Abstract
Summary
This study evaluates the effect of zoledronic acid (ZOL) on the osseointegration of titanium implants in rabbits with glucocorticoid (GC)-induced bone loss, and our findings demonstrated that a single dose of ZOL is able to reverse the detrimental effects of GCs on the osseointegration of titanium implants.
Introduction
The purpose of this study is to evaluate the effect of ZOL on the osseointegration of titanium implants in rabbits with GC-induced bone loss.
Methods
Three groups of six NZW rabbits were treated for 18 weeks with saline (SALINE), GC (methylprednisolone, 0.35 mg/kg three times a week), or GC + ZOL (methylprednisolone + single dose of ZOL, 0.1 mg/kg). The animals received a titanium implant in the left tibia after 6 weeks and were killed at the 18th week. Bone mineral density (BMD) was measured with dual-energy X-ray absorptiometry at baseline, eighth week (W8), and 18th week (W18) after treatment to determine the change upon treatment (∆BMD). Histomorphometric and serum bone alkaline phosphatase analysis (BAP) were also performed.
Results
At W8, GC group had a significant reduction in lumbar spine and tibia BMD compared with SALINE (p = 0.003 and p = 0.000), as also observed for GC + ZOL group (p = 0.014 and p = 0.003) just 2 weeks after ZOL treatment. In contrast, at W18, the GC + ZOL had an evident BMD rescue with similar lumbar spine and tibia ∆BMD compared with SALINE (0.043 ± 0.006 vs. 0.055 ± 0.009 g/cm2, p = 0.457 and 0.027 ± 0.003 vs. 0.041 ± 0.011 g/cm2, p = 0.232) and a significantly higher ∆BMD compared with the GC (p = 0.024 and p = 0.001). Histomorphometry revealed that osseointegration was significantly reduced in GC (tibia cortical thickness and diameter, bone-implant contact, total and peri-implant bone area) whereas GC + ZOL had these parameters similar to SALINE (p > 0.05). Likewise, ZOL reversed the BAP alteration induced by GC.
Conclusions
Our findings demonstrated that a single dose of ZOL is able to reverse the detrimental effects of glucocorticoids on the osseointegration of titanium implants, suggesting that ZOL therapy may improve the outcome of bone implants in patients with glucocorticoid-induced osteoporosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osseointegration is defined as “a direct structural and functional connection between ordered living bone and the surface of a load-carrying implant”, originally meant to describe the biological fixation of titanium dental implants [1]. The loosening of an implant due to failure of osseointegration has been associated with biomaterial, biomechanical, and biological factors [2, 3]. In addition, conditions that interfere with bone metabolism, such as systemic disorders that adversely affect wound healing, may decrease the potential for successful osseointegration [4–6]. Systemic drugs, including those routinely used to treat rheumatological conditions, may also influence the osseointegration of titanium implants [7, 8].
Glucocorticoid (GC) therapy is an important treatment for the symptoms of chronic inflammatory diseases [9]. The general use of this drug has been connected to osteoporosis in humans, since it initially increases bone resorption and subsequently it mainly reduces bone formation and bone turnover [10]. This condition is a known risk factor for implant loosening, since it seems to affect the process of implant osseointegration [11]. Experiments in ovariectomized rats have demonstrated that osteoporosis causes a delay in bone healing around implants [12, 13].
Recently, the bisphosphonate zoledronic acid (ZOL) has been approved for the treatment of osteoporosis due to its beneficial effect on bone mass [14, 15]. This drug has a high affinity for hydroxyapatite and binds directly to mineralized bone [16]. In canine models, zoledronic acid enhances bone growth into porous implants [17] and prevents periprosthetic bone loss, which is a direct cause of aseptic loosening in total hip arthroplasty [18]. Similarly, locally applied bisphosphonates have been shown to improve implant fixation in osteopenic ovariectomized animals [16]. However, no study has investigated the efficacy of ZOL in promoting titanium implant osseointegration in glucocorticoid-induced osteoporosis (GIO). We therefore used a rabbit experimental model to evaluate whether a single intravenous dose of ZOL could improve the osseointegration of titanium implants under the osteoporotic conditions induced by GC therapy.
Material and methods
Animal protocol
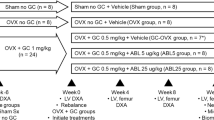
The Animal Ethics Committee of COBEA (Brazilian College of Experimental Animals) approved all experimental procedures in accordance with the guidelines set by UFAW (The Universities Federation for Animals Welfare). Eighteen male New Zealand adult rabbits 16 weeks old weighing 2.670 ± 0.067 kg [19] were divided into three groups of six rabbits each. All groups were treated for 18 weeks: the control group (SALINE) received saline (0.3 ml, SC) three times per week, the GC received methylprednisolone (0.35 mg/kg, SC) three times a week [20, 21], and the GC + ZOL group received GC with the same treatment schedule along with a single dose of ZOL (0.1 mg/kg, IV) at sixth week [22]. The animals were kept in individual cages with food and water ad libitum and were weighed weekly for drug administration. Blood was collected from ear vein at entry and at 18th week (W18) for biochemical analysis.
Endosseous implant model
Surgery was performed at sixth week. The animals were anesthetized intramuscularly with a mixture of xylazine (5 mg/kg) and ketamine (50 mg/kg). After trichotomy, the skin was cleansed and an incision of approximately 2 cm was made, exposing the bone by blunt dissection. A unicortical implant bed was prepared and a screw-type pure titanium implant [23] with rough surface (porosity of 1–2 μm), 8.5 mm in length, and 3.75 mm in diameter (Conexão Sistema de Protese Ltd., porous implant treated with acid twice through electrochemical deposition) was placed until the screw thread was completely introduced perpendicularly into the bone cortex. Soft tissues were replaced and sutured. A single dose of enrofloxacin was administrated at the time of the surgery, and analgesic oral drugs (dipyrone) were given for the first 3 days of the postoperative period.
Densitometric evaluation by dual-energy X-ray absorptiometry
Bone density was measured by dual-energy X-ray absorptiometry with a densitometer (QDR 2000 Hologic, Waltham, MA, USA) in high-resolution mode, using the “small animals” software supplied by the equipment manufacturer. The technique was standardized by positioning the anesthetized rabbits so that the lumbar spine (vertebrae L4–L5) and the proximal portion of the non-operated (right) tibia could be analyzed, and the region of interest was defined as the same where the implant was inserted but in the contralateral tibia. The first assessment was performed on the first day of the experiment, the second at the eighth week (2 weeks after the implant surgery), and the third at end of the treatment (18th week). Results are expressed as mean ± SE of BMD variation (∆BMD).
Bone alkaline phosphatase analysis
Bone alkaline phosphatase (BAP) was measured using a commercially available enzyme immunoassay (Quidel Corporation, San Diego, CA, USA). This assay utilizes a monoclonal anti-BAP antibody coated on a microtiter plate to capture BAP in the samples. The enzyme activity of the captured BAP is detected with a pNPP substrate.
Analysis of bone parameters
After the animals were killed (18th week), the left tibia (implanted) and right tibia (non-operated) were removed and fixed in 4% neutral buffered formalin for 14 days. The specimens were prepared for non-decalcified histology [24]. Briefly, pieces were washed in running water for 24 h, dehydrated in an ascending series of ethanol (40% to 100%), and subsequently embedded in methyl metacrylate blocks. Sections (80 μm) were obtained and stained with toluidine blue. Bone cortical thickness, tibia size (diameter), ratio of bone to implant contact, total bone area of tibia section, and peri-implant bone density were analyzed by light microscopy. Images were captured and digitized with Image Pro Plus 6 (Media Cybernetics, Bethesda, MD, USA).
The cortical thickness (micrometer) was determined as the mean of multiple measurements of the non-operated right tibia performed at each 30 μm of tibia perimeter (Fig. 1b, red line). To evaluate tibia size, the mean of three diameter measurements of the non-operated tibia (centimeter) using magnifying lens was determined (Fig. 1d, arrow).
a Effect of saline (SALINE), glucocorticoid (GC), and GC plus zoledronic acid treatment (GC + ZOL) on tibia cortical thickness (micrometer) at 18th week (W18). Results are expressed as mean ± SE. *p < 0.05 comparison with saline group (SALINE). #p < 0.05 comparison with GC + ZOL. b Non-operated tibia stained with toluidine blue. The red line indicates tibia thickness measurement (original magnification ×10). c Effect of SALINE, GC, and GC + ZOL on tibia size (diameter, micrometer) at 18th week (W18). Results are expressed as mean ± SE. *p < 0.05 comparison with SALINE. d Photomicrographs of the non-operated tibia with arrow indicating the diameters measurement (original magnification ×4)
Osseointegration was observed by direct bone (toluidine blue-stained) deposition on the implant surface (in black) without any other detectable tissue interposed, as judged via light microscopy. The total bone area of tibia section was evaluated through a software device which determines the bone tissue stained with toluidin blue (BT) present in the total area of tibia + implant (TA, square micrometer; Fig. 2a) and expressed as percent of bone area = BT/TA × 100, [25]. Osseointegration was also evaluated by point-counting technique [26]. Briefly, the bone density (i.e., the proportion of mineralized bone in a 500-µm-wide zone lateral to the implant (yellow rectangle)) was obtained bilaterally in the cortical passage of the implants and expressed as percentage of mineralized bone (Fig. 2b). Additionally, the ratio of bone to implant contact was calculated by the measurement of total perimeter of the implant (TPI) and the measurement of all osseointegrated spaces around the implant (OSI; red line in Fig. 2c) obtained manually and expressed as percent bone to implant contact (% = OSI/TPI × 100).
a Histomorphometric appearance of a titanium implant perpendicularly inserted in the left tibia of a SALINE-injected rabbit (original magnification ×4). b Histomorphometric appearance of the peri-implant bone density (the proportion of mineralized bone in a 500-µm-wide zone lateral to the implant (yellow rectangle). ct connective tissue, mb mineralized bone. c Bone to implant contact measurement (red line) of the left tibia (original magnification ×40). d Effect of saline (SALINE), glucocorticoid (GC), and GC plus zoledronic acid treatment (GC + ZOL) on the percentage of total bone area, peri-implant bone density, and bone to implant contact at 18th week (W18). Results are expressed as mean ± SE. *p < 0.05 comparison with SALINE. #p < 0.05 comparison with GC + ZOL. Data of bone to implant contact was analyzed by Mann–Whitney test
Statistical analysis
Results are expressed as mean ± SE. The results were analyzed by repeated measured ANOVA and compared with a student Newman Keul’s test. Non-parametric data were analyzed by the Mann–Whitney test. The chosen level of significance was 0.05.
Results
General outcomes
The final mean body weight gain was comparable in the three groups (SALINE, 0.925 ± 0.190 kg; GC, 0.550 ± 0.080 kg; GC + ZOL, 1.000 ± 0.120 kg; p = 0.067). No adverse gastrointestinal effects (vomiting or diarrhea) or surgical complications (mortality, infection, or wound dehiscence) were observed.
BMD variation
Initial lumbar spine and tibia mean BMD values were comparable in experimental groups (SALINE, 0.268 ± 0.008 and 0.371 ± 0.012 g/cm2; GC, 0.268 ± 0.011 and 0.376 ± 0.008 g/cm2; GC + ZOL, 0.291 ± 0.006 and 0.369 ± 0.009 g/cm2; p = 0.113 and p = 0.845). As expected, during the course of the experiment, the SALINE group showed an increase in lumbar ∆BMD values (0.033 ± 0.007 g/cm2) at W8 and (0.055 ± 0.009 g/cm2) at W18 (Fig. 3a). Similar results were registered in the tibia, with a ∆BMD (0.033 ± 0.011 g/cm2) at W8 and (0.041 ± 0.011 g/cm2) at W18 (Fig. 3b). In contrast, compared with SALINE, GC treatment caused a significant reduction in ∆BMD lumbar spine at W8 (−0.008 ± 0.008 g/cm2, p = 0.003) that was maintained until W18 (−0.004 ± 0.012 g/cm2, p = 0.003; Fig. 3a). Likewise, tibia ∆BMD values compared with SALINE were reduced (−0.019 ± 0.006 g/cm2, p = 0.000) at W8 and (−0.018 ± 0.010 g/cm2, p = 0.002) at W18 (Fig. 3b).
a Lumbar BMD variation (Δ BMD = final BMD − initial BMD). White columns represent BMD variation at eighth week (W8); hatched columns represent BMD variation at 18th week (W18). b Tibial BMD variation (Δ BMD = final BMD − initial BMD). White columns represent BMD variation at W8; hatched columns represent BMD variation at W18. Results are expressed as mean ± SE. *p < 0.05 comparison with SALINE. #p < 0.05 by comparison with: glucocorticoid plus zoledronic acid group (GC + ZOL)
A single dose of ZOL given intravenously at the moment of the surgery promoted a complete rescue of BMD loss at the final evaluation (W18) in the GC + ZOL group. The ∆BMD values of lumbar spine and tibia recorded in the GC + ZOL group were similar to those of the SALINE group (0.043 ± 0.006 vs. 0.055 ± 0.009, p = 0.457 and 0.027 ± 0.003 vs. 0.041 ± 0.011, p = 0.232) and significantly higher than those of the GC group (0.043 ± 0.006 vs. −0.004 ± 0.012, p = 0.024 and 0.027 ± 0.003 vs. −0.018 ± 0.010, p = 0.001; Fig. 3a and b). Data of ∆BMD in lumbar spine and tibia of GC + ZOL group recorded in W8 (only 2 weeks after ZOL treatment) did not differ from those obtained in GC group at the same time (Fig. 3a and b)
BAP analysis
Data showed that in adult rabbits during final growth period GC induces a more relevant reduction in ΔBAP (final–initial) compared with SALINE (−60.77 ± 8.89 vs. −39.78 ± 2.86 U/L, p = 0.05). The addition of ZOL to GC treatment resulted in a significantly lower ΔBAP compared with GC (−34.71 ± 4.06 vs. −60.77 ± 8.89 U/L, p = 0.03), and comparable values to SALINE group (−34.71 ± 4.069 vs. −39.78 ± 2.86 U/L, p = 0.34).
Histomorphometric analysis
A significant improvement in tibial cortical thickness at W18 was observed in the GC + ZOL group compared with the GC group (122.00 ± 1.87 vs. 98.81 ± 2.28 μm, p = 0.001) although the values were lower than those of the SALINE group (122.00 ± 1.87 vs. 133.08 ± 2.36 μm, p = 0.003; Fig. 1a). GC treatment promoted reduction of tibia diameter when compared with SALINE group (0.750 ± 0.045 vs. 0.805 ± 0.031 cm, p = 0.032; Fig. 1c). The addition of ZOL to GC treatment partially reversed tibia diameter (0.777 ± 0.049 cm); however, this data did not achieve significance (p = 0.381; Fig. 1c).
Figure 2d summarizes data of osseointegration measurements. The percent of total bone area of tibia section was reduced in the GC group compared with the SALINE group (p = 0.012). The GC + ZOL group demonstrated a complete reversion of this loss and had values comparable to those of the SALINE group (p = 0.187) and higher values than those of the GC group (p = 0.015). The percentage of peri-implant bone density was significantly lower in GC group compared with SALINE and GC + ZOL groups (p = 0.006 and p = 0.05, respectively). Reinforcing this finding, the percent bone-implant contact was significantly lower in the GC group than in the SALINE group (p = 0.008), whereas, a single injection of ZOL resulted in values comparable to SALINE group (p = 0.584), and a considerable increase in this parameter compared with the GC group (p = 0.023; Fig. 2d).
Discussion
The experiments described in this paper demonstrate that a single intravenous dose of zoledronic acid is able to reverse the deleterious effects of GC treatment on bone and titanium implant osseointegration.
Our novel approach of evaluating the osseointegration of implants in animals with established GIO is distinct from that of previous studies that have focused on the osteoporosis-preventing effects of biphosphonate [27]. Our design has the advantage to reproduce the clinical conditions observed in rheumatologic patients more accurately. GIO is observed in as many as 30–50% of patients receiving chronic glucocorticoid therapy [28], one third of whom will develop fractures [29]. Moreover, most previous animal protocols have used supra-therapeutic doses of glucocorticoid precluding a definitive conclusion about their clinical relevance [30]. The dose used herein was the one commonly used for patients with rheumatoid arthritis and related conditions. The efficacy of this dose in inducing bone abnormalities was demonstrated in previous reports using rabbits [20, 21].
Notably, GC is the most common cause of secondary osteoporosis. The frequency of GC use is relatively high, reaching 0.5% of the general population and 1.75% of women aged 55 or older [31–34]. Interestingly, GIO has same distinct features with postmenopausal osteoporosis, including the mechanism underlying bone loss and the occurrence of fractures at higher BMD levels [35, 36]. The risk of fracture is greatly increased in patients undergoing this therapy, with an odds ratio of 6.2 for vertebral fracture in the women with RA compared with age-matched women from a population-based group [37].
The present study design using the histological criteria of osseointegration is therefore the first to specifically evaluate the effect of zoledronic acid treatment on implants in animals with glucocorticoid-compromised bone, given that preceding reports used estrogen-deficient animal models [16, 27, 38]. In fact, histomorphometry of GIO bone has distinct characteristics, with a dominant decrease in cancellous bone and reduced bone turnover [39] supported by our finding of a more relevant ΔBAP in GC group compared with SALINE.
We have confirmed and extended the prior observation that GC also induces cortical thinning [11] and demonstrated that GIO animals have a reduced percentage of bone tissue around the implant and significantly less bone-implant contact than normal animals, which may ultimately affect implant osseointegration [40]. The relevance of the histological observation of direct bone contact is emphasized by the recent review which suggests that this phenomenon is not the result of a valuable biological tissue response but instead the lack of a negative tissue response [41]. Consistent with this finding, it is known that local reactions affecting bone-surface contact are a common feature of aseptic implant loosening [42].
Zoledronic acid is a potent bisphosphonate that suppresses bone turnover and increases bone mineral density with a consequent reduction in vertebral and non-vertebral fractures [43]. A recent multicentric study demonstrated that ZOL is as effective as risedronate for the prevention and treatment of bone loss in patients undergoing GC treatment [44]. Moreover, it was also reported that ZOL has additional beneficial effects on bone mineralization by promoting osteoblast differentiation and protein synthesis [45–47] and by enhancing osteoblastogenesis [48]. Our data of ZOL reversion of BAP alteration induced by GC supports the bone formation activity of zoledronic acid and its use in this condition. Reinforcing this finding, the reduced ponderal growth in animals treated with GC is probably not due solely to the catabolic effect in muscle [49, 50], but also to a direct effect in bone mass [30] that was improved by ZOL.
The lack of this effect in 2 weeks (W8) is an expected result since in this short period zoledronic acid may not completely reverse the bone loss promoted by GC treatment. In fact, the reduction of serum alkaline phosphatase after a single-dose zoledronate in healthy dogs was not observed from baseline on days 21 and 28 [51]. The same data was described for humans with no reduction in serum alkaline phosphatase in the 14-day postinfusion [52].
On the other hand, our study demonstrates that a single infusion of zoledronic acid in GIO animals seems to be very effective in W18, a beneficial effect also described in the literature using local implant application of zoledronic acid in ovariectomized rats [16, 38]. Since zoledronic acid is a well-established therapeutic agent for the treatment of osteoporosis, successful bone implants would be expected without the need of local ZOL application in many patients currently receiving ZOL therapy.
In summary, a single dose of zoledronic acid reverts glucocorticoid-induced bone loss and supports the stable integration of the host bone and implant in our animal model. These promising results suggest that a therapeutic strategy including ZOL treatment may improve the outcome of bone implants in patients with glucocorticoid-induced osteoporosis.
References
Branemark PI, Grondahl K, Branemark BK (2005) Why osseointegration would work and how it did in the first patients treated. Basic facts and philosophical thoughts. The osseointegration book: from calvarium to calcaneus, chapter 3, 1st edn. Quintessenz, Berlin
LeGeros RZ, Craig RG (1993) Strategies to affect bone remodeling: osteointegration. J Bone Miner Res 8:583–596
el Askary AS, Meffert RM, Griffin T (1999) Why do dental implants fail? Part I. Implant Dentistry 8(2):173–185
Lugero GG, Caparbo VF, Guzzo ML, Konig B, Jorgetti V (2000) Histomorphometric evaluation of implants in osteoporotic rabbits. Implant Dent 9:303–309
Von Wowern N (2001) General and oral aspects of osteoporosis: a review. Clin Oral Investig 5:71–82
Sakakura CE, Giro G, Gonçalves D, Pereira RM, Orrico SR, Marcantonio E Jr (2006) Radiographic assessment of bone density around integrated titanium implants after ovariectomy in rats. Clin Oral Impl Res 17:134–138
Duarte PM, Nogueira Filho GR, Sallum EA, de Toledo S, Sallum AW, Nociti Júnior FH (2001) The effect of an immunosuppressive therapy and its withdrawal on bone healing around titanium implants. A histomorfometric study in rabbits. J Periodontol 10:1391–1397
Beikler T, Fleming TF (2003) Implants in the medically compromised patient. Crit Rev Oral Biol Med 4:305–316
Morand EF (2007) Effects of glucocorticoids on inflammation and arthritis. Curr Opin Rheumatol 19(3):302–307
Woolf AD (2007) An update on glucocorticoid-induced osteoporosis. Curr Opin Rheumatol 19:370–375
Keller JC, Stewart M, Roehm M, Schneider GB (2004) Osteoporosis-like bone conditions affect osseointegration of implants. Int J Oral Maxillofac Implants 19(5):687–694
Yamazaki M, Shirota T, Tokugawa Y, Motohashi M, Ohno K, Michi K, Yamaguchi A (1999) Bone reactions to titanium screw implants in ovariectomized animals. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 87(4):411–418
Motohashi M, Shirota T, Tokugawa Y, Ohno K, Michi K, Yamaguchi A (1999) Bone reactions around hydroxyapatite-coated implants in ovariectomized rats. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 87(2):145–152
Recker RR, Delmas PD, Halse J, Reid IR, Boonen S, García-Hernandez PA, Supronik J, Lewiecki EM, Ochoa L, Miller P, Hu H, Mesenbrink P, Hartl F, Gasser J, Eriksen EF (2008) Effects of intravenous zoledronic acid once yearly on bone remodeling and bone structure. J Bone Miner Res 23:6–16
Brown JE, Ellis SP, Lester JE, Gutcher S, Khanna T, Purohit OP, McCloskey E, Coleman RE (2007) Prolonged efficacy of a single dose of the bisphosphonate zoledronic acid. Clin Cancer Res 13:5406–5410
Gao Y, Zou S, Liu X, Bao C, Hu J (2009) The effect of surface immobilized bisphosphonates on the fixation of hydroxyapatite-coated titanium implants in ovariectomized rats. Biomaterials 30(9):1790–1796
Bobyn JD, Hacking SA, Krygier JJ, Harvey EJ, Little DG, Tanzer M (2005) Zoledronic acid causes enhancement of bone growth into porous implants. J Bone Joint Surg Br 87:416–420
Wise LM, Waldman SD, Kasra M, Cheung R, Binnington A, Kandel RA, White LM, Grynpas MD (2005) Effect of zoledronate on bone quality in the treatment of aseptic loosening of hip arthroplasty in the dog. Calcif Tissue Int 77(6):367–375
Masoud I, Shapiro F, Kent R, Moses A (1986) A longitudinal study of the growth of the New Zealand white rabbit: cumulative and biweekly incremental growth rates for body length, body weight, femoral length, and tibial length. J Orthop Res 4(2):221–231
Luppen CA, Blake CA, Ammirati KM, Stevens ML, Seeherman HJ, Wozney JM, Bouxsein ML (2002) Recombinant human bone morphogenetic protein-2 enhances osteotomy healing in glucocorticoid-treated rabbits. J Bone Miner Res 17(2):301–310
Waters RV, Gamradt SC, Asnis P, Vickery BH, Avnur Z, Hill E, Bostrom M (2000) Systemic corticosteroids inhibit bone healing in a rabbit ulnar osteotomy model. Acta Orthop Scand 71(3):316–321
Little DG, Smith NC, Williams PR, Briody JN, Bilston LE, Smith EJ, Gardiner EM, Cowell CT (2003) Zoledronic acid prevents osteopenia and increases bone strength in a rabbit model of distraction osteogenesis. J Bone Miner Res 18:1300–1307
Coelho AL, Suzuki M, Dibart S, DA Silva N, Coelho PG (2007) Cross-sectional analysis of the implant-abutment interface. J Oral Rehabil 34(7):508–516
Schenk RK, Olah AJ, Herrmann W (1984) Preparation of calcified tissues for light microscopy. In: Dickson GR (ed) Methods of calcified tissue preparation. Elsevier Science, Amsterdam, pp 1–56
He FM, Yang GL, Li YN, Wang XX, Zhao SF (2009) Early bone response to sandblasted, dual acid-etched and H2O2/HCl treated titanium implants: an experimental study in the rabbit. Int J Oral Maxillofac Surg 38(6):677–681
Nociti FH Jr, Stefani CM, Sallum EA, Duarte PM, Sallum AW (2002) Nicotine and bone density around titanium implants: a histometric study in rabbits. Implant Dent 11(2):176–182
Gasser JA, Ingold P, Venturiere A, Shen V, Green JR (2008) Long-term protective effects of zoledronic acid on cancellous and cortical bone in the ovariectomized rat. J Bone Miner Res 23:544–551
Bijlsma JWJ, Van Everdingen A, Huisman M, De Nijs RNJTL, Jacobs JWG (2002) Glucocorticoids in rheumatoid arthritis. Ann NY Acad Sci 966:82–90
Di Munno O, Delle Sedie A (2008) Effects of glucocorticoid treatment on focal and systemic bone loss in rheumatoid arthritis. J Endocrinol Invest 31(7):43–47
Castañeda S, Calvo E, Largo R, González-González R, de la Piedra C, Díaz-Curiel M, Herrero-Beaumont G (2008) Characterization of a new experimental model of osteoporosis in rabbits. J Bone Miner Metab 26(1):53–59
Walsh LJ, Wong CA, Pringle M, Tattersfield AE (1996) Use of oral corticosteroids in the community and the prevention of secondary osteoporosis: a cross sectional study. BMJ 313(7053):344–346
Naganathan V, Jones G, Nash P, Nicholson G, Eisman J, Sambrook PN (2000) Vertebral fracture risk with long-term corticosteroid therapy: prevalence and relation to age, bone density, and corticosteroid use. Arch Intern Med 160(19):2917–2922
Michel BA, Bloch DA, Fries JF (1991) Predictors of fractures in early rheumatoid arthritis. J Rheumatol 18(6):804–808
Adinoff AD, Hollister JR (1983) Steroid-induced fractures and bone loss in patients with asthma. N Engl J Med 309(5):265–268
Van Staa TP, Laan RF, Barton IP, Cohen S, Reid DM, Cooper C (2003) Bone density threshold and other predictors of vertebral fracture in patients receiving oral glucocorticoid therapy. Arthritis Rheum 48:3224–3229
Kanis JA, Johansson H, Oden A, Johnell O, de Laet C, Melton LJ III, Tenenhouse A, Reeve J, Silman AJ, Pols HA, Eisman JA, McCloskey EV, Mellstrom D (2004) A meta-analysis of prior corticosteroid use and fracture risk. J Bone Miner Res 19(6):893–899
Peel NF, Moore DJ, Barrington NA, Bax DE, Eastell R (1995) Risk of vertebral fracture and relationship to bone mineral density in steroid treated rheumatoid arthritis. Ann Rheum Dis 54(10):801–806
Gao Y, Luo E, Hu J, Xue J, Zhu S, Li J (2009) Effect of combined local treatment with zoledronic acid and basic fibroblast growth factor on implant fixation in ovariectomized rats. Bone 44(2):225–232
Ogoshi T, Hagino H, Fukata S, Tanishima S, Okano T, Teshima R (2008) Influence ofglucocorticoid on bone in 3-, 6-, and 12-month-old rats as determined by bone mass and histomorphometry. Mod Rheumatol 18(6):552–561
Mori H, Manabe M, Kurachi Y, Naguno M (1997) Osseointegration of dental implants in rabbit bone with low mineral density. J Oral Maxillofac Surg 55:351–361
Mavrogenis AF, Dimitriou R, Parvizi J, Babis GCJ (2009) Biology of implant osseointegration. J Musculoskelet Neuronal Interact 9(2):61–71
Hirakawa K, Jacobs JJ, Urban R, Saito T (2004) Mechanisms of failure of total hip replacements: lessons learned from retrieval studies. Clin Orthop Relat Res 420:10–17
Lack DM, Delmas PD, Eastell R, Reid IR, Boonen S, Cauley JA, Cosman F, Lakatos P, Leung PC, Man Z, Mautalen C, Mesenbrink P, Hu H, Caminis J, Tong K, Rosario-Jansen T, Krasnow J, Hue TF, Sellmeyer D, Eriksen EF, Cummings SR (2007) HORIZON Pivotal Fracture Trial. Once-yearly zoledronic acid for treatment of postmenopausal osteoporosis. N Engl J Med 356(18):1809–1822
Reid DM, Devogelaer JP, Saag K, Roux C, Lau CS, Reginster JY, Papanastasiou P, Ferreira A, Hartl F, Fashola T, Mesenbrink P, Sambrook PN, HORIZON investigators (2009) Zoledronic acid and risedronate in the prevention and treatment of glucocorticoid-induced osteoporosis (HORIZON): a multicentre, double-blind, double-dummy, randomised controlled trial. Lancet 373(9671):1253–1263
Greiner SH, Wildemann B, Back DA, Alidoust M, Schwabe P, Haas NP, Schmidmaier G (2008) Local application of zoledronic acid incorporated in a poly(d, l-lactide)-coated implant accelerates fracture healing in rats. Acta Orthop 79(5):717–725
Greiner S, Kadow-Romacker A, Wildemann B, Schwabe P, Schmidmaier G (2007) Bisphosphonates incorporated in a poly(d, l-lactide) implant coating inhibit osteoclast like cells in vitro. J Biomed Mater Res A 83(4):1184–1191
Greiner S, Kadow-Romacker A, Lübberstedt M, Schmidmaier G, Wildemann B (2007) The effect of zoledronic acid incorporated in a poly(D, L-lactide) implant coating on osteoblasts in vitro. J Biomed Mater Res 80(4):769–775
Suratwala SJ, Cho SK, van Raalte JJ, Park SH, Seo SW, Chang SS, Gardner TR, Lee FY (2008) Enhancement of periprosthetic bone quality with topical hydroxyapatite-bisphosphonate composite. J Bone Joint Surg Am 90(10):2189–2196
You YN, Short KR, Jourdan M, Klaus KA, Walrand S, Nair KS (2009) The effect of high glucocorticoid administration and food restriction on rodentskeletal muscle mitochondrial function and protein metabolism. PLoS ONE 4(4):e5283
Kugelberg M, Shafiei K, Ohlsson C, Sävendahl L, Zetterström C (2005) Glucocorticoid eye drops inhibit growth in the newborn rabbit. Acta Paediatr 94(8):1096–1101
de Lorimier LP, Fan TM (2005) Bone metabolic effects of single-dose zoledronate in healthy dogs. J Vet Intern Med 19(6):924–927
Arden-Cordone M, Siris ES, Lyles KW, Knieriem A, Newton RA, Schaffer V, Zelenakas K (1997) Antiresorptive effect of a single infusion of microgram quantities of zoledronate in Paget’s disease of bone. Calcif Tissue Int 60(5):415–418
Acknowledgments
The authors are grateful to Maria Aurora Gomes da Silva and Maria de Fátima de Almeida for skillful technical assistance, and to Dr. Walcy R. Teodoro and Dr. Vanda Jorgetti for helpful discussion of the histological analyses. The study was supported in part by grants from Conexão Sistema de Prótese Ltda, FAPESP #06/57383-5 and Conselho Nacional de Ciência e Tecnologia (CNPQ) #305691/2006-6 (RMRP).
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Carvas, J.S.B., Pereira, R.M.R., Caparbo, V.F. et al. A single dose of zoledronic acid reverses the deleterious effects of glucocorticoids on titanium implant osseointegration. Osteoporos Int 21, 1723–1729 (2010). https://doi.org/10.1007/s00198-009-1125-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-009-1125-5