Abstract
Summary
This study examined femur geometry underlying previously observed decline in BMD of the contralateral hip in older women the year following hip fracture compared to non-fractured controls. Compared to controls, these women experienced a greater decline in indices of bone structural strength, potentially increasing the risk of a second fracture.
Introduction
This study examined the femur geometry underlying previously observed decline in BMD of the contralateral hip in the year following hip fracture compared to non-fractured controls.
Methods
Geometry was derived from dual-energy X-ray absorptiometry scan images using hip structural analysis from women in the third cohort of the Baltimore Hip Studies and from women in the Study of Osteoporotic Fractures. Change in BMD, section modulus (SM), cross-sectional area (CSA), outer diameter, and buckling ratio (BR) at the narrow neck (NN), intertrochanteric (IT), and shaft (S) regions of the hip were compared.
Results
Wider bones and reduced CSA underlie the significantly lower BMD observed in women who fractured their hip resulting in more fragile bones expressed by a lower SM and higher BR. Compared to controls, these women experienced a significantly greater decline in CSA (−2.3% vs. −0.2%NN, −3.2% vs. −0.5%IT), SM (−2.1% vs. −0.2%NN, −3.9% vs. −0.6%IT), and BMD (−3.0% vs. −0.8%NN, −3.3% vs. −0.6%IT, −2.3% vs. −0.2%S) and a greater increase in BR (5.0% vs. 2.1%NN, 6.0% vs. 1.3%IT, 4.4% vs. 1.0%S) and shaft outer diameter (0.9% vs. 0.1%).
Conclusion
The contralateral femur continued to weaken during the year following fracture, potentially increasing the risk of a second fracture.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hip fracture is the most severe consequence of osteoporosis in terms of morbidity and associated mortality [1–6]. The majority of hip fracture research has focused on predicting fractures and on interventions that reduce their incidence. Only limited attention has been given to changes in bone after a hip fracture, particularly to indices of bone strength, despite the propensity these patients have to fracture their contralateral hip [7–11]. Understanding the natural course of change in the contralateral hip after an index hip fracture is relevant to design of interventions to optimize recovery and to minimize the risk of additional fractures.
A previous study of women participating in the third Baltimore Hip Study (BHS3) showed that in the year following fracture, women with recent hip fractures had a decline in bone mineral density (BMD) in the unfractured hip 11 times greater than age-matched women who had not fractured their hip [12]. These results suggest that the unfractured, proximal femur is weakening considerably in the year following fracture. Assuming mechanical similarity with the hip that has already fractured this is an alarming trend that may underlie the observation that a prevalent hip fracture is a major risk factor for new hip fractures. However, inferences drawn from BMD measurements by dual-energy X-ray absorptiometry (DXA) do not explain how the mechanical strength differs from normal and how it changes over time.
Strength under a particular load is a function of the geometry which determines the magnitudes of stresses within the bone as well as the tissue properties which limit the ability of the tissue to resist those stresses [13]. Current noninvasive methods cannot measure tissue properties, and the hip structural analysis (HSA) technique used in the present study is only a partial solution because the limited 2D geometric information in a DXA scan is insufficient for a complete 3D engineering simulation. Nevertheless, the method can provide geometric measures of strength in bending and in axial compression as well as an index of susceptibility to local buckling, at two femur locations where fractures commonly occur and a third purely cortical region where they are rare. The purpose of this analysis is to examine the femur geometry underlying the previously observed changes in hip BMD in the year following hip fracture from the BHS3 study. To provide a context, we compared hip geometry and its rates of change with an age-matched control group of older women without hip fractures from the Study of Osteoporotic Fractures (SOF).
Methods
Identification of hip fracture cases
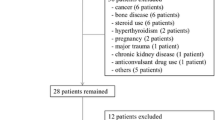
The Baltimore Hip Studies are a series of longitudinal studies of hip fracture outcomes in elderly community-dwelling men and women. The analysis for this paper used data collected from the third study; details have been previously published [14]. Briefly, between 1992 and 1995, 205 Caucasian women who were admitted to one of two acute care teaching hospitals in the Baltimore, Maryland metropolitan area after suffering a hip fracture were enrolled in the study. Women who were resident in nursing homes at the time of the fracture, admitted more than 48 h after the fracture event, under the age of 65, or had distal femoral fractures were excluded from participation.
Bone mineral density was measured at the non-fractured hip with dual-energy X-ray absorptiometry, using either Hologic QDR 1,000W® or QDR 1,500® (Hologic, Waltham, MA, USA) densitometers, within 18 days after fracture (baseline) and at 2, 6, and 12 months after the hip fracture admission. These scanners are both pencil beam systems and provide consistent measures of bone size. DXA machines were calibrated daily using a phantom to ensure that no significant drift occurred over time. Precision was calculated for each machine by measuring and remeasuring a group of healthy subjects who were taken on and off the scanner table. Precision was found to be 2.2% at the femoral neck and 4.0% at the trochanter using the conventional DXA software. Baseline scans were performed on 205 women; 124 were measured at 2 months, 121 at 6 months, and 102 at 12 months. A total of 176 women had at least one DXA scan suitable for hip structure analysis. All study protocols and consent procedures were approved by Institutional Review Boards of the participating hospitals and the University of Maryland Baltimore.
Identification of comparison groups
The comparison group was drawn from participants in the Study of Osteoporotic Fracture. The SOF is a multicenter prospective cohort study of Caucasian postmenopausal women with participants recruited from four areas in the USA: Baltimore Maryland, Minneapolis Minnesota, Portland Oregon, and the Monongahela Valley of Pennsylvania [15]. Women age 65 or older were enrolled between September 1986 and October 1988. At the second clinic visit, between January 1989 and December 1990, each participant had BMD measurements of the left hip using a Hologic QDR 1000 (Hologic, Waltham, MA, USA) DXA scanner and served as the “baseline” scan for this group. Scans were repeated at the fourth clinic visit using the same DXA scanner systems (August 1992 to July 1994), an average of 3.5 years later (range, 1.8 to 5.2 years). A total of 8,076 (83.2%) postmenopausal women participating in the study had DXA scans of the hip at study visit 2 (baseline), and of those, 5,079 had successful HSA analyses. At visit 4, 4,260 (84%) had a follow-up measurement by HSA.
For this analysis, an age-matched control group was randomly selected from a sample of 3,580 SOF women with HSA measures at both visits who had not suffered a hip fracture through the follow-up period in 2002. Two SOF participants were matched to each hip fracture case from BHS3 based on 5-year age groupings. Because SOF participants were younger, it was not possible to obtain matched controls for 25 BHS3 participants in the 86–90 and 90+ age groups, so these BHS3 subjects were excluded from the analysis.
Measures
Analysis of structural parameters
The HSA program employs conventional DXA image data to derive geometric properties of bone cross-sections using principles first described by Martin and Burr [16]. HSA conducted for this study used the software version developed at Johns Hopkins [17]. The HSA algorithm derives the conventional BMD, the outer diameter (OD), the total mineralized bone surface in the cross-section (CSA), the cross-sectional moment of inertia (CSMI), the locus of the center of mass (centroid), and the section modulus (SM) directly from the mass profiles [17]. The centroid position is reported as the distance of the centroid from the medial cortical margin divided by OD. Section modulus is computed as CSMI/d max, where d max is the maximum distance from the centroid to the medial or lateral cortical margin (Fig. 1). Another parameter, the buckling ratio (BR) is estimated as the ratio of d max to estimated mean cortical thickness derived from an annulus model of the cross-section using the measured OD, assuming that a fixed proportion of the CSA is in the cortex. The CSA and SM are indices of resistance to axial compressive and bending loads, respectively, while the BR is a crude index of susceptibility to local buckling under bending loads.
The HSA software generates profiles of pixel values traversing the proximal femur at three locations: the narrow neck (NN) across the femoral neck at its narrowest point, the intertrochanter (IT) along the angle bisector defined by the neck and shaft axes, and across the shaft at a distance of 1.5 times minimum neck width distal to the axes intersection. Although fracture only occurred in these subjects at the neck or IT region, shaft results where fragility fractures are rare are included to illustrate consistency in the outcomes, although buckling at the thick cortex shaft is unlikely even in these subjects. At each of these locations, five parallel profiles spaced one pixel apart both proximal and distal to the three defined locations, are generated. Within each region, the five profiles are averaged and the BMD, CSA, OD, SM, and BR are reported.
Covariates
Baseline age in years, height (cm), and weight (kg) were measured at 10 days or 2 months after fracture for BHS3 and at visit 2 (“baseline”) for SOF participants.
Statistical analysis
Differences in baseline age, height, weight, and femur geometry at three regions of the hip were compared using t tests. Baseline femur geometry adjusted for age, height, and weight was also compared because bone mechanical strength is positively correlated with age and body size. These results are presented as percent difference between BHS3 and SOF controls at all three regions. Differences in the follow-up periods for the BHS3 cohort (2, 6, and 12 months) and SOF cohorts (approximately 3.5 years between visits 2 and 4) prevent time-specific comparisons of bone geometry outcomes. Because measures were available at only two time points for the SOF subjects, rates of change were estimated assuming a linear rate of change over time. Comparisons of rates of change among the two cohorts were made using maximum likelihood estimates of the parameters of longitudinal regression models [12].
Mixed models were fitted for each outcome. Random subject effects were taken into account by specifying an exchangeable covariance matrix. The fixed effects for the comparison between the BHS3 and the SOF cohorts were modeled according to the following equation:
where Y t is the bone geometry measure of the subject at a specific follow-up time point; b 0 is the intercept (and represents the predicted level of the bone geometry measure for the SOF cohort at baseline); X is the cohort indicator variable where 0 = SOF and 1 = BHS3; t 2, t 6, t 12, and t >12 are indicator variables for the time points corresponding to follow-up at 2, 6, 12, and more than 12 months, respectively; and m is the months follow-up for subjects in the SOF cohort.
The baseline covariate terms include age, height, weight, and bone geometry measured at baseline. Because of the product terms involved, b 1, b 2, b 3, and b 4 are parameters fitted with BHS3 data and b 5, the linear rate of change parameter, with SOF data. Having obtained estimates of the parameters, the change from baseline at 12 months was determined as b 4 for the BHS3 cohort and b 5 for the SOF cohort.
Rates of change are reported as annual percent change, from age and body size—corrected bone geometry at baseline for each group at the narrow neck, IT, and shaft regions of the hip. Differences were considered significant if p < 0.05. All analyses were done using Stata statistical software, version 9 (Stata, College Station, TX, USA).
Results
Differences in baseline characteristics and bone geometry between SOF controls and BHS3 hip fracture cases are shown in Table 1, while adjusted percent differences from controls are displayed in Fig. 1. Baseline measurements were missing or technically unsuitable for HSA in 15 BHS3 women; therefore, these data were excluded from further analyses. Women who suffered from a recent hip fracture were significantly taller and weighed less than SOF controls. At the NN, IT, and shaft regions for both unadjusted and adjusted bone geometry, BHS3 women had significantly lower SM, BMD, CSA, and higher BR; OD was only significantly wider at the NN.
Annual percent changes for the two groups at the three femur regions are shown in Table 2, while modeled trends in these parameters are shown graphically in Figs. 2, 3, and 4. Bone mineral density: rates of decline in BMD were significantly higher in BHS3 women at the NN (3.0% vs. 0.8%, p < 0.01), IT (3.3% vs. 0.6%, p < 0.01), and shaft (2.3% vs. 0.2%, p < 0.01). Decline appears to be greatest during the first 6 months following fracture at the NN and IT (Figs. 2, 3, and 4). Cross-sectional area: rates of decline in CSA were significantly greater at the NN (2.3% vs. 0.2%, p < 0.01) and IT (3.2% vs. 0.5%, p < 0.01) and the greatest decline was observed at the NN and IT in the first 6 months following fracture (Figs. 2, 3, and 4). Outer diameter: the rate of OD expansion was similar at the NN and IT regions, but was significantly higher at the shaft (0.9% vs. 0.1%, p < 0.01). Section modulus: rates of decline in SM were significantly greater at the IT (3.9% vs. 0.6%, p < 0.01) but not at the NN or shaft. Similar to trends observed in BMD and CSA, decline was greatest during the first 6 months following fracture at the NN but during the first 2 months at the IT (Figs. 2, 3, and 4). Buckling ratio: buckling ratios increased faster in BHS3 women than in SOF controls at the NN (5.0% vs. 2.1%, p < 0.01), IT (6.0% vs. 1.3%, p < 0.01), and shaft (4.4% vs. 1.0%, p < 0.01) suggesting increasing susceptibility to local buckling (Figs. 2, 3, and 4).
Discussion
This analysis extends prior work by Magaziner and colleagues that showed significantly lower BMD of the contralateral hip and greater decline in the year following fracture in older women with hip fracture than in age-matched controls [12]. The continuing BMD decline is alarming because the unfractured hip was in all likelihood as fragile as the one that did fracture. The present study takes a closer look at that data by examining the underlying femur geometric strength and its trajectory of change to obtain a clearer perspective on the mechanical consequences of the BMD decline. As in the prior study, the results were compared to age-matched controls drawn from participants in the Study of Osteoporotic Fractures who had not suffered a prevalent or incident hip fracture.
In the cross-sectional comparison we observed a number of important geometric differences at post-fracture baseline between BHS3 fracture cases and SOF controls. Our goal was to gain some insight into how much structurally weaker the femurs of BHS3 women were compared to age-matched controls who do not fracture their hips. The adjusted BMD differences in BHS3 women averaged 9–14% lower at the three HSA regions than controls. The underlying mechanical implications of the BMD differences, however, are complicated by the opposing effects of OD on BMD and on bending strength (SM). In the definitive study of femur geometry in the SOF by Kaptoge et al., the ability of BMD to predict hip fracture could not be explained by mass differences alone (BMC or CSA) but required the additional decrement due to a wider bone diameter. Paradoxically, a wider bone should be stronger (higher SM) but femoral necks were significantly wider in BHS3 compared to SOF controls consistent with the findings of Kaptoge and colleagues in SOF and Rivadeneira and colleagues in the Rotterdam study [18, 19]. We did not observe wider femurs in BHS3 at the intertrochanter and shaft regions which may possibly reflect differences in fracture populations between these samples/studies. In neither the Kaptoge nor the Rivadeneira papers did section modulus predict fracture as well as BMD as would be expected from engineering beam theory, suggesting that the wider diameter may tend to preserve SM at the expense of cortical stability. In the present study the largest differences between BHS3 and SOF controls were in the buckling ratio, as was also evident in the SOF and Rotterdam studies [18, 19]. The rates of change in BR were greater than that of any other parameter in BHS3 compared to SOF controls suggesting that buckling susceptibility continues to increase (as is also evident in BMD decline) in the year following fracture.
In the longitudinal comparisons, the BHS3 women showed significant declines in SM (although not significant at NN and shaft), BMD, CSA, and significant increases in BR in the year following fracture. Outer diameter showed apparent increases at all regions but only reached significance in the 1-year period at the shaft where method precision is highest [20]. These results are consistent with adaptive changes to reduced loading activities in the post-fracture period among BHS3 women. In SOF controls, decline in BMD at the NN region was entirely due to change in OD; loss of NN bone (CSA) was non-significant. At the IT region, the decline in BMD was due to a combination of significant loss of CSA and a significant increase in OD. These opposing changes appear to preserve SM.
It is also important to note that there was little evidence of recovery among BHS3 women and the decline of some parameters appears to be greater in the first 6 months following fracture (Figs. 2, 3, and 4). Although there appears to be some recovery between 6 and 12 months, a full recovery is not achieved and the femur is geometrically weaker compared to baseline. This is consistent with findings from a study by Mikkola et al. that showed bone mineral mass and geometry of the tibia in women and men who sustained a hip fracture were systematically lower than non-hip fracture controls even an average of 3.5 years post-fracture [21]. These trends may be explained by the increase in bone turnover observed after fracture, perhaps secondary to a reduction in loading activity. Studies of biochemical markers of bone turnover showed that bone remodeling is significantly increased after fracture where resorption exceeds bone formation during the first 4–7 months following fracture, and though more consistent, bone markers continue to be elevated several years after fracture. These trends are most pronounced in hip fracture cases and may be further confounded by immobilization of the lower limb that typically follows this type of fracture [22–25]. The continued elevation of remodeling that occurs long after the fracture may lead to additional loss of bone mass and strength that predisposes women to a higher risk of future fracture. In contrast, a longitudinal study by Dirschl et al. reporting change in BMD over 6 years following fracture showed that BMD lost during the first year after fracture was completely recovered after 6 years, and was even higher than it was at the time of fracture [26]. However, results were from a small sample of men and women and it is not clear if these long-term trends would be similar in indices of bone strength.
Changes in femur geometry over time reflect adaptation to prevalent loading conditions, and the small changes among SOF controls suggest that their loading conditions remained relatively constant when no fracture occurs. This is clearly not the case in the recovery period following fracture, where loading is significantly diminished and when faster rates of change in CSA and SM following fracture are detected. Adaptation to load on the femur may be more evident in bone geometry than in BMD, which has important implications for rehabilitation strategies post-fracture [27, 28]. In addition, several pharmacologic intervention studies including treatment with PTH and Raloxifene have shown greater changes in bone geometry than in BMD [29, 30]. Primary outcomes for rehabilitation interventions post-fracture include improved functioning, but little is known about the effects of physical rehabilitation on BMD or bone strength. It may be that a combination of exercise and pharmacologic treatment will yield the most benefit.
Although the results of this study are consistent with the previous analyses of contralateral hip BMD among these women who have suffered a hip fracture, the annual BMD loss reported previously was up to two times greater than the BMD loss observed in this analysis [12, 31]. This may in part be due to differences in the analytic samples. However, differences in BMD loss between the two analyses are most likely due to the difference in methods used to measure BMD. BMD in the previous analysis was measured directly by conventional scanner software whereas in the present analysis, BMD was measured using HSA software. The HSA narrow neck region is roughly comparable to the conventional femoral neck; correlations between conventional DXA and HSA BMD measures are high although they are not equivalent due to difference in neck location and in algorithm edge detection. We ran the same models using DXA-measured BMD and found the results to be significant and comparable to BMD measured by HSA (DXA BMD, −3.2% in BHS3 vs. −0.6% in SOF; HSA BMD, −2.8% in BHS3 vs. −0.8% in SOF).
There were several limitations to this study. Although we were able to adjust for height, weight, and age at baseline, we were unable to account for additional factors that may influence change in bone strength following a hip fracture. It could be that femur weakening was exacerbated if women who suffered a hip fracture were sicker (had multiple co-morbidities) than their age-matched controls. However, in the previous analysis of BMD change the year after fracture, neither co-morbidities nor disability as measured by difficulty with ADLs were found to be confounders and were left out of final models. In addition, we were unable to accurately account for the influence of bone altering medication such as hormone replacement therapy (HRT), which was still a common therapy at the time women in these studies were scanned. HRT use was self-reported in the BHS3 and SOF studies and women in either study could only be categorized equivalently as ever taking HRT or not at all. We found that a significantly larger proportion of women who recently fractured their hip had ever taken HRT compared to SOF controls, but after adjustment, we found that results did not change. One cannot be certain that the contralateral hip was as fragile as the hip that fractured; moreover, changes in mechanical load due to altered stance on the intact hip during the recovery period may in part be responsible for some of the changes in geometry evident here. These complex effects cannot be evaluated with the limited data in this study. Finally, in order to make comparisons at 2, 6, and 12 months, we assumed a linear trajectory over 4 years for the SOF cohort as estimated from individual changes in the SOF subjects during that time span. Although one should be cautious when interpreting these results, the estimate decline in BMD over 12 months obtained in our study is similar to prior reports of BMD change over time [32–37]. While rates of change may vary with age, the average BMD decline observed in older women from a population-based cohort study adjusted for age and BMI was −0.0045 g/cm2 per year which is similar to the estimates we obtained for SOF controls in this analysis [33]. Other studies reported a decline in femoral BMD between 0.9% and 1.43% which is also similar to the estimates we obtained [32, 34–36]. However, if trajectories are not linear in this sample, our models may be over or underestimating the true difference between women with and without a hip fracture.
In conclusion, we have shown that geometric strength of the contralateral hip decreased significantly faster during the year following hip fracture compared to age-matched controls from the SOF study that did not experience a hip fracture. The majority of the geometric decline in BHS3 women occurs within the first 6 months at the NN and IT regions where fragility fractures occur. Given the increased risk of suffering a second fracture in the contralateral hip, this analysis provides a potential explanation of the mechanisms by which these fractures occur. Results of the present study point to further loss of bone strength as another consequence of hip fracture that should be considered when identifying strategies for post-fracture care.
References
Vestergaard P, Rejnmark L, Mosekilde L (2007) Has mortality after a hip fracture increased? J Am Geriatr Soc 55:1720–1726
Magaziner J, Lydick E, Hawkes W, Fox KM, Zimmerman SI, Epstein RS, Hebel JR (1997) Excess mortality attributable to hip fracture in white women aged 70 years and older. Am J Public Health 87:1630–1636
Penrod JD, Litke A, Hawkes WG, Magaziner J, Koval KJ, Doucette JT, Silberzweig SB, Siu AL (2007) Heterogeneity in hip fracture patients: age, functional status, and comorbidity. J Am Geriatr Soc 55:407–413
Fredman L, Magaziner J, Hawkes W, Hebel JR, Fried LP, Kasper J, Guralnik J (2005) Female hip fracture patients had poorer performance-based functioning than community-dwelling peers over 2-year follow-up period. J Clin Epidemiol 58:1289–1298
Magaziner J, Fredman L, Hawkes W, Hebel JR, Zimmerman S, Orwig DL, Wehren L (2003) Changes in functional status attributable to hip fracture: a comparison of hip fracture patients to community-dwelling aged. Am J Epidemiol 157:1023–1031
Magaziner J, Hawkes W, Hebel JR, Zimmerman SI, Fox KM, Dolan M, Felsenthal G, Kenzora J (2000) Recovery from hip fracture in eight areas of function. J Gerontol A Biol Sci Med Sci 55:M498–M507
Chapurlat RD, Bauer DC, Nevitt M, Stone K, Cummings SR (2003) Incidence and risk factors for a second hip fracture in elderly women. The study of osteoporotic fractures. Osteoporos Int 14:130–136
Melton LJ 3rd, Kearns AE, Atkinson EJ, Bolander ME, Achenbach SJ, Huddleston JM, Therneau TM, Leibson CL (2008) Secular trends in hip fracture incidence and recurrence. Osteoporos Int . doi:10.1007/s00198-008-0742-8
Nymark T, Lauritsen JM, Ovesen O, Rock ND, Jeune B (2006) Short time-frame from first to second hip fracture in the Funen County Hip Fracture Study. Osteoporos Int 17:1353–1357. doi:10.1007/s00198-006-0125-y
Berry SD, Samelson EJ, Hannan MT, McLean RR, Lu M, Cupples LA, Shaffer ML, Beiser AL, Kelly-Hayes M, Kiel DP (2007) Second hip fracture in older men and women: the Framingham Study. Arch Intern Med 167:1971–1976
Lonnroos E, Kautiainen H, Karppi P, Hartikainen S, Kiviranta I, Sulkava R (2007) Incidence of second hip fractures. A population-based study. Osteoporos Int 18:1279–1285. doi:10.1007/s00198-007-0375-3
Magaziner J, Wehren L, Hawkes WG, Orwig D, Hebel JR, Fredman L, Stone K, Zimmerman S, Hochberg MC (2006) Women with hip fracture have a greater rate of decline in bone mineral density than expected: another significant consequence of a common geriatric problem. Osteoporos Int 17:971–977
Hayes W, Bouxsein M (1997) Biomechanics of cortical and trabecular bone: implications for assessment of fracture risk. In: Mow V, Hayes W (eds) Basic orthopaedic biomechanics. Lippincott-Raven, Philadelphia, pp 66–111
Fox KM, Magaziner J, Hawkes WG, Yu-Yahiro J, Hebel JR, Zimmerman SI, Holder L, Michael R (2000) Loss of bone density and lean body mass after hip fracture. Osteoporos Int 11:31–35
Cummings SR, Black DM, Nevitt MC, Browner WS, Cauley JA, Genant HK, Mascioli SR, Scott JC, Seeley DG, Steiger P (1990) Appendicular bone density and age predict hip fracture in women. The Study of Osteoporotic Fractures Research Group. JAMA 263:665–668
Martin RB, Burr DB (1984) Non-invasive measurement of long bone cross-sectional moment of inertia by photon absorptiometry. J Biomech 17:195–201
Beck TJ (2007) Extending DXA beyond bone mineral density: understanding hip structure analysis. Curr Osteoporos Rep 2:49–55
Kaptoge S, Beck TJ, Reeve J, Stone KL, Hillier TA, Cauley JA, Cummings SR (2008) Prediction of incident hip fracture risk by femur geometry variables measured by hip structural analysis in the study of osteoporotic fractures. J Bone Miner Res . doi:10.1359/jbmr.080802
Rivadeneira F, Zillikens MC, De Laet CE, Hofman A, Uitterlinden AG, Beck TJ, Pols HA (2007) Femoral neck BMD is a strong predictor of hip fracture susceptibility in elderly men and women because it detects cortical bone instability: the Rotterdam Study. J Bone Miner Res 22:1781–1790
Khoo BC, Beck TJ, Qiao QH, Parakh P, Semanick L, Prince RL, Singer KP, Price RI (2005) In vivo short-term precision of hip structure analysis variables in comparison with bone mineral density using paired dual-energy X-ray absorptiometry scans from multi-center clinical trials. Bone 37:112–121
Mikkola T, Sipila S, Portegijs E, Kallinen M, Alen M, Kiviranta I, Pekkonen M, Heinonen A (2007) Impaired geometric properties of tibia in older women with hip fracture history. Osteoporos Int 18:1083–1090
Akesson K, Kakonen SM, Josefsson PO, Karlsson MK, Obrant KJ, Pettersson K (2005) Fracture-induced changes in bone turnover: a potential confounder in the use of biochemical markers in osteoporosis. J Bone Miner Metab 23:30–35
Obrant KJ, Ivaska KK, Gerdhem P, Alatalo SL, Pettersson K, Vaananen HK (2005) Biochemical markers of bone turnover are influenced by recently sustained fracture. Bone 36:786–792
Ivaska KK, Gerdhem P, Akesson K, Garnero P, Obrant KJ (2007) Effect of fracture on bone turnover markers: a longitudinal study comparing marker levels before and after injury in 113 elderly women. J Bone Miner Res 22:1155–1164
Yu-Yahiro JA, Michael RH, Dubin NH, Fox KM, Sachs M, Hawkes WG, Hebel JR, Zimmerman SI, Shapiro J, Magaziner J (2001) Serum and urine markers of bone metabolism during the year after hip fracture. J Am Geriatr Soc 49:877–883
Dirschl DR, Henderson RC, Oakley WC (1997) Accelerated bone mineral loss following a hip fracture: a prospective longitudinal study. Bone 21:79–82
Kaptoge S, Dalzell N, Jakes RW, Wareham N, Day NE, Khaw KT, Beck TJ, Loveridge N, Reeve J (2003) Hip section modulus, a measure of bending resistance, is more strongly related to reported physical activity than BMD. Osteoporos Int 14:941–949
Kaptoge S, Jakes RW, Dalzell N, Wareham N, Khaw KT, Loveridge N, Beck TJ, Reeve J (2007) Effects of physical activity on evolution of proximal femur structure in a younger elderly population. Bone 40:506–515
Uusi-Rasi K, Semanick LM, Zanchetta JR, Bogado CE, Eriksen EF, Sato M, Beck TJ (2005) Effects of teriparatide [rhPTH (1–34)] treatment on structural geometry of the proximal femur in elderly osteoporotic women. Bone 36:948–958
Uusi-Rasi K, Beck TJ, Semanick LM, Daphtary MM, Crans GG, Desaiah D, Harper KD (2006) Structural effects of raloxifene on the proximal femur: results from the multiple outcomes of raloxifene evaluation trial. Osteoporos Int 17:575–586
Wehren LE, Hawkes WG, Hebel JR, Orwig DL, Magaziner J (2005) Bone mineral density, soft tissue body composition, strength, and functioning after hip fracture. J Gerontol A Biol Sci Med Sci 60:80–84
Jones G, Nguyen T, Sambrook P, Kelly PJ, Eisman JA (1994) Progressive loss of bone in the femoral neck in elderly people: longitudinal findings from the Dubbo osteoporosis epidemiology study. BMJ 309:691–695
Burger H, de Laet CE, van Daele PL, Weel AE, Witteman JC, Hofman A, Pols HA (1998) Risk factors for increased bone loss in an elderly population: the Rotterdam Study. Am J Epidemiol 147:871–879
Dennison E, Eastell R, Fall CH, Kellingray S, Wood PJ, Cooper C (1999) Determinants of bone loss in elderly men and women: a prospective population-based study. Osteoporos Int 10:384–391
Melton LJ 3rd, Atkinson EJ, O’Connor MK, O’Fallon WM, Riggs BL (2000) Determinants of bone loss from the femoral neck in women of different ages. J Bone Miner Res 15:24–31
Ensrud KE, Palermo L, Black DM, Cauley J, Jergas M, Orwoll ES, Nevitt MC, Fox KM, Cummings SR (1995) Hip and calcaneal bone loss increase with advancing age: longitudinal results from the study of osteoporotic fractures. J Bone Miner Res 10:1778–1787
Karlsson M, Nilsson JA, Sernbo I, Redlund-Johnell I, Johnell O, Obrant KJ (1996) Changes of bone mineral mass and soft tissue composition after hip fracture. Bone 18:19–22
Conflicts of interest
The lead author has no conflicts of interest to report.
The following co-authors report disclosures for:
Consultancies: J. Magaziner—Merck, Novartis, Amgen; M.C. Hochberg—Amgen, Merck, Novartis, Roche Pharmaceutical Co., Wyeth Pharmaceuticals, and Eli Lilly Inc. In neither case do the consultancies relate to the research presented in this paper.
Licensing arrangement: T.J. Beck—the HSA method has been licensed to Hologic Inc. by the Johns Hopkins University, employer of T.J. Beck.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Funding Sources
The Study of Osteoporotic Fractures (SOF) is supported by National Institutes of Health funding. The National Institute on Aging (NIA) provides support under the following grant numbers: AG05407, AR35582, AG05394, AR35584, AR35583, R01 AG005407, R01 AG027576-22, 2 R01 AG005394-22A1, and 2 R01 AG027574-22A1, AG05407, AR35582, AG05394, AR35584, AR35583, AG026720.
The Baltimore Hip Studies are supported by NIH grant numbers: R37 AG009901; R01 AG018668; P30 AG028747.
Rights and permissions
About this article
Cite this article
Reider, L., Beck, T.J., Hochberg, M.C. et al. Women with hip fracture experience greater loss of geometric strength in the contralateral hip during the year following fracture than age-matched controls. Osteoporos Int 21, 741–750 (2010). https://doi.org/10.1007/s00198-009-1000-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-009-1000-4