA 9 on and thicker from BA 11 on. Boys first catch up on metacarpal length, around BA 13–14, and approximately one bone age year later on metacarpal thickness. This mirrors the progress of the correlations of L, T and W with BA shown in Fig. 3, as discussed below.
Our data concur with Garn’s observation that relative variability in W and T is greater in girls and show this to be true of all four parameters and particularly of M. Garn took the greater variability in girls to be an indicator of X chromosome involvement and a dosage effect in skeletal maturation [8].
Our finding that M begins to decrease earlier in girls than in boys (Fig. 3) is in agreement with Garn’s observations in Ohio whites [8]. However, according to Garn, peak M is reached around CA 11 in girls and 15 in boys, while our data show this to occur around CA 11 girls and between CA 13 and 14 in boys. Garn reported the decrease from peak M until CA 18 to be ca. 6% in boys (3.82 ± 0.77 to 3.58 ± 0.92 mm) and ca. 16% in girls (3.27 ± 0.66 to 2.75 ± 0.72 mm), whereas in the children from the present study, it differs much less between the genders (10% in boys, 13% in girls).
T, W, L and M as indicators of maturity
T, W, L and M all show a better correlation with BA than with CA (Fig. 2), with r2 values the highest for L and the lowest for M in either case and for both genders. Per CA bin, the correlation between L and BA is continuously strong from infancy until puberty and only falls off during late puberty, whereas the correlation between T and BA is only strong during puberty, during which period it shows a clear time offset between girls and boys (Fig. 4). The correlation between W and BA progresses similarly to that between T and BA but without reaching as high values during puberty. In other words, the maturation of the RUS bones in both boys and girls is best reflected by L until puberty and by T during puberty.
Correlations with height and weight
Not surprisingly, L shows the strongest correlation with height by BA bin in either gender. Garn observed that subperiosteal apposition continues throughout adulthood in all bones whether load bearing or not [8]. We had speculated that W would show a strong correlation with body height, indicating that also non-load-bearing bones become wider in response to tall height. Surprisingly, Fig. 4a shows a marked difference between the genders here: Particularly girls appear to have wider metacarpals the taller they are. We have no explanation for this phenomenon. Figure 4b shows L to correlate with weight more in boys than in girls. As expected, this difference is the greatest from puberty onwards, when the correlation between height and weight is also stronger in boys. However, this offers no further explanation for the inter-gender difference in how W correlates with height.
We see many fields of inquiry opening up from this database. In the area of growth disorders, we have already been able to show that GH treatment of children with growth hormone deficiency leads to a strong and significant increase in T within the first year of treatment as a result of subperiosteal bone deposition [20]. Another field of interest, especially given the change in children’s activities attending the computer age, is the secular trend in anthropometric measures.
Conclusion
We have presented reference values for metacarpal T, W, L and M from Caucasian children who grew up in a healthy environment at a time when obesity did not skew normative data. Each correlates in a characteristic manner with bone age (better than with chronological age) in the course of skeletal maturation, indicating differential responses to hormonal changes during growth. T, W, L, M and bone age were all measured fully automatically by the BoneXpert programme. T (and W and L in boys) show a phase of attenuated growth from around bone age 7—the “prepubertal dip”—followed by accelerated growth in puberty. These reference data provide a basis for further research into skeletal development and the management of hormone therapies in children.
References
Boettcher J, Pfeil A, Rosholm A, Petrovitch A, Seidl BE, Malich A et al (2005) Digital X-ray radiogrammetry combined with semiautomated analysis of joint space widths as a new diagnostic approach in rheumatoid arthritis: a cross-sectional and longitudinal study. Arthritis Rheum 52:3850–3859
Mentzel HJ, Blume J, Boettcher J, Lehmann G, Tuchscherer D, Pfeil A et al (2006) The potential of digital X-ray radiogrammetry (DXR) in the assessment of osteopenia in children with chronic inflammatory bowel disease. Pediatr Radiol 36:415–420
van Rijn RR, Boot A, Wittenberg R, van der Sluis IM, van den Heuvel-Eibrink M, Lequin MH et al (2006) Direct X-ray radiogrammetry versus dual-energy X-ray absorptiometry: assessment of bone density in children treated for acute lymphoblastic leukaemia and growth hormone deficiency. Pediatr Radiol 36:227–232
Thodberg HH, van Rijn RR, Tanaka T, Martin DD, Kreiborg S (2009) A paediatric bone index derived by automated radiogrammetry. Osteoporos Int 21:1391–1400. doi:10.1007/s00198-009-1085-9
Bonnard GD (1968) Cortical thickness and diaphysial diameter of the metacarpal bones from the age of three months to eleven years. Helv Paediatr Acta 23:445–463
Prader A, Largo RH, Molinari L, Issler C (1989) Physical growth of Swiss children from birth to 20 years of age. First Zurich Longitudinal Study of growth and development. Helv Paediatr Acta Suppl 52:1–125
Gasser T, Kneip A, Binding A, Prader A, Molinari L (1991) The dynamics of linear growth in distance, velocity and acceleration. Ann Hum Biol 18:187–205
Garn SM (1970) The earlier gain and the later loss of cortical bone in nutritional perspective. Thomas, Springfield
Martin DD, Deusch D, Schweizer R, Binder G, Thodberg HH, Ranke MB (2009) Clinical application of automated Greulich–Pyle bone age determination in children with short stature. Pediatr Radiol 39:598–607
Thodberg HH, Kreiborg S, Juul A, Pedersen KD (2009) The BoneXpert method for automated determination of skeletal maturity. IEEE Trans Med Imaging 28:52–66
Thodberg HH (2009) An automated method for determination of bone age. J Clin Endocrinol Metab 94:2239–2244
van Rijn RR, Lequin MH, Thodberg HH (2009) Automatic determination of Greulich and Pyle bone age in healthy Dutch children. Pediatr Radiol 39:591–597
Martin DD, Sato K, Sato M, Thodberg HH, Tanaka T (2010) Validation of a new method for automated determination of bone age in Japanese children. Horm Res Paediatr 74:15–22
Martin DD, Neuhof J, Jenni OG, Ranke MB, Thodberg HH (2010) Automatic determination of left- and right-hand bone age in the First Zurich Longitudinal Study. Horm Res Paediatr 74:50–55
Thodberg HH, Jenni OG, Ranke MB, Martin DD (2010) Validation of bone age methods through prediction of final adult height. Horm Res Paediatr 73:398–404
Thodberg HH, Olafsdottir H (2003) Adding curvature to minimum description length shape models. British Machine Vision Conference 5, pp 14–16
Rosholm A, Hyldstrup L, Baeksgaard L, Grunkin M, Thodberg HH (2001) Estimation of bone mineral density by digital X-ray radiogrammetry: theoretical background and clinical testing. Osteoporos Int 12:961–969
Seeman E (2001) Sexual dimorphism in skeletal size, density, and strength. J Clin Endocrinol Metab 86:4576–4584
Frost HM, Schonau E (2000) The“muscle-bone unit” in children and adolescents: a 2000 overview. J Pediatr Endocrinol Metab 13:571–590
Martin DD, Heckmann C, Walter C, Ranke MB, Thodberg HH, Binder G (2010) Differentiation of growth hormone effects on metacarpal bone and bone age in children with growth hormone deficiency. Osteoporos Int (in press)
Acknowledgements
Julia Neuhof is thanked for her excellent work in scanning the ZLS X-ray films, Novo Nordisk for lending the Scanner, and Elisabeth Kaelin, Jon Caflisch and Luciano Molinari for the data and X-ray management of the ZLS.
Conflicts of interest
Hans Henrik Thodberg is the owner of Visiana, which holds and markets the BoneXpert medical device for automated determination of bone age. The other authors have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Martin, D.D., Heckmann, C., Jenni, O.G. et al. Metacarpal thickness, width, length and medullary diameter in children—reference curves from the First Zürich Longitudinal Study. Osteoporos Int 22, 1525–1536 (2011). https://doi.org/10.1007/s00198-010-1389-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-010-1389-9