Abstract
This prospective study assessed whether metacarpal indices predict fracture risk in children and adolescents. Radiogrammetry was performed at the second metacarpal midshaft on annual hand–wrist radiographs of 359 South African (SA) children aged 10–17 years. Bone length, bone width, and medullary width were measured, and the following proxies for bone strength calculated: metacarpal index (MCI), bone mineral density (BMD), section modulus (SM), stress–strain index (SSI), and slenderness index (SLI). Height and weight were measured annually. Self-reported physical activity (PA) and fracture history were obtained at ages 15 years (for the preceding 12 months) and 17 years, respectively. At 17 years, 82 (23%) participants (black, 16%; white, 42%; p < 0.001) reported a previous fracture. None of the bone measures or indices were associated with fracture in black participants. In white females, after adjusting for PA, a 1 standard deviation (SD) greater SLI doubled the fracture risk [odds ratio (OR) 2.08; 95% confidence interval (CI) 1.08, 3.98]. In white males, a 1 SD greater BMD was associated with a 2.62-fold increase in fracture risk (OR 3.62; 95% CI 1.22, 10.75), whilst a 1 SD greater SM (OR 2.29; 95% CI 1.07, 4.89) and SSI (OR 2.23; 95% CI 1.11, 4.47) were associated with a more than twofold increase in fracture risk, after height, and PA adjustment. No single index consistently predicted fracture across the four groups possibly due to ethnic and sex differences in bone geometry, muscle mass, and skeletal loading. Metacarpal radiogrammetry did not reliably predict fracture in SA children.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Childhood and adolescence is associated with a high incidence of fracture with at least 30% of children sustaining a fracture during this time [1,2,3,4]. Fractures in children occur predominantly during puberty, when there is dissociation between the ages of peak growth velocity and bone mineral accrual [5]. Compelling evidence exists for the antecedents of bone fragility in adulthood being established during the circumpubertal years [6,7,8]. Children who fracture are more inclined to fracture as adults [6, 9] and have evidence of reduced bone mineral density (BMD) and strength at previous fracture sites in adulthood [10].
The mechanical and functional properties of bone are a consequence of its morphological characteristics combined with tissue quality traits [11]. Biological constraints result in significant variation of these traits both within and across population groups [11]. Ethnic disparities in fracture incidence have been shown in US children [12]. In a South African (SA) study, a greater proportion of white (41%) than black (19%) children had fractured by age 15 years [3], despite white children having greater bone area and bone mineral content than their black peers after adjusting for differences in height and weight [3, 13]. The prevalence of fractures is also sex-specific, being greater in boys than girls [3, 4, 14]. Additionally, environmental factors such as physical activity (PA) and body mass index (BMI) independently contribute to variations in fracture incidence [13, 15].
Metacarpal bone characteristics measured by radiogrammetry have been used to predict fracture risk in adults [16,17,18] and children [18,19,20]. There have been conflicting reports on the reliability of this method even though the strength of the association between wrist and forearm fractures and metacarpal measures obtained by radiogrammetry have been shown to be comparable to dual energy X-ray absorptiometry (DXA) [19]. The aim of this study was to determine the association between various metacarpal indices and fracture risk in a cohort of SA children and adolescents. We hypothesised that irrespective of ethnicity or sex, metacarpal bone dimensions and indices would predict fracture risk.
Materials and Methods
Participants and Protocol
The participants were members of the Bone Health Cohort (BHC) which is a sub-cohort of the Birth to Twenty Cohort (Bt20) whose participant recruitment protocols have previously been described [21]. Briefly, Bt20 is a longitudinal child health study of 3273 singleton children born over a 6-week period in 1990 in the greater Soweto-Johannesburg metropolitan area, South Africa. Children were classified as black (African descent) or white (European descent) based on the race classification used in South Africa for demographic and restitution purposes. Ethnic classification was self-reported by the parents and only those children whose parents both belonged to the same ethnic group were included in this study. Genetic studies have shown little ethnic admixture between the groups in the Bt20 cohort [22]. At age 9 years, 563 of these children were included in the BHC to investigate factors affecting the acquisition of peak bone mass during adolescence. An additional 120 white children born in the same period as the original cohort were enrolled into the BHC to compensate for the small number of white participants, which represented the population demographics of South Africa at that time. Birth weight, socioeconomic status, and maternal age and education of the additional white participants were similar to those of the existing white children of the BHC. All participants were healthy; those taking medication known to affect bone metabolism were excluded from the study.
Measurements included weight, height, and hand–wrist X-rays, and each participant’s annual assessment was done at approximately the same time every year. The mean age and range at each annual assessment is presented in Supplementary Table 1.
Anthropometric Measurements
Weight and height of participants were measured whilst wearing light clothing and no shoes. Weight was measured to the nearest 100 g using a digital scale (Dismed, Miami, FL, USA) and height to the nearest millimetre using a stadiometer (Holtain, Crymych, UK). Quality control annual training and monitoring ensured a coefficient of variation between measurers of less than 2%. BMI was calculated as weight (kg)/height (m)2.
Radiography
Postero-anterior hand–wrist radiographs of the left hand were taken annually between 9 and 21 years of age by certified radiographers at the Charlotte Maxeke Academic Hospital in Johannesburg. The left hand was radiographed in all participants irrespective of hand dominance. The X-ray beam was focussed on the distal aspect of the third metacarpal of the left hand. Radiographs were taken using cassettes with single-emulsion film under standard conditions of tube to film distance of 76 cm and exposure at 42 kV and 12 mA/s, and processed in an automatic developer in accordance with the optimal conditions described by Tanner [23].
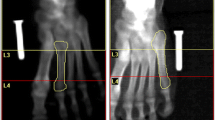
Radiogrammetry
The dimensions of the second metacarpal were measured on annual radiographs from 359 participants between the ages of 10 and 17 years. Measurements were carried out using digital vernier callipers calibrated to 0.01 mm and the following parameters were obtained in millimetres: Total length of bone from proximal to distal end (L), and outer bone width (D) and medullary inner width (d) at the midshaft of the bone. The cortical thickness was calculated as the difference between the bone width and medullary width (D − d). Using these measurements, the following indices were calculated: MCI = (D − d)/D [24], BMD = π(D − d) × [1 − ((D − d)/D)] [25], section modulus (SM) = π[(D4 − d4)/32]/0.5D [26], slenderness index (SLI) = (bone length × body weight)/SM [27], stress–strain index (SSI) = SM × volumetric BMD [28]. A single researcher (AM) performed all measurements. Intraobserver reliability of metacarpal measurements were (i) metacarpal length 0.14%, (ii) bone width 0.80%, and (iii) medullary width 6.20% [21]. Interobserver reliability was evaluated by comparing the metacarpal measurements for the 10-year age group against measurements performed on the same participants from this cohort in a previous study. The difference between the results of the two studies was less than 3% [29].
Fracture Questionnaire
Fracture history was obtained retrospectively at age 17 years. Participants completed a questionnaire with the assistance of their parent or caregiver. Information obtained included age at fracture, cause and site of fracture (with the aid of a skeletal diagram), by whom the fracture was diagnosed, whether radiographs were taken to confirm the fracture, and the treatment offered and performed. As our fracture data were collected retrospectively, the fractures could not be verified radiographically. Between 6 months and a year after completing the initial fracture questionnaire, 9% of the participants who were selected randomly, verified their fracture data telephonically. The grades of trauma causing fracture were classified as slight (grade 1), moderate (grade 2), and severe (grade 3) (Table 1) [3, 30]. Only those participants who had sustained fractures as a result of mild to moderate trauma were included in the analyses.
Physical Activity Levels
Self-reported PA was obtained at age 15 years for the preceding 12 months via an interviewer administered questionnaire which had been previously validated in a SA population [31]. Activities were categorized as formal (physical education, extra-mural school, and club sport) and informal (leisure time activities outside of the school or club environment). The duration of activity was recorded in minutes per week (min/week) and capped at 1680 min/week for informal activity. School and club sport were both capped at 1200 min/week.
Data Analysis
Cross-Sectional Data
Data for black and white participants were analysed separately because of differences between the two ethnic groups in anthropometry and bone mass measures obtained using radiogrammetry [21] and DXA [13]. Participants were categorized into yearly age groups for cross-sectional analyses. For example, age group 10 included participants aged between 10 and 10.9 years. Data were analyzed using STATA version 14 (Stata Corporation, Inc., College Station, TX, USA). A one-way ANOVA with a post-hoc Bonferroni multiple comparisons test (α level 0.05) was performed to determine sex and ethnic differences in fracture prevalence, and, in participant anthropometry, bone measures, bone indices, and PA levels. Participant height and BMI data were converted to Z-scores using the World Health Organisation Anthroplus software (http://www.who.int/growthref/tools/en). Black females were the largest group of non-fracturing participants and were, therefore, used as a reference group against which to compare the other groups’ bone measures, bone indices, and PA scores after converting the variables to Z-scores based on black female data. The Z-scores were calculated by subtracting the reference mean from each individual score and dividing by the reference standard deviation (SD). Student t-tests were used to determine differences in Z-score bone measures between participants with and without fractures within the four ethnic and sex groups. Bivariate logistic regression analyses were used to determine the associations between anthropometric measures, bone measures, and bone indices and fracture history at 17 years separately for each sex and ethnic group. Multivariate logistic regression analyses, adjusting for height and formal PA, were also performed to examine the same associations at 17 years. Statistical significance was set at p < 0.05 for all analyses.
Longitudinal Data
Correlation analysis was performed on height at each year from 10 until 16 years with MCI, BMD, SM, and SSI to determine the influence of participant height on each index at different ages.
To determine the association between bone measures and indices prior to the age of peak metacarpal length velocity (PLV) [21] and a history of fracture at 17 years, logistic regression analysis was performed for each bone measure and index for the combined sex and ethnic groups of participants at 10 years of age to determine the odds ratios (ORs) for fracture at 17 years after adjusting for height.
A generalized estimating equations (GEE) model was used to analyze the correlated data of the bone measures and indices with the binary outcome of fracture. The combined data of participants from both ethnic and sex groups from ages 10 until 16 years were assessed against the cumulative fracture incidence between 10 and 17 years. A binomial family with a logit link was specified in the model. An autoregressive correlation structure was deemed the most appropriate to minimize loss of statistical power for the repeated measures. ORs were calculated for the bone indices and the binary outcome of fracture. Statistical significance was set at p < 0.05.
Results
Participant recruitment and number of observations are shown in Fig. 1. A total number of 359 participants, aged between 10 and 17 years, had valid hand–wrist X-rays and had completed the fracture and PA questionnaires. Attrition of participants and participants missing data collection waves during the study were due either to time constraints, challenges with transportation, or to the circular migration of individuals between their extended family in urban and rural areas.
Fracture Incidence
The mean age on completion of the fracture questionnaire was 17.69 ± 0.25 years. Eighty-two (23%) of these individuals had sustained one or more fractures during their lifetime. The percentage of white females who had fractured was more than triple that of black females (40 vs. 12%), whilst the percentage of white males who had fractured was more than double that of black males (44 vs. 20%). Within ethnic groups, there were no significant sex differences in fracture prevalence. The sites of fracture and grades of trauma are presented in Table 2. Five participants, who had sustained a fracture due to a grade 3 level of trauma, were excluded from further analyses.
Cross-Sectional Data
Cohort Characteristics at Age 17 Years
Characteristics of participants of the cohort at age 17 years are presented in Table 3. At 17 years of age, black participants were significantly shorter than their white peers. Black and white females were of similar weight; however, black males were lighter than white males. Black females and males had thinner cortices, greater medullary widths, and hence a lower MCI than their white peers. Black and white females had shorter and narrower bones with smaller medullary cavities than their respective male peers. Females, therefore, had lower BMD, SM, and SSI than males. Females had more slender bones than males as reflected by their higher SLI. At 15 years, black participants engaged in significantly less formal PA than their white peers.
Comparison of Fracture and Non-fracture Groups
Comparisons of anthropometry, bone measures and indices between the fractured and non-fractured groups at age 17 years are presented in Table 4. The only anthropometric difference between those who had and had not fractured was in white females, with those who had fractured having a significantly higher BMI Z-score than those who had not (p = 0.04). Metacarpal length, bone width, and cortical thickness did not differ between those who had and had not fractured in black females, black males, and white females. However, white males who had fractured had wider bones (p = 0.03) and greater medullary widths (p = 0.02) than those without fractures. There were no differences in any of the bone indices between the fracture and non-fracture groups in black participants. In white participants, females who had fractured had a greater SLI than their non-fractured peers (p = 0.01), while males who had fractured had lower MCI and SLI but higher BMD, SM, and SSI than their non-fracturing peers.
Associations Between Anthropometric Characteristics and History of Fractures at Age 17 Years
Bivariate logistic regression analyses showed that in white females a 1 SD greater BMI Z-score was associated with a 93% increase in fracture risk (OR 1.93; 95% confidence interval, CI 1.01, 3.71) (Supplementary Table 2). None of the anthropometric measures were associated with fracture risk in the other three groups (Supplementary Table 2).
Associations Between Bone Measures and History of Fractures at Age 17 Years
Bivariate logistic regression analyses showed that in white males, a 1 SD greater bone width was associated with a 96% increase in fracture risk (OR 1.96; 95% CI 1.03, 3.72) (Supplementary Table 2). When adjusted for height and PA (Fig. 2), the OR increased to 2.77 (95% CI 1.09, 7.09). In the same group, the odds for fracture increased 2.2-fold with a 1 SD greater medullary width (OR 2.22; 95% CI 1.05, 4.69) (Supplementary Table 2), however, the association was no longer significant when adjusted for height and PA (Fig. 2). In the other three groups, none of the bone measures were associated with fracture risk.
Odds ratios for having a history of fracture, based on bone measures and indices at 17 years of age, after covarying for height and formal physical activity. Data are presented as odds ratios with 95% confidence intervals. TL total length, BW bone width, MW medullary width, MCI metacarpal index, CT cortical thickness, BMD bone mineral density, SM section modulus, SSI stress–strain index, SLI slenderness index. SLI covaried for formal physical activity only. Significant p-values < 0.05 are in bold
Associations Between Bone Indices and History of Fractures at Age 17 Years
Bivariate logistic regression analyses showed that in white females a 1 SD greater SLI was associated with a twofold increase in odds for fracture (OR 2.00; 95% CI 1.11, 3.61) (Supplementary Table 2). After adjusting for PA, the OR did not change (OR 2.08; 95% CI 1.08, 3.98; Fig. 2). In contrast, greater SLI in black females was associated with a reduced risk of fracture (OR 0.51; 95% CI 0.26, 1.00) (Supplementary Table 2), however, this was no longer significant when adjusted for PA (Fig. 2).
In white males, a 1 SD greater MCI was associated with a 55% decreased risk of fracture (OR 0.45; CI 0.20, 0.99) (Supplementary Table 2) which was no longer significant after adjusting for height and PA (Fig. 2). The bone indices BMD, SM, and SSI were associated with fracture risk in white males before and after adjusting for height and PA (Supplementary Table 2; Fig. 2). When adjusted for height and PA, a 1 SD greater BMD increased the risk of fracture threefold (OR 3.62; 95% CI 1.22, 10.75), and a 1 SD greater SM and SSI increased the odds of fracture by 129% (OR 2.29; 95% CI 1.07, 4.89) and 123% (OR 2.23; 95% CI 1.11, 4.47), respectively (Fig. 2).
Longitudinal Data
The bone indices BMD, SM, and SSI were moderately correlated with height at each year from age 10 until 16 years (r = 0.32–0.55) (Supplementary Table 3). There was no consistent relationship between MCI and height across the age range (Supplementary Table 3).
When the association between bone indices prior to PLV and adolescent fracture history were assessed, logistic regression showed that for the combined groups of participants, none of the bone indices measured at age 10 years significantly predicted fracture history at age 17 years (data not shown).
Longitudinal analyses of the bone measures and indices from ages 10 until 16 years and the odds of a positive fracture history by 17 years of age, before and after adjusting for height, using GEE for the combined groups are presented in Table 5. Increases in cortical thickness, MCI, and BMD were associated with decreases in fracture risk when unadjusted, but after adjusting for height, the relationships were reversed. When unadjusted, a 1 mm increase in cortical thickness between 10 and 16 years was associated with a 1% lower risk of fracture history at age 17 years (p = 0.03). A unit increase in MCI between ages 10 and 16 years resulted in a 9% decrease risk of fracture risk by age 17 years (p = 0.02), whilst a unit increase in BMD was associated with a 1% decreased risk of fracture by 17 years of age (p = 0.03) using unadjusted data. After adjusting for height, there was a slight increase in fracture risk by age 17 years for a unit increase in CT (p = 0.01), MCI (p = 0.02), and BMD (p = 0.01) between ages 10 and 16 years.
Discussion
Our study of SA children and adolescents from a longitudinal cohort comprising two ethnic groups assessed metacarpal bone measures and indices and their association with fracture risk during childhood and adolescence. We observed ethnic differences in fracture prevalence in the first 17 years of life, with substantially higher incidences in both white females and males relative to their black peers, consistent with results obtained at 10 and 15 years in the Bt20 cohort [13]. Similarly, ethnic differences in fracture incidence have previously been reported in SA adults in whom black individuals had a lower incidence of femoral neck fractures [32] even though their metacarpal BMD was lower than that of their white peers [33]. Whilst these studies taken together suggest that genetics may play a role in protecting against fracture, extrinsic factors which affect the attainment of peak bone mass may also contribute to the aetiology of skeletal fragility in late adulthood [6].
Fracture prevalence has been shown to be a function of bone geometry [34], thus geometric indices obtained by radiogrammetry such as the MCI and BMD, both of which reflect bone size and cortical thickness, have been the most widely used metacarpal indices to determine fracture risk [17, 19, 35]. Studies on both adults [16] and children [19] have shown a low MCI to be associated with a greater fracture risk. Even though we have previously shown that black children have thinner cortices relative to bone width [21], and hence a lower MCI than white children, we have also shown that they fractured less. In keeping with the above findings, our white males at 17 years of age who had a history of fracture had greater bone widths and wider medullary cavities, reflective of a lower MCI, than their non-fracturing peers. They also had a 55% decrease in fracture risk associated with a 1 SD gain in MCI, but this was negated when height and PA were considered. The group of white males with a history of fractures participated in more formal PAs, thus any biomechanical advantage provided by the geometrical organization of their bones may have been overridden by greater force at the time of injury. The finding that white males who fractured were taller, played more formal sport, and had greater DXA-derived bone mass has been previously reported from this cohort [13]. We have also shown that white males who had fractured had a higher BMD than their non-fracturing peers. In contrast, in Europe, a lower BMD was reported in adolescent males who had fractured compared to those who had not [18]. Our results indicate that a higher BMD does not entirely compensate for higher risk-taking activities.
In our study, although there were no sex differences in fracture prevalence (possibly because of the small numbers), black males had a lower MCI than their female counterparts, whereas white males and females who had not fractured had a similar MCI. In contrast, 17–18-year old females in Europe with no history of fracture had a higher MCI than their male peers [18]. Collectively, in addition to sex differences, these results also reflect population differences in bone geometry. In both the fractured and non-fractured participants, we also observed sex differences in radiogrammetry-derived BMD, which reflects the greater bone widths and cortices in males compared to females. These sex differences are consistent with the greater DXA-derived BMD at 15 years in males compared to females in this cohort [13]. A shortcoming of both radiogrammetry- and DXA-derived BMD is that they represent bone size rather than volumetric BMD which may be obtained by more advanced high-resolution computed tomography. The latter technique may also give insight into factors such as cortical porosity that may contribute to fracture.
Long bone fracture is primarily the result of bending or torsional stresses [36]. When we assessed SM and SSI which are surrogate strength indices based on moments of inertia, these indices were associated with fracture only in white males. We found that a greater SM and SSI increased fracture risk significantly, even after adjusting for height and PA. Our white males who fractured had greater bone width and medullary width, and hence reduced cortical thickness, resulting in a higher SM and SSI compared to their non-fractured peers. This outward displacement of the cortex from the neutral axis of the bone should have conferred a greater resistance to bending and torsional forces, and a reduced propensity to fracture [37]. This incongruity may be attributed to the overriding influence of higher levels of PA participation.
Our study and others have shown that metacarpal indices are influenced by height [38] which is a major determinant of bone size and mass [39]. In our cohort, at 17 years of age, there were no differences in height or metacarpal length between participants who had fractured and those who had not. This finding differs from results obtained at 15 years of age where white males of this cohort who fractured were taller than their non-fracturing peers [13], and may be related to differences in age of pubertal development and peak height velocity. An additional influencing factor may have been our sample size which was 23% smaller than that at 15 years. Taller individuals are at a greater risk for fracture despite their longer and wider bones with relatively thinner cortices [40]. In a twin study, the taller twins had increased fracture risk due to increased porosity of the cortex, despite their bone geometry offering greater resistance to torsional and bending forces [40].
Since height influences metacarpal indices, we assessed the SLI, which is also a proxy for bone strength, for its association with a history of fracture. The SLI, is an index based on moments of inertia which factors in body size, that is, the product of weight and bone length [27]. We showed that the SLI was associated with a history of fracture in white females only. Whilst our white females with a history of fracture had a greater SLI and hence more slender bones than their non-fractured peers, we also showed that after adjusting for PA, a 1 SD increase in SLI doubled the risk of fracture. Since body weight is used in the calculation of the SLI, the greater weight in white females who fractured may account for the association between the SLI and fracture in this group only. At both 15 and 17 years, white females in this cohort who fractured had greater fat mass [13] which supports the findings of Goulding and co-workers in New Zealand [41].
Bone mass measures in 8-year old children obtained by DXA have been reported to predict upper limb fracture during puberty [42], but this was not found in our study. Metacarpal indices of the combined sex and ethnic groups evaluated at 10 years, which is prior to the age of PLV in these participants [21], were of no value in predicting adolescent fracture. This suggests that external risk factors may play a greater role than measures of bone mass in the association with fracture. Bone mass measures have been shown to track from childhood through adolescence [7]. In our longitudinal analyses, we have shown that an increase in bone width and/or cortical thickness, as reflected by the MCI, is associated with a 9% reduction of fracture history risk at age 17 years in SA children. However, it is unclear for how many years from the time of measurement that the index has predictive value and prospective studies would be needed to elucidate this. Radiogrammetry-derived BMD, when assessed longitudinally, was only weakly associated with decreased adolescent fracture. We acknowledge a shortcoming of this study in that the timing of the fractures was not documented as they occurred; these data may have provided better correlation with the indices longitudinally.
A strength of this study is that it presents longitudinal data on radiogrammetry-derived metacarpal indices and their associations with fracture history in SA children of two ethnic groups. To the best of our knowledge, there are no other such studies. We were limited by the overall small number of white individuals, and relatively few black participants with a history of fracture, which may have resulted in the loss of statistical power. In this study, we considered it essential to stratify the participants by sex and ethnicity due to known differences in their bone geometry. Another limitation is that radiogrammetry only provides quantitative rather than qualitative information. Our metacarpal measurements were at the mid-diaphyseal region where the composition of bone differs from metaphyseal sites which have a higher trabecular content and are the most prevalent sites of fracture [43]. Fractures were not verified radiographically, though there was consistency with fracture reports obtained at ages 10, 13, and 15 years [13]. Self-reported fracture history has been shown to be relatively accurate, particularly for upper limb and hip fractures [44]. In this study, the cause, site, and grade of fracture were not assessed separately due to the small participant numbers, nor were data adjusted for potential modifiers of skeletal health. Previous studies on this cohort have shown that despite ethnic disparities in nutrition, 25-hydroxy vitamin D levels and socio-economic status, black children had greater bone mass than their white peers at most sites [29, 45]. We also did not adjust for lean mass or the possible influence of bone’s microstructural properties. We acknowledge that self-reported PA may be prone to recall bias, however, it is the most practical method to assess PA in a large longitudinal cohort.
In conclusion, metacarpal indices obtained at age 10 years, that is prior to the age of peak bone length velocity, did not predict fracture risk in SA adolescents. When the combined sex and ethnic groups were assessed longitudinally throughout adolescence, greater cortical thickness, MCI, and BMD were associated with a small decrease in fracture risk by age 17 years, but the opposite was seen when differences in height were adjusted for. At 17 years of age, the SLI was associated with fracture risk in white females, whereas greater bone width, BMD, SM, and SSI were associated with fracture risk in white males. There are ethnic and sex differences in the associations between radiogrammetry-derived metacarpal bone geometry measures and indices of moments of inertia with fracture in SA adolescents. We conclude that our study was unable to show that metacarpal radiogrammetry was reliably able to predict fracture in SA children, but this may possibly be due to sample size limitations.
References
Hedstrom EM, Svensson O, Bergstrom U, Michno P (2010) Epidemiology of fractures in children and adolescents. Acta Orthop 81:148–153
Clark EM (2014) The epidemiology of fractures in otherwise healthy children. Curr Osteoporos Rep 12:272–278
Thandrayen K, Norris SA, Pettifor JM (2009) Fracture rates in urban South African children of different ethnic origins: the Birth to Twenty cohort. Osteoporos Int 20:47–52
Cooper C, Dennison EM, Leufkens HG, Bishop N, van Staa TP (2004) Epidemiology of childhood fractures in Britain: a study using the general practice research database. J Bone Miner Res 19:1976–1981
Jones IE, Williams SM, Dow N, Goulding A (2002) How many children remain fracture-free during growth? A longitudinal study of children and adolescents participating in the Dunedin Multidisciplinary Health and Development Study. Osteoporos Int 13:990–995
Cooper C, Eriksson JG, Forsen T, Osmond C, Tuomilehto J, Barker DJ (2001) Maternal height, childhood growth and risk of hip fracture in later life: a longitudinal study. Osteoporos Int 12:623–629
Foley S, Quinn S, Jones G (2009) Tracking of bone mass from childhood to adolescence and factors that predict deviation from tracking. Bone 44:752–757
Baxter-Jones AD, Faulkner RA, Forwood MR, Mirwald RL, Bailey DA (2011) Bone mineral accrual from 8 to 30 years of age: an estimation of peak bone mass. J Bone Miner Res 26:1729–1739
Amin S, Melton LJ, Achenbach SJ, Atkinson EJ, Dekutoski MB, Kirmani S, Fischer PR, Khosla S (2013) A distal forearm fracture in childhood is associated with an increased risk for future fragility fractures in adult men, but not women. J Bone Miner Res 28:1751–1759
Farr JN, Khosla S, Achenbach SJ, Atkinson EJ, Kirmani S, McCready LK, Melton III LJ, Amin S (2014) Diminished bone strength is observed in adult women and men who sustained a mild trauma distal forearm fracture during childhood. J Bone Miner Res 29:2193–2202
Jepsen KJ (2011) Functional interactions among morphologic and tissue quality traits define bone quality. Clin Orthop Relat Res 469:2150–2159
Wren TA, Shepherd JA, Kalkwarf HJ, Zemel BS, Lappe JM, Oberfield S, Dorey FJ, Winer KK, Gilsanz V (2012) Racial disparity in fracture risk between white and nonwhite children in the United States. J Pediatr 161:1035–1040
Thandrayen K, Norris SA, Micklesfield LK, Pettifor JM (2011) Heterogeneity of fracture pathogenesis in urban South African children: the Birth to Twenty cohort. J Bone Miner Res 26:2834–2842
Mayranpaa MK, Makitie O, Kallio PE (2010) Decreasing incidence and changing pattern of childhood fractures: a population-based study. J Bone Miner Res 25:2752–2759
Clark EM, Ness AR, Tobias JH (2008) Vigorous physical activity increases fracture risk in children irrespective of bone mass: a prospective study of the independent risk factors for fractures in healthy children. J Bone Miner Res 23:1012–1022
Kiel DP, Hannan MT, Broe KE, Felson DT, Cupples LA (2001) Can metacarpal cortical area predict the occurrence of hip fracture in women and men over 3 decades of follow-up? Results from the Framingham Osteoporosis Study. J Bone Miner Res 16:2260–2266
Haara M, Heliovaara M, Impivaara O, Arokoski JP, Manninen P, Knekt P, Karkkainen A, Reunanen A, Aromaa A, Kroger H (2006) Low metacarpal index predicts hip fracture: a prospective population study of 3,561 subjects with 15 years of follow-up. Acta Orthop 77:9–14
Renz DM, Malich A, Ulrich A, Pfeil A, Mentzel HJ, Streitparth F, Maurer MH, Teichgraber UK, Bottcher J (2016) Reference values for digital X-ray radiogrammetry parameters in children and adolescents in comparison to estimates in patients with distal radius fractures. J Bone Miner Metab 34:55–64
Ma D, Jones G (2003) The association between bone mineral density, metacarpal morphometry, and upper limb fractures in children: a population-based case–control study. J Clin Endocrinol Metab 88:1486–1491
Jones G, Boon P (2008) Which bone mass measures discriminate adolescents who have fractured from those who have not? Osteoporos Int 19:251–255
Magan A, Nyati LH, Micklesfield LK, Norris SA, Pettifor JM (2017) Metacarpal growth during adolescence in a longitudinal South African cohort. J Bone Miner Res 32:1926–1934
May A, Pettifor JM, Norris SA, Ramsay M, Lombard Z (2013) Genetic factors influencing bone mineral content in a black South African population. J Bone Miner Metab 31:708–716
Tanner JM (2001) Assessment of skeletal maturity and prediction of adult height (TW3 method). W.B. Saunders, London
Dequeker J (1976) Quantitative radiology: radiogrammetry of cortical bone. Br J Radiol 49:912–920
Jorgensen JT, Andersen PB, Rosholm A, Bjarnason NH (2000) Digital X-ray radiogrammetry: a new appendicular bone densitometric method with high precision. Clin Physiol 20:330–335
Franklyn M, Oakes B, Field B, Wells P, Morgan D (2008) Section modulus is the optimum geometric predictor for stress fractures and medial tibial stress syndrome in both male and female athletes. Am J Sports Med 36:1179–1189
Tommasini SM, Nasser P, Schaffler MB, Jepsen KJ (2005) Relationship between bone morphology and bone quality in male tibias: implications for stress fracture risk. J Bone Miner Res 20:1372–1380
Cointry GR, Ferretti JL, Reina PS, Nocciolino LM, Rittweger J, Capozza RF (2014) The pQCT ‘Bone Strength Indices’ (BSIs, SSI). Relative mechanical impact and diagnostic value of the indicators of bone tissue and design quality employed in their calculation in healthy men and pre- and post-menopausal women. J Musculoskelet Neuronal Interact 14:29–40
Vidulich L, Norris SA, Cameron N, Pettifor JM (2006) Differences in bone size and bone mass between black and white 10-year-old South African children. Osteoporos Int 17:433–440
Manias K, McCabe D, Bishop N (2006) Fractures and recurrent fractures in children; varying effects of environmental factors as well as bone size and mass. Bone 39:652–657
McVeigh JA, Norris SA (2012) Criterion validity and test–retest reliability of a physical activity questionnaire in South African primary school-aged children. S Afr J Sports Med 24:43–48
Solomon L (1968) Osteoporosis and fracture of the femoral neck in the South African Bantu. J Bone Jt Surg Br 50:2–13
Solomon L (1979) Bone density in ageing Caucasian and African populations. Lancet 2:1326–1330
Taes Y, Lapauw B, Griet V, De Bacquer D, Goemaere S, Zmierczak H, Kaufman JM (2010) Prevalent fractures are related to cortical bone geometry in young healthy men at age of peak bone mass. J Bone Miner Res 25:1433–1440
Dey A, McCloskey EV, Taube T, Cox R, Pande KC, Ashford RU, Forster M, de Takats D, Kanis JA (2000) Metacarpal morphometry using a semi-automated technique in the assessment of osteoporosis and vertebral fracture risk. Osteoporos Int 11:953–958
Rubin CT, Lanyon LE (1982) Limb mechanics as a function of speed and gait: a study of functional strains in the radius and tibia of horse and dog. J Exp Biol 101:187–211
Bouxsein ML (2005) Determinants of skeletal fragility. Best Pract Res Clin Rheumatol 19:897–911
Martin DD, Heckmann C, Neuhof J, Jenni OG, Ranke MB, Binder G (2012) Comparison of radiogrammetrical metacarpal indices in children and reference data from the First Zurich Longitudinal Study. Pediatr Radiol 42:982–991
Faulkner RA, Davison KS, Bailey DA, Mirwald RL, Baxter-Jones AD (2006) Size-corrected BMD decreases during peak linear growth: implications for fracture incidence during adolescence. J Bone Miner Res 21:1864–1870
Bjornerem A, Bui QM, Ghasem-Zadeh A, Hopper JL, Zebaze R, Seeman E (2013) Fracture risk and height: an association partly accounted for by cortical porosity of relatively thinner cortices. J Bone Miner Res 28:2017–2026
Goulding A, Jones IE, Taylor RW, Manning PJ, Williams SM (2000) More broken bones: a 4-year double cohort study of young girls with and without distal forearm fractures. J Bone Miner Res 15:2011–2018
Flynn J, Foley S, Jones G (2007) Can BMD assessed by DXA at age 8 predict fracture risk in boys and girls during puberty? An eight-year prospective study. J Bone Miner Res 22:1463–1467
Meena S, Sharma P, Sambharia AK, Dawar A (2014) Fractures of distal radius: an overview. J Fam Med Prim Care 3:325–332
Hundrup YA, Hoidrup S, Obel EB, Rasmussen NK (2004) The validity of self-reported fractures among Danish female nurses: comparison with fractures registered in the Danish National Hospital Register. Scand J Public Health 32:136–143
Poopedi MA, Norris SA, Pettifor JM (2011) Factors influencing the vitamin D status of 10-year-old urban South African children. Public Health Nutr 14:334–339
Acknowledgements
The Bone Health Cohort (BHC) was supported financially by the Wellcome Trust (UK) and the South African MRC. JMP received funding from the National Research Foundation. SAN was supported by the DST-NRF Centre of Excellence in Human Development at the University of the Witwatersrand. The contribution of the BHC staff, participants and caregivers is gratefully acknowledged.
Author information
Authors and Affiliations
Contributions
Study design JMP, SAN, LKM, Analysis of Radiographs AM, Fracture data collection KT, Integrity of data AM and RJM, Data interpretation AM, LKM, JMP, RJM, Drafting and revising manuscript- AM, LKM, SAN, KT, RJM, JMP.
Corresponding author
Ethics declarations
Conflict of interest
Ansuyah Magan, L.K. Micklesfield, S.A. Norris, K. Thandrayen, R.J. Munthali, and J.M. Pettifor declare no conflict of interest.
Human and Animal Rights and Informed Consent
This study was approved by the University of the Witwatersrand Committee for Research on Human Subjects and was performed in accordance with the Ethical Standards as laid down in the 1964 Declaration of Helsinki and its later amendments. Informed assent from adolescent participants and consent from parents were obtained for inclusion in this study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Magan, A., Micklesfield, L.K., Norris, S.A. et al. Metacarpal Indices and Their Association with Fracture in South African Children and Adolescents. Calcif Tissue Int 104, 14–25 (2019). https://doi.org/10.1007/s00223-018-0467-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-018-0467-4