Abstract
Summary
The Osteoporosis Risk Factor and Prevention-Fracture Prevention Study (OSTPRE-FPS) was a randomized population-based open trial (n = 593). The supplementation group (n = 287) received daily cholecalciferol 800 IU + calcium 1,000 mg for 3 years while the control group (n = 306) received neither supplementation nor placebo. Daily vitamin D and calcium supplementation have a positive effect on the skeleton in ambulatory postmenopausal women.
Introduction
Vitamin D deficiency is common in the elderly, and vitamin D levels are associated with low bone mineral density (BMD). The working hypothesis was that vitamin D and calcium supplementation could prevent bone loss in ambulatory postmenopausal women.
Methods
The OSTPRE-FPS was a randomized population-based open trial with a 3-year follow-up in 3,432 women (aged 66 to 71 years). A randomly selected subsample of 593 subjects underwent BMD measurements. The supplementation group (n = 287) received daily cholecalciferol 800 IU + calcium 1,000 mg for 3 years while the control group (n = 306) received neither supplementation nor placebo.
Results
In the intention-to-treat analysis, total body BMD (n = 362) increased significantly more in the intervention group than in the control group (0.84% vs. 0.19%, p = 0.011). The BMD change differences at the lumbar spine (p = 0.372), femoral neck (p = 0.188), trochanter (p = 0.085), and total proximal femur (p = 0.070) were statistically nonsignificant. Analyses in compliant women (≥80% of use) resulted in stronger and statistically significant effects at the total body and femoral regions.
Conclusion
Daily vitamin D and calcium supplementation have a positive effect on the skeleton in ambulatory postmenopausal women with adequate nutritional calcium intake.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Serum levels of 25-hydroxyvitamin D (25[OH]D) are directly related to bone mineral density (BMD) [1]. Calcium absorption decreases from digestive tract when 25(OH)D levels are inadequate (<75 nmol/l) [2]. Accordingly, low 25(OH)D leads to bone resorption and bone loss and thus increased risk of fracture [1, 3–5]. Vitamin D deficiency is common in the elderly since the capacity of the skin to synthesize provitamin decreases with age [6]. Low vitamin D status is prevalent in elderly women living in northern latitudes [7], but this deficiency can also be detected in young adults in northern Europe [8] and in the housebound elderly [9]. It is believed that in order to achieve an optimal vitamin D level of >75 nmol/l one should consume between 800 and 1,000 IU of vitamin D everyday [10].
In a recent meta-analysis, calcium alone and calcium with vitamin D were associated with reduced bone loss at the hip and spine [11]. In another study, the effect of vitamin D and calcium was nonsignificant at the spine and in the total body [12]. Dawson-Hughes et al. reported that the combined supplementation had no effect on proximal femur in a 3-year follow-up [13]. However, an increase of femoral BMD during a shorter 18-month follow-up has also been reported [5]. Chapuy et al. reported a lower rate of annual bone loss at the proximal femur with combined supplementation [14], but in a recent trial, vitamin D treatment alone had no bone effect [15]. These controversial findings could be partly explained by variations in dosages and different intervals between dosings [16]. In addition, different forms of vitamin D and the heterogeneity of study populations might confound the results.
There is still no definitive answer about how vitamin D and calcium supplementation can influence bone status, and in particular, there are no population-based trials to settle the issue. In this 3-year population-based Osteoporosis Risk Factor and Prevention Study-Fracture Prevention Study (OSTPRE-FPS) randomized trial, we hypothesized that vitamin D and calcium supplementation might be able to reduce bone loss in ambulatory postmenopausal women over the age of 65. The open population-based approach demonstrates the effect of the intervention in the general population, in comparison with the situation in women who simply continue their normal diet, perhaps using nonprescription sources of vitamin D and calcium supplementation.
Subjects and methods
Study design and participants
This study was based on the OSTPRE-FPS which began in 2003 in Kuopio, Finland. The primary aim of the study was to determine whether vitamin D and calcium supplementation would be effective in preventing falls and fractures in postmenopausal women. The Ethics Committee of Kuopio University Hospital approved the OSTPRE-FPS study in October 2001. Written informed consent was collected from the study participants at the baseline enquiry.
The targeted OSTPRE-FPS population (n = 5,407) was selected from the population-based OSTPRE cohort (n = 13,100) of women born in 1932–1941 [17]. The inclusion criteria for OSTPRE-FPS were age at a minimum of 65 years at the end of November 2002, living in the Kuopio Province at the onset of the trial, and not belonging to the former OSTPRE bone densitometry sample. The willingness to participate in a calcium and vitamin D trial was enquired via a postal enquiry between August and December 2002. The 3,432 volunteers out of 5,407 (63.5%) were randomized into two groups of equal size without stratification or random allocation sequence by an independent statistician. The subjects were assigned to their groups by postal notification according to the randomization. OSTPRE-FPS was conducted as an open-label trial. The power analysis was done based on incidence of fractures. There was no a priori power analysis to calculate the size of the subsample.
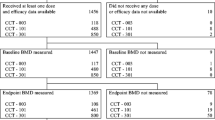
In the entire trial population, the intervention and control groups had 1,718 and 1,714 subjects, respectively. A subsample of 750 women was randomly selected from the 3,432 women at the baseline. In the subsample, the supplementation and control groups had both 375 subjects. The subsample underwent a detailed measurement program including the BMD and serum 25(OH)D measurements. The baseline measurements took place between February 2003 and May 2004 and the follow-up measurement between January 2006 and May 2007 (mean (SD) follow-up time 2.8 (0.4) years). Between the randomization and the actual start of the intervention, 237 subjects withdrew, and ten were lost during the follow-up. At the end of the trial, 306 and 287 subjects in intervention and control groups of the subsample, respectively, completed the follow-up (Fig. 1).
Baseline characteristics
The baseline postal questionnaire included questions about health disorders, medication, duration of hormone therapy (HT; years), gynecological history, calcium questionnaire (milligram per day, the total dietary calcium was calculated as summing up calcium derived from dairy products (cheese, milk, sour milk, yogurt, sour whole milk), juices including calcium and supplements (both prescription and natural products)), physical activity (type of activity and duration in hours per week), alcohol consumption (one alcohol unit was based on calculation that one bottle of beer has been estimated to contain 12 g and one glass of wine (12 cl) and hard liquor (4 cl) 14 g of absolute alcohol), and smoking (present status). The time since menopause (years) was calculated using the self-reported beginning of amenorrhea at baseline. In Eastern Finland, 75% of dietary calcium has been estimated to come from dairy products [18]. The self-reported calcium intake has been validated, and it showed moderate correlation against the 4-day food record [18]. The medications possibly affecting bone metabolism included corticosteroids, diuretics, cytotoxic drugs, anticonvulsive drugs, anabolic steroids, calcitonin, bisphosphonates, and vitamin D. Weight was measured with a digital calibrated scale (Phillips, type HF 351/00) and height with a calibrated wall meter.
Intervention
The intervention group obtained daily cholecalciferol 800 IU and calcium carbonate 1,000-mg supplementation (Calcichew-D3 Forte, Leiras-Nycomed Ltd.) divided into two daily doses for 3 years, and the control group received no supplementation. The vitamin D and calcium was a combined formula that was chewable, and subjects took it twice a day. Both groups were asked to continue with their previous diet. The supplements were distributed via prescriptions which were written and supervised by one of the authors (MT), and local pharmacies arranged the distribution of the supplements. The prescriptions were written for 1-year period at the beginning of the trial. The pharmacies contacted one of the authors (MT) once a year to renew the prescriptions. The pharmacies provided the supplements for 3 months at a time for the subjects of the intervention group. Compliance was calculated as the percentage of the delivered tablets of predicted consumption during the follow-up period.
Main outcome measure
BMD measurements were performed at the lumbar spine (L2–L4), left proximal femur, and total body with dual X-ray absorptiometry (DXA; Lunar Prodigy, GE, Madison, WI, USA) twice, at the baseline and at the end of the trial. The regions of interest at the proximal femur included femoral neck, trochanter, Ward’s triangle, and total proximal femur. The four vertebrae between L1 and L4 (n = 395) were used in the analyses, and whenever it was not possible (e.g., degenerative changes), we substituted it with any two or three consecutive vertebrae between L1 and L4 (n = 85). The phantom control of the DXA instruments was run daily. The in vitro long-term reproducibility (CV) for total femur region was 0.3%. The technical quality of each DXA measurement and analysis was carefully checked, and those with measurement errors were not included in the statistical analyses.
Serum 25(OH)D measurements
Blood samples (n = 593) were obtained in a nonfasting state at the baseline and the 3-year follow-up visits. Serum was frozen, and all 25(OH)D samples were analyzed promptly after the study closure. Serum 25(OH)D was determined by radioimmunoassay method using 25(OH)D RIA kit from DiaSorin (Stillwater, MN, USA). Total variation (CV%) for the Diasorin method was from 8.2% to 11.0% according to the manufacturer.
Statistical analysis
Data were analyzed on an intention-to-treat basis by retaining groups according to randomization (Fig. 1; SPSS, version 14.0.1; SPSS, Chicago, IL, USA). Differences between the intervention and control groups were analyzed with independent-samples t test for normally varied and with the Mann–Whitney test for nonnormally varied variables. Pearson chi-square test was used for the univariate analyses of category variables. The change in BMD within the group was defined with paired-samples t test. The difference of change of BMD between the groups was defined with general linear repeated-measures model. The results are presented time × treatment interaction from the repeated-measures analysis of variance. The differences of vitamin D levels and change between the groups were analyzed with independent-samples t test. All analyses were unadjusted. The secondary analysis was performed in adherent women (i.e., those who took at least 80% of their supplementation). Associations between serum 25(OH)D level, total calcium intake at the baseline, and the annual BMD change were analyzed with linear regression model.
Results
The characteristics of the study population at the baseline are shown in Table 1. All differences between the intervention and control groups were nonsignificant. There were no statistically significant differences between the entire study population and the subsample (data not shown).
Main outcome results
Table 2 shows the change in BMD during the trial. Total body BMD increased significantly more in the intervention group than in the control group (0.84% vs. 0.19%, p = 0.011). The BMD decrease at Ward’s triangle was lower in the intervention group (−2.69% vs. −2.83%, p = 0.003). The BMD changes at the spine (p = 0.372), femoral neck (p = 0.188), trochanter (p = 0.085), and total proximal femur (p = 0.070) were statistically nonsignificant between the groups.
Secondary outcome results
The mean compliance was 79%. The proportions for 70%, 80%, and 90% compliance were 71.8%, 63.8%, and 47.4% of the intervention group, respectively.
The women who were adherent (i.e., those who took at least 80% of their supplementation) showed significantly lower bone loss in femoral neck (−1.26% vs. −1.73%, p = 0.002), Ward’s triangle (−1.63% vs. −2.83%, p < 0.0001), trochanter (0.25% vs. −0.88%, p = 0.001), and total proximal femur (−0.84% vs. −1.47%, p < 0.0001) than in the control group. Further, total body BMD increased more in the intervention group (+1.31% vs. +0.19%, p = 0.002). In contrast, lumbar spine bone loss was greater in the intervention group than in the control group (+0.67% vs. +0.76%, p = 0.033; Table 3).
Baseline serum 25(OH)D associated with Ward’s triangle annual BMD change (p = 0.033), but it did not associate with trochanter (p = 0.726), total hip (p = 0.845), proximal femur (p = 0.099), lumbar spine (p = 0.060), or total body (p = 0.343) annual BMD change.
The total intake of calcium at the baseline did not predict annual BMD change at Ward’s triangle (p = 0.497), trochanter (p = 0.665), total hip (p = 0.720), proximal femur (p = 0.339), lumbar spine (p = 0.729), or total body (p = 0.668).
Serum 25(OH)D level
The mean (SD) baseline serum 25(OH)D levels were 50.1 (18.8) nmol/l and 49.2 (17.7) nmol/l in the intervention and control groups (p = 0.544), respectively. The absolute changes in 25(OH)D levels were 24.7 (24.1) nmol/l and 6.8 (19.3) nmol/l in the intervention and control groups (p < 0.001), respectively. At the end of the trial, the mean levels were 74.6 (21.9) nmol/l and 55.9 (21.8) nmol/l (p < 0.001), respectively.
Adverse effects of the supplementation
In total, 40 out of 290 women discontinued the intervention: 17 due to adverse effects, 22 due to other reasons, and one due to no specific reason. The adverse effects responsible for discontinuation were gastrointestinal symptoms (nine), exacerbation of diseases (two), and mouth irritation (one), skin symptoms (one), nausea (one), cough (one), backache (one), and weight increase (one).
Discussion
The daily cholecalciferol 800 IU and calcium carbonate 1,000-mg supplementation increased the total body BMD in women aged 66 to 71 years in this randomized 3-year population-based trial. However, no site-specific changes at the femoral region or at the lumbar spine were detected in the main analyses. In further analyses, the intervention effect appeared to be greater in total body and femoral regions among women who adhered to the supplementation.
It has been reported earlier that there is a progress of about 1% annual bone loss in the femoral neck in the elderly [19]. Furthermore, inadequate intakes of vitamin D and calcium lead to reduced calcium absorption, higher bone remodeling rates, and increased bone loss [3, 14]. The combination of these factors increases the risk of osteoporosis and consequently the risk for osteoporotic fractures. There is evidence to suggest that adequate sunlight exposure and the use of supplements are needed to meet human vitamin D needs [20]. Vitamin D supplementation has been shown to have long-term effects on the skeleton as a whole [13]. Similarly, the positive effect on total body BMD that was seen in this study may reflect the general skeletal effect. However, we cannot exclude the possibility that total body and spinal BMD increase could be confounded because of age-related degenerative changes, such as osteoarthritis and aortic calcification [21, 22]. On the other hand, vitamin D and calcium supplementation may have stronger effect on cortical bone [23]. Consequently, the positive effect seen in the total body BMD might be explained by higher proportion of cortical bone in the skeleton.
In a large RCT trial, 1,000 mg daily calcium alone showed 1.6% smaller bone loss in hip over 5-year follow-up in elderly women [24]. The relatively small changes detected in BMD between the supplemented and control groups in the present and earlier studies raise the question of the clinical relevance of the positive results. At the population level, the supplementation would not be sufficient to prevent osteoporosis, but it could at least decelerate the age-related bone loss to some extent. Additional nonpharmacological and pharmacological interventions should be considered, especially in subjects at a high risk of suffering osteoporotic fractures [25]. Dawson-Hughes et al. have reported that 1.1% net increase in total body BMD during the 3-year vitamin D (700 IU) and calcium (500 mg) trial was associated with relative risk of 0.4 of first osteoporotic fracture [13]. Accordingly, in our study, BMD increase of 0.9% but with slightly greater dose of vitamin D (800 IU) and calcium (1,000 mg) might point out for similar relative risk reduction.
Daily oral dosing with vitamin D seems to be a more effective way of administration than weekly or monthly ones [16]. However, recent study demonstrated the effect of large vitamin D loading and intermittent dosages to normalize serum levels [26]. Furthermore, vitamin D supplementation is effective in preventing the seasonal-related vitamin D level decrease and subsequent bone loss [27, 28]. In fact, vitamin D sufficiency might be more important than high calcium intake to maintain desirable serum parathyroid hormone levels [29]. BMD improvements in the vitamin D and calcium-supplemented subjects are largely lost if the supplementation is discontinued [30]. This is in agreement with the present study where women who were adherent had the most benefit from the supplementation. These findings argue in favor of the importance of regularity in the supplementation. Further, vitamin D supplementation supports other therapies, since optimal vitamin D repletion is necessary for achieving the maximal benefits from antiresorptive pharmacological therapies [31].
There is evidence of an age-related intestinal resistance to the actions of 1,25-dihydroxyvitamin D [32]. Accordingly, this has led to the question about the sufficiency of daily 1,000-mg calcium intake even in the old age. It is known that calcium absorption increases with higher vitamin D levels [2], and accordingly optimal calcium intake in people with adequate vitamin D status might be lower [33]. Nonetheless, it has been suggested that the vitamin D requirement is not greatly dependent on calcium intake [34], and a daily intake of 1,200 mg calcium in the general population should cover calcium needs [11, 34]. In the present study, the mean daily intake of calcium was 980 mg at baseline, which is nearly at the current Finnish recommendation (1,000 mg/day). Thus, the high nutritional calcium intake might have suppressed the positive effect of the supplementation. Further, recent findings suggest that calcium supplementation is associated with adverse cardiovascular events [35, 36]. Thus, the recommendation for supplying additional calcium for those subjects with a nutritional supply of over 1,000 mg needs to be evaluated in further studies. More studies are needed to study whether daily vitamin D confer additional health benefits.
Mean serum 25(OH)D levels were 50 nmol/l, which suggests that subjects were slightly deficient in terms of vitamin D [20]. In fact, it has recently been reported that only women with 25(OH)D levels below 50 nmol/l benefit from a higher calcium intake [37]. Therefore, we suggest that the positive effect of the supplementation might be attributable to greater extent to the adequate vitamin D intake than calcium intake. This is further supported by the earlier finding that BMD increases with higher 25(OH)D concentrations [37]. Since February 2003, following the recommendation by the Finnish Ministry of Social Affairs and Health, fluid milks (0.5 mg/100 ml), margarines, and spreads (10 mg/100 g) have been fortified by vitamin D in Finland. Indeed, this action in general has improved the mean vitamin D intake and status in Finland, but low 25(OH)D levels still occur [38].
The strengths of this study were its population-based design and the long follow-up. However, as only two thirds of individuals volunteered to participate (3,432 out of 5,407), the population-based benefit was diminished. The subsample of 593 women was randomly selected from those 3,432 subjects, and therefore it is a representative cohort. One limitation was that the compliance with the intended intervention was not complete (79% of the prescribed calcium–vitamin D tablets that were dispensed from the pharmacies). However, the present compliance was quite similar as in the previous study [12]. Further, the compliance was estimated based on prescriptions and not on exact count of tablets consumed. Since vitamin D and calcium supplementations are available over the counter and are routinely included in standard multivitamins, the subjects in the control group might well have increased their use of calcium and vitamin D supplementation. In fact, 3.8% of control subjects reported using prescribed vitamin D with or without calcium supplements at baseline, but this has risen to 16.1% by the end of the trial (data not shown). However, serum 25(OH)D levels increased significantly more in the intervention group (24.7 nmol/l) than in the control group (6.8 nmol/l). This confirms that women in the intervention group had used the study supplementation. The open population-based approach demonstrates the effect of the intervention in the general population, in comparison with the situation in women who simply continue their normal diet perhaps using nonprescription sources of vitamin D and calcium supplementation.
In conclusion, combined daily cholecalciferol 800 IU and calcium carbonate 1,000 mg has a positive effect on the skeleton in ambulatory postmenopausal women with adequate mean nutritional calcium intake. Whether there is effect without calcium supplementation needs to be confirmed in future studies.
References
Bischoff-Ferrari HA, Giovannucci E, Willet WC, Dietrich T, Dawson-Hughes B (2006) Estimation of optimal serum concentrations of 25-hydroxyvitamin D for multiple health outcomes. Am J Clin Nutr 84:18–28 [Erratum, Am J Clin Nutr 2006;84:1253]
Heaney RP, Dowell MS, Hale CA, Bendich A (2003) Calcium absorption varies within the reference range for serum 25-hydroxyvitamin D. J Am Coll Nutr 22:142–146
Lips P (2001) Vitamin D deficiency and secondary hyperparathyroidism in the elderly: consequences for bone loss and fractures and therapeutic implications. Endocr Rev 22:477–501
Larsen ER, Mosekilde L, Foldspang A (2004) Vitamin D and calcium supplementation prevents osteoporotic fractures in elderly community dwelling residents: a pragmatic population-based 3-year intervention study. J Bone Miner Res 19:370–378
Chapuy MC, Arlot ME, Duboeuf F, Brun J, Crouzet B, Arnaud S, Delmas PD, Meunier PJ (1992) Vitamin D3 and calcium to prevent hip fractures in elderly women. N Engl J Med 327:1637–1642
Venning G (2005) Recent developments in vitamin D deficiency and muscle weakness among elderly people. BMJ 330(7490):524–526
Margiloff L, Harris SS, Lee S, Lechan R, Dawson-Hughes B (2001) Vitamin D status of an outpatient clinic population. Calcif Tissue Int 69(5):263–267
Lamberg-Allardt CJ, Outila TA, Karkkainen MU, Rita HJ, Valsta LM (2001) Vitamin D deficiency and bone health in healthy adults in Finland: could this be a concern in other parts of Europe? J Bone Miner Res 16(11):2066–2073
Gloth FM 3rd, Gundberg CM, Hollis BW, Haddad JG Jr, Tobin JD (1995) Vitamin D deficiency in homebound elderly persons. JAMA 274(21):1683–1686
Dawson-Hughes B, Heaney RP, Holick MF, Lips P, Meunier PJ, Vieth R (2005) Estimates of optimal vitamin D status. Osteoporos Int 16:713–716
Tang BM, Eslick GD, Nowson C, Smith C, Bensoussan A (2007) Use of calcium or calcium in combination with vitamin D supplementation to prevent fractures and bone loss in people aged 50 years and older: a meta-analysis. Lancet 370:657–666
Jackson RD, LaCroix AZ, Gass M, Wallace RB, Robbins J, Lewis CE, Bassford T, Beresford SA, Black HR, Blanchette P, Bonds DE, Brunner RL, Brzyski RG, Caan B, Cauley JA, Chlebowski RT, Cummings SR, Granek I, Hays J, Heiss G, Hendrix SL, Howard BV, Hsia J, Hubbell FA, Johnson KC, Judd H, Kotchen JM, Kuller LH, Langer RD, Lasser NL, Limacher MC, Ludlam S, Manson JE, Margolis KL, McGowan J, Ockene JK, O’Sullivan MJ, Phillips L, Prentice RL, Sarto GE, Stefanick ML, Van Horn L, Wactawski-Wende J, Whitlock E, Anderson GL, Assaf AR, Barad D, Women’s Health Initiative Investigators (2006) Calcium plus vitamin D supplementation and the risk of fractures. N Engl J Med 354(7):669–683
Dawson-Hughes B, Harris SS, Krall EA, Dallal GE (1997) Effect of calcium and vitamin D supplementation on bone density in men and women 65 years of age or older. N Engl J Med 337:670–676
Chapuy MC, Pamphile R, Paris E, Kempf C, Schlichting M, Arnaud S, Garnero P, Meunier PJ (2002) Combined calcium and vitamin D3 supplementation in elderly women: confirmation of reversal of secondary hyperparathyroidism and hip fracture risk: the Decalyos II study. Osteoporos Int 13(3):257–264
Zhu K, Bruce D, Austin N, Devine A, Ebeling PR, Prince RL (2008) A randomized controlled trial of the effects of calcium with or without vitamin D on bone structure and bone related chemistry in elderly women with vitamin D insufficiency. J Bone Miner Res 23(8):1343–1348
Chel V, Wijnhoven HAH, Smit JH, Ooms M, Lips P (2008) Efficacy of different doses and time intervals of oral vitamin D supplementation with or without calcium in elderly nursing home residents. Osteoporos Int 19:663–671
Honkanen R, Alhava EM, Saarikoski S, Tuppurainen M (1991) Osteoporosis risk factors in perimenopausal women. Calcif Tissue Int 49(Suppl):S74–75
Honkanen R et al (1996) Does lactose intolerance predispose to low bone density? A population-based study of perimenopausal Finnish women. Bone 19:23–28
Jones G, Sambrook P, Kelly PJ, Eisman JA (1994) Progressive loss of bone in the femoral neck in elderly people: longitudinal findings from the Dubbo osteoporosis epidemiology study. BMJ 309:691–695
Holick MF (2007) Vitamin D deficiency. N Engl J Med 357(3):266–281
Jones G, Nguyen T, Sambrook P, Kelly PJ, Eisman JA (1994) Progressive loss of bone in the femoral neck in elderly people: longitudinal findings from the Dubbo osteoporosis epidemiology study. BMJ 309:691–695
Greenspan SL, Maitland LA, Myers ER, Krasnow MB, Kido TH (1994) Femoral bone loss progresses with age: a longitudinal study in women over age 65. J Bone Miner Res 9:1959–1965
Daly RM, Bass S, Nowson C (2006) Long-term effects of calcium-vitamin-D3-fortified milk on bone geometry and strength in older men. Bone 39(4):946–953
Reid IR, Mason B, Horne A, Ames R, Reid HE, Bava U, Bolland MJ, Gamble GD (2006) Randomized controlled trial of calcium in healthy older women. Am J Med 119:777–785
Roux C, Bischoff-Ferrari HA, Papapoulos SE, de Papp AE, West JA, Bouillon R (2008) New insights into the role of vitamin D and calcium in osteoporosis management: an expert roundtable discussion. Curr Med Res Opin 24(5):1363–1370
Bacon CJ, Gamble GD, Horne AM, Scott MA, Reid IR (2009) High-dose oral vitamin D3 supplementation in the elderly. Osteoporos Int 20:1407–1415
Dawson-Hughes B, Dallal GE, Krall EA, Harris S, Sokoll LJ, Falconer G (1991) Effect of vitamin D supplementation on wintertime and overall bone loss in healthy postmenopausal women. Ann Intern Med 115(7):505–512
Meier C, Woitge HW, Witte K, Lemmer B, Seibel MJ (2004) Supplementation with oral vitamin D3 and calcium during winter prevents seasonal bone loss: a randomized controlled open-label prospective trial. J Bone Miner Res 19:1221–1230
Steingrimsdottir L, Gunnarsson O, Indridason OS, Franzson L, Sigurdsson G (2005) Relationship between serum parathyroid hormone levels, vitamin D sufficiency, and calcium intake. JAMA 294(18):2336–2341
Dawson-Hughes B, Harris SS, Krall EA, Dallal GE (2000) Effect of withdrawal of calcium and vitamin D supplements on bone mass in elderly men and women. Am J Clin Nutr 72:745–750
Adami S, Giannini S, Bianchi G, Siningaglia L (2009) Vitamin D status and response to treatment in post-menopausal osteoporosis. Osteoporos Int 20(2):239–244
Ireland P, Fordtran JS (1973) Effect of dietary calcium and age on jejunal calcium absorption in humans studied by intestinal perfusion. J Clin Invest 52:2672–2681
Bischoff-Ferrari HA (2007) How to select the doses of vitamin D in the management of osteoporosis. Osteoporos Int 18:401–407
Dawson-Hughes B, Bischoff-Ferrari HA (2007) Therapy of osteoporosis with calcium and vitamin D. Suppl 22:V59–63
Bolland MJ, Barber PA, Doughty RN, Mason B, Horne A, Ames R, Gamble GD, Grey A, Reid IR (2008) Vascular events in healthy older women receiving calcium supplementation: randomized controlled trial. BMJ 336:262–266
Pentti K, Tuppurainen MT, Honkanen R, Sandini L, Kröger H, Alhava E, Saarikoski S (2009) Use of calcium supplements and the risk of coronary heart disease in 52–62-year-old women: the Kuopio osteoporosis risk factor and prevention study. Maturitas 63(1):73–78
Bischoff-Ferrari HA, Kiel DP, Dawson-Hughes B, Orav JE, Li R, Spiegelman D, Dietrich T, Willett WC (2009) Dietary calcium and serum 25-hydroxyvitamin D status in relation to bone mineral density among U.S. adults. J Bone Miner Res 24(5):935–942
Lamberg-Allardt C, Viljakainen H & Working Group. Follow-up study on the vitamin D status in the Finnish population 2002 and 2004. In Reports of the Ministry of Social Affairs and Health, Helsinki, Finland 2006: Ministry of Social Affairs and Health, pp 1–49
Acknowledgements
We thank Ms. Seija Oinonen for technical support and Dr. Ewen MacDonald for linguistic check and local pharmacies for drug delivery. Supported by Finnish Cultural Foundation (Hulda Tossavainen Foundation; M.K.), Sigrid Juselius Foundation (H.K.), Academy of Finland (M.T. and J.S.), Kuopio University Hospital EVO grant, and Leiras-Nycomed Ltd. for the calcium and vitamin D supplementation. The study result has been presented at the 54th Nordic Orthopedic Federation Congress, June 11–13, 2008, Amsterdam, Netherlands.
Conflicts of interest
None.
Authors’ contributions
Author M.K. had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Authors M.T., R.H., E.A., and H.K. designed the study and directed its implication. Authors M.K., K.S., L.S., R.H., and H.K. analyzed and interpreted the data. Author K.S. helped to prepare the materials and methods section. Author M.K. drafted the manuscript. Authors M.T., K.S., T.R., J.S., R.H., J.A., E.A., and H.K. made critical revision of the manuscript for the important intellectual content.
Author information
Authors and Affiliations
Corresponding author
Additional information
The trial has been registered in Clinicaltrials.gov at identifier NCT00592917 (registration date: January 2nd 2008).
Rights and permissions
About this article
Cite this article
Kärkkäinen, M., Tuppurainen, M., Salovaara, K. et al. Effect of calcium and vitamin D supplementation on bone mineral density in women aged 65–71 years: a 3-year randomized population-based trial (OSTPRE-FPS). Osteoporos Int 21, 2047–2055 (2010). https://doi.org/10.1007/s00198-009-1167-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-009-1167-8