Abstract
Summary
To clarify the contribution of osteoporosis to future immobilization, a prospective observational study was carried out on Japanese postmenopausal women. The prevalence of low bone mineral density (BMD) and vertebral fracture were independent risks for future immobilization.
Introduction
Immobilization by hip fracture requires more medical care and higher costs. Osteoporosis increases the risk of hip fracture, but there is little data linking osteoporosis and immobilization in postmenopausal Japanese women.
Methods
The study participants consisted of postmenopausal ambulatory volunteers. Baseline information such as BMD, prevalent fractures, comorbidities, pain in the body, and variables were obtained from 1993, and time course of occurrence of immobilization was observed until 2008.
Results
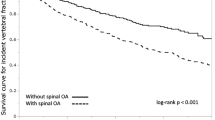
A total of 1,312 participants were enrolled and were observed for a total of 6.7 ± 4.1 years. A total of 75 subjects suffered immobilization. In multivariate analysis to calculate the Cox’s hazard ratio of baseline parameters for immobilization, four independent variables were observed: age (hazard ratio, 1.52 [95% CI, 1.29 to 1.80], p = 0.000), pain in the body (2.54 [1.42 to 4.89, p = 0.001]), low BMD (1.83 [1.10 to 3.13, p = 0.020]), and dementia (3.58 [91.80 to 6.76, p = 0.001]). The hazard ratio of prevalent vertebral fracture was 1.98 (1.20 to 3.30, p = 0.007) instead of low BMD of above model.
Conclusion
These results indicate that low BMD and prevalent vertebral fracture pose an independent risk for future immobilization in postmenopausal Japanese women.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Japan is known as a rapidly aging society. In fact, the total number of households with persons aged 65 or older shot up from 8.5 million in 1980 to 18.5 million in 2005. Due to significant changes in family composition in Japan after industrial success, approximately half of the 18.5 million households are maintained by elderly people who live alone or as elderly pair and potentially need care [1]. In addition, a total of approximately 60 billion dollars were required for the public health care system in 2007 [2], the cost of care for patients with fractures accounted for around 13% (8 billion dollars) [3], and the overall cost of treating fractures was the third highest expense [4]. With Japan’s first generation of baby boomers entering their 60s, a significant increase in the number of elderly households and drastically higher costs for their care are expected in the near future. Globally, the demand for medical care and social services for elderly people is increasing, while medical resources are apparently becoming scarcer, especially in Japan and the USA [5]. Seeking possible strategies and solutions to these issues, communities in each country should take prompt action by grasping and analyzing the current status of elderly patient care.
In conclusion, osteoporosis—a systemic skeletal disease characterized by deteriorated bone strength [6]—is considered a national issue in our aging society because it increases susceptibility to bone fractures, which impair quality of life (QOL) and decrease the mobility of affected patients [7, 8]. Special care is required by osteoporotic patients, especially those with hip fractures. In addition, it is reported that vertebral fractures are a risk factor increasing mortality in the Caucasian [9–12] and Asian populations [13]. However, there are no available data to show whether low bone mineral density (BMD), prevalent fractures, or incident vertebral fractures pose a risk of future immobility. For this reason, we have attempted to investigate the risk and frequency of immobilization in this prospective observational study among postmenopausal ambulatory Japanese women.
Methods
Subject selection and follow-up
This prospective observational study began April 1, 1993 in Nagano prefecture, Japan. Study participants were postmenopausal ambulatory volunteers over 50 years of age who were recruited from patients visiting Research Institute and Practice for Involutional Diseases and were selected by two practitioners (MS and YS). Exclusion criteria included critical illness and irregular clinical visits. Patients with metabolic bone diseases such as primary hyperparathyroidism, hyperthyroidism, osteomalacia, and malabsorption syndrome; steroid users; and those with severe renal failure were also excluded from the study. The period of follow-up for each participant was calculated as the time from inclusion in the study to the occurrence of immobilization, exit from study, or end of study (April 30, 2008). Whenever a participant did not show up, an attempt was made to contact the participant, by telephone or letter, and recommend a visit to the clinic. Participant immobility and survival were also confirmed through inquiries. When we lost contact with subjects who moved to relatives’ homes mainly due to loss of independence in their daily life, follow-up was terminated upon confirmation they had moved. Other missing cases were patients referred to other hospitals for various reasons. The follow-up periods for those cases were terminated upon the date of referral. Follow-up for participants who died during the observation was terminated when the date of death was confirmed by death certificate. Subjects bed-bound in their homes and receiving familial care or institutionalized in nursing homes were defined as immobile, and their follow-up was terminated on the date they were bed-bound or institutionalized.
Baseline data collection
As a baseline examination, anthropometrical indices such as body weight, body height, and body mass index (BMI, kg/m2) were measured. An interview was carried out to determine smoking and alcohol drinking habits. When subjects visited practitioners due to pain in the body during locomotion, the exact site of pain was identified as knee, leg, hip, or dorsal lesion. The effect of baseline pain in the body on immobilization was analyzed for different types of pain and general pain. Lumbar osteoarthrosis was diagnosed based on the Kellgren–Lawrence score (K–L score) [14], and rheumatoid arthritis was diagnosed based on criteria proposed by the American Rheumatism Association [15]. The other histories of comorbidities including diabetes mellitus, hypertension, dyslipidemia, dementia, malignancies, and cardio- and cerebro-vascular events were investigated. When subjects indicated some comorbidity, the diagnosis of that comorbidity was made by the proper diagnostic measures reported previously [13].
Measurements of bone mineral density and biochemical indices
Axial bone mineral density at lumbar spine (LBMD) was measured by dual-energy X-ray absorptiometry (DXA) using a Lunar DPX-L or DPX-IQ (Lunar Corporation, Madison, WI, USA). The inter-assay variance of LBMD in our laboratory was 0.5 ± 0.5% (CV ± SD) [16]. To detect machine drift, a quality assurance test was carried out with every measurement.
Non-fasting serum, plasma and urine samples were collected at the time of enrollment as baseline data. Biochemical examinations such as serum levels of calcium, phosphate, Al-P activity, total protein, total cholesterol, triglycerides, HbA1c, glucose, and creatinine were measured immediately after centrifugation using an auto-analyzer.
Diagnosis of osteoporosis and treatment
The diagnosis of osteoporosis was made in accordance with the diagnostic criteria for osteoporosis (year 2000 version) proposed by the Japanese Society for Bone and Mineral Research [17], in which osteoporosis is diagnosed as the presence of fragility fractures in any bone lesion in those with less BMD than 80% (−1.63SD) of the young adult mean (YAM). Osteoporosis is also diagnosed when the LBMD is less than 70% (−2.45SD) of the YAM even in those without prevalent fragility fractures. In those diagnosed as having osteoporosis, bone resorption inhibitors (bisphosphonate, estrogen, or selective estrogen receptor modulator), 1-alpha-OH vitamin D3, or vitamin K2 were administered if they desired such treatment. The specific treatment each subject received was selected according to subject preference and with our assistance. Some of these patients did not want to receive any osteoporotic drugs, for various reasons, and some patients exhibited very low compliance to the therapeutic regimen prescribed. Therefore, the subjects were categorized into three groups in accordance with treatment status: no treatment, bisphosphonate or estrogen, and vitamin groups.
Definition of prevalent and incident fracture
We investigated the presence of prevalent and incident fractures of vertebral and long bones (fractures of the hip, distal end of radius, surgical neck of humerus or other long bone). Vertebral fractures were diagnosed by a semi-quantitative visual method reported by Genant et al. [18] that was adapted to the present study in accordance with the method reported previously [19, 20]. The vertebral X-ray films were taken every 1 to 2 years interval, and the additional X-ray films were also taken when the participants complained the clinical symptoms suspicious for vertebral fractures. The presence of prevalent long bone fractures was determined through interviews with participants, on the basis of medical records, or by X-ray film confirmation.
Assessment of mobility
Mobility was defined in accordance with the subject’s locomotive ability. Subjects bed-bound at home (lying in bed all day) or institutionalized in nursing homes (lying in bed or using a wheelchair for locomotion), were defined as immobile. Subjects who moved to relatives’ homes, another type of dependency, were defined as missing cases because the reasons for moving were expected to be complicated, and immobility was not the only reason for moving.
Ethical considerations
The ethical committee of the Research Institute and Practice for Involutional Diseases reviewed the protocol of the present study. Detailed written informed consent was also obtained from all subjects.
Statistical analysis
In the descriptive analysis of baseline characteristics, the numerical data are expressed as mean ± SD. To clarify the relationship between subjects with or without immobility and baseline characteristics, the age-adjusted Cox’s proportional hazard model was used to estimate the association and time dependency between immobility and baseline data. Here, we estimated the age-adjusted hazard ratios with 95% confidence intervals as study variables. Second, in multivariate Cox’s regression analysis, we used the backward variable selection method. The exclusion criterion was a p value of less than 0.1. All p values presented were taken from the two-side test and considered significant when less than 0.05. All analyses were performed using JMP software, version 5.1.2 (SAS Institute Inc., Carly, NC, USA).
Results
Demography of the subjects
A total of 1,405 postmenopausal women met the inclusion criteria. Among them, 93 subjects refused to participate in the present study, and the remaining 1,312 subjects were enrolled in the study. The mean and SD of age was 65.1 ± 9.2 years old, and the follow-up period was 6.7 ± 4.1 years with the longest observation time being 15 years. The numerical and categorical data at baseline are listed in Tables 1 and 2, respectively. In contrast to data reported for the Caucasian population, subjects with smoking or alcohol habits were markedly fewer. Factors affecting locomotion ability included prevalent fractures (24.2% of subjects) and pain in the body at joints, legs, or dorsal lesion (63.1% of subjects). Categorized baseline data were summarized in Table 2. A total of 525 (40.0%) osteoporotic patients were treated with anti-resorptive drugs (bisphosphonates and selective estrogen receptor modulator or estrogen), and the remaining 787 (60.0%) participants were followed without drug intervention for osteoporosis.
Outcomes during observation
Follow-up for 746 of the 1,312 cases (56.9%) continued until the end of the study on April 30, 2008. The remaining 466 cases (35.5%) dropped out of the study. A total of 75 cases met the definition of immobilization in the present study (5.7%, 8.6 per 1,000 person-years). Twenty-five subjects moved from their own house to a relative’s house. Some lost a degree of independence but not enough to meet the definition of immobilization. Furthermore, the causes of moving were not simply due to disability but also economical reason or dementia.
Table 3 summarizes incident fractures observed during the observation period. The most frequent type of incident fracture was vertebral fractures, including both morphometrical and clinical fractures.
Table 4 presents the age-adjusted hazard ratio of baseline or incident parameter in the event of immobilization. As shown in Table 4, hazard ratios of age, pain in the body, fracture (prevalent), BMD, diabetes, and dementia indicate a p value of less than 0.1. In contrast to expectations, the odds ratio for immobilization of incident fracture did not reach a significant level.
Additionally, we also conducted variable selection for these significant factors. The presence of osteoporosis and prevalent fractures showed a very high correlation: the presence of fractures was 40.9% (235 cases out of 575) in subjects with osteoporosis and 4.6% (34 cases out of 737) in those without osteoporosis. In our two-model analysis, the type-1 model included the presence of osteoporosis, and the type-2 model included the presence of fractures. Table 5 shows the multivariate hazards ratio by Cox’s regression analysis of risks for immobility adjusted for age, presence of pain, osteoporosis, and dementia. Table 6 shows the multivariate hazards ratios of prevalent fractures, instead of presence of osteoporosis, in the type-1 model. Each factor posed a significant independent risk for immobility in postmenopausal Japanese women.
Discussion
The primary aim of the present study was to clarify whether osteoporosis poses a future risk for immobilization. The Cox’s hazard model demonstrated that osteoporosis and prevalent vertebral fractures are associated with immobilization after adjustment of confounding factors. Osteoporosis is a known disease that raises susceptibility to future fractures and hip or vertebral fractures resulting in decreased QOL [21–23] or disability after hip fractures [24–27]. In the present study, 451 incident fractures were observed during the observation period among 1,312 participants. Although prevalent fractures were a significant risk factor, incident fractures were not. These results suggested that fractures that occurred early and existed for a long time affected mobility more than the ones that occurred after entering the study. However, these results did not indicate less importance of incident fractures in terms of occurrence of immobilization. It may be simply due to lack of statistical power.
We have been focusing on the occurrence of immobilization in postmenopausal Japanese women but not on quality of life or activities of daily living (ADL) scores, which can estimate the subject’s status of activity quantitatively. The QOL or ADL score may not be enough to clearly understand the subject’s activity directly. On the other hand, the immobilization defined in the study may be recognized more easily in practice to assess the subject’s activity than the QOL or ADL score. This is why we evaluated the subject’s morbidity by housebound or institutionalized condition.
In the present study, we evaluated the effect of multiple factors potentially affecting locomotion or mobility, such as bone and joint diseases, vascular diseases, and dementia. In addition to locomotion-related diseases, comorbidities of common diseases in the elderly, such as hypertension, dyslipidemia, diabetes, and past history of malignancies were also evaluated in the participants. Those baseline evaluations may enable assessment of the effects of the total condition on immobility in the elderly. As shown in Table 6, pain in the body and dementia are independent risks for immobility, and these findings appear reasonable. We did not evaluate the causes of pain and the degree of pain because the causal factors for some kinds of pain could not be analyzed, and the assessment of degree of pain is thought to vary subjectively. Since most pain may be due to bone and joint degenerative diseases, such as osteoarthrosis in vertebrae or leg joints and osteoporosis, our findings were within expectations. While individual site of pain did not pose a significant risk of immobilization, overall pain in the body did pose a significant risk of immobilization. Three possible explanations may account for the findings. The first possible explanation is that the accumulation of pain from various sites may be a risk, and the second reason is that degree of pain is important but not the pain location. The third reason is that the number of sites of pain did not have a significant statistical power when the pain in the body was divided into each site of pain. Further clarification may be required. Since previous reports also indicated that subjects with dementia were prone to a significantly greater risk of decline in daily activities [28], the present result in terms of the relation between dementia and immobilization was good agreement. The other comobidities did not show any significant relation to immobilization. The patients with nervous diseases were also expected to have immobilization. However, the numbers of patient with nervous systems were very small, and the statistical power may not be enough.
The effect of osteoporotic treatment by bone resorption inhibitors on future immobilization was not significant in this study group. It has been reported that alendronate, calcitonin, and teriparatide treatments were known to decrease low back pain [29–31]. Furthermore, estrogen and bisphosphonate treatments were known modalities for preventing incident fractures. Thus, it is possible that the treatment of osteoporosis is a factor that reduces the likelihood of immobilization. However, the present results did not show a significant reduction in the risk of future immobilization in subjects who receive osteoporotic treatment. This is because osteoporotic treatment may reduce the risk of immobilization caused by osteoporotic fractures, but the causal factors for immobilization in the present study include not only osteoporosis but also osteoarthrosis and dementia. Therefore, the effect of osteoporotic treatment on immobilization should be evaluated in osteoporotic patients by drug comparative trial.
In conclusion, age, pain in the body, osteoporosis, and dementia are independent risk factors for future immobilization among Japanese postmenopausal women.
References
Iijima S (2008) Situation of the long-term care insurance system. Jpn J Geriatrics 45:377–380 In Japanese
Harada A, Matsui Y, Takemura M, Ito Z, Wakao N, Ota T (2005) Cost-utility analysis of osteoporosis. Jpn J Geriat 16:6–14 In Japanese
Cabinet Office, Government of Japan (2004) White Paper on the National Lifestyle 2004 A comfortable way of life for the Japanese people, founded on personal relationships
Okie S (2008) Home delivery—bringing primary care to housebound elderly. New Engl J Med 359:2409–2412
NIH Consensus Development Panel on Osteoporosis Prevention, Diagnosis, and Therapy (2001) Osteoporosis prevention, diagnosis, and therapy. JAMA 285:785–795
Hannan EL, Magaziner J, Wang JJ, Eastwood EA, Silberzweig SB, Gilbert M, Morrison RS, McLaughlin MA, Orosz GM, Siu AL (2001) Mortality and locomotion 6 months after hospitalization for hip fractures: risk factors and risk-adjusted hospital outcomes. JAMA 285:2736–2742
Siu AL, Penrod JD, Boockvar KS, Koval K, Strauss E, Morrison RS (2006) Early ambulation after hip fracture: effects on function and mortality. Arch Intern Med 166:766–771
Johnell O, Kanis JA, Oden A, Sernbo I, Redlund-Johnell I, Petterson C, De Laet C, Jonsson B (2004) Mortality after osteoporotic fractures. Osteoporos Int 15(1):38–42
Ensrud KE, Thompson DE, Cauley JA, Nevitt MC, Kado DM, Hochberg MC, Santora AC, Black DM (2000) Prevalent vertebral deformities predict mortality and hospitalization in older women with low bone mass. Fracture intervention trial research group. J Am Geriatr Soc 48(3):241–249
Center JR, Nguyen TV, Schneider D, Sambrook PN, Eisman JA (1999) Mortality after all major types of osteoporotic fracture in men and women: an observational study. Lancet 353(9156):878–882
Kado DM, Browner WS, Palermo L, Nevitt MC, Genant HK, Cummings SR (1999) Vertebral fractures and mortality in older women: a prospective study. Study of osteoporotic fractures research group. Arch Intern Med 159(11):1215–1220
Kuroda T, Shiraki M, Tanaka S, Ohta H (2009) Contributions of 25-hydroxyvitamin D, co-morbidities and bone mass to mortality in Japanese postmenopausal women. Bone 44:168–172
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16:494–502
Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS, Healey LA, Kaplan SR, Liang MH, Luthra HS et al (1988) The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum 31:315–324
Shiraki M, Shiraki Y, Aoki C, Hosoi T, Inoue S, Kaneki M, Ouchi Y (1997) Association of bone mineral density with apolipoprotein E phenotype. J Bone Miner Res 12:1438–1445
Orimo H, Hayashi Y, Fukunaga M, Sone T, Fujiwara S, Shiraki M, Kushida K, Miyamoto S, Soen S, Nishimura J, Ohashi Y, Hosoi T, Gorai I, Tanaka H, Igai T, Kishimoto H (2001) Osteoporosis Diagnostic Criteria Review Committee: Japanese Society for Bone and Mineral Research. Diagnostic criteria for primary osteoporosis: year 2000 revision. J Bone Miner Metab 19:331–337
Genant HK, Jergas M, Palermo L, Nevitt M, Valentin RS, Black D, Cummings SR (1996) Comparison of semiquantitative visual and quantitative morphometric assessment of prevalent and incident vertebral fractures in osteoporosis. The study of Osteoporotic Fractures Research Group. J Bone Miner Res 11:984–996
Shiraki M, Kuroda T, Nakamura T, Fukunaga M, Hosoi T, Orimo H, Makino K (2006) The sample size required for intervention studies on fracture prevention can be decreased by using a bone resorption marker in the inclusion criteria: prospective study of a subset of the Nagano Cohort, on behalf of the Adequate Treatment of Osteoporosis (A-TOP) Research Group. J Bone Miner Metab 24:219–225
Shiraki M, Kuroda T, Tanaka S, Saito M, Fukunaga M, Nakamura T (2008) Nonenzymatic collagen cross-links induced by glycoxidation (pentosidine) predicts vertebral fractures. J Bone Miner Metab 26:93–100
Hagino H, Nakamura T, Fujiwara S, Oeki M, Okano T, Teshima R (2009) Sequential change in quality of life for patients with incident clinical fractures: a prospective study. Osteoporosis Int 20(5):695–702
Cockerill W, Lunt M, Silman AJ, Cooper C, Lips P, Bhalla AK, Cannata JB, Eastell R, Felsenberg D, Gennari C, Johnell O, Kanis JA, Kiss C, Masaryk P, Naves M, Poor G, Raspe H, Reid DM, Reeve J, Stepan J, Todd C, Woolf AD, O’Neill TW (2004) Health-related quality of life and radiographic vertebral fracture. Osteoporos Int 15(2):113–119
Brenneman SK, Barrett-Connor E, Sajjan S, Markson LE, Siris ES (2006) Impact of recent fracture on health-related quality of life in postmenopausal women. J Bone Miner Res 21(6):809–816
Miller CW (1978) Survival and ambulation following hip fracture. J Bone Joint Surg Am 60(7):930–934
Borgquist L, Ceder L, Thorngren KG (1990) Function and social status 10 years after hip fracture. Prospective follow-up of 103 patients. Acta Orthop Scand 61(5):404–410
Keene GS, Parker MJ, Pryor GA (1993) Mortality and morbidity after hip fractures. BMJ 307(6914):1248–1250
Kitamura S, Hasegawa Y, Suzuki S, Sasaki R, Iwata H, Wingstrand H, Thorngren KG (1998) Functional outcome after hip fracture in Japan. Clin Orthop Relat Res 348:29–36
Cotter VT (2007) The burden of dementia. Am J Manag Care Suppl 8:S193–S197
Nevitt MC, Thompson DE, Black DM, Rubin SR, Ensrud K, Yates AJ, Cummings SR (2000) Effect of alendronate on limited-activity days and bed-disability days caused by back pain in postmenopausal women with existing vertebral fractures. Fracture Intervention Trial Research Group. Arch Intern Med 160(1):77–85
Knopp JA, Diner BM, Blitz M, Lyritis GP, Rowe BH (2005) Calcitonin for treating acute pain of osteoporotic vertebral compression fractures: a systematic review of randomized, controlled trials. Osteoporos Int 16(10):1281–1290
Nevitt MC, Chen P, Dore RK, Reginster JY, Kiel DP, Zanchetta JR, Glass EV, Krege JH (2006) Reduced risk of back pain following teriparatide treatment: a meta-analysis. Osteoporos Int 17(2):273–280
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shiraki, M., Kuroda, T., Shiraki, Y. et al. Effects of bone mineral density of the lumbar spine and prevalent vertebral fractures on the risk of immobility. Osteoporos Int 21, 1545–1551 (2010). https://doi.org/10.1007/s00198-009-1121-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-009-1121-9