Abstract
Summary
Previous studies have found an association between acid suppressants and fracture risk. We assessed fracture risk in patients taking concomitant acid suppressant and bisphosphonates. Positive associations were observed for any hip and vertebral fracture. The effect size was modest; however, the significance lies in the widespread prescribing of acid suppressants.
Introduction
Previous studies have found that acid-suppressive medication (ASM) is associated with an increased risk of fracture. Bisphosphonates can cause upper gastrointestinal problems, and patients may be prescribed ASM to minimise these effects.
Methods
A retrospective cohort study using the GPRD was conducted in patients aged 40 years and older starting proton pump inhibitors (PPI, N = 234,144), H2 receptor antagonists (H2RA, N = 166,798) or bisphosphonates (N = 67,309). Fracture risk in current versus past use of ASM and concomitant use of bisphosphonate plus ASM versus bisphosphonate alone was compared using time-dependent Cox regression.
Results
In the 6 months before initiating bisphosphonate therapy, 20.1% of patients received a PPI and 7.5% an H2RA. Current PPI use was associated with an increased risk of any (adjusted relative rate (ARR) 1.15, 95% CI 1.10–1.20), hip (ARR 1.22, 95% CI 1.10–1.37), and vertebral fracture (ARR 1.40, 95% CI 1.11–1.78); and concomitant bisphosphonates and PPIs with an increased risk of any (ARR 1.08, 95% CI 1.01–1.16) and hip fracture (ARR 1.24, 95% CI 1.08–1.42).
Conclusions
ASM is associated with an increased risk of fracture when taken alone or in combination with bisphosphonates. Given the frequency of coprescription of ASM and bisphosphonates, this issue requires further investigation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The lifetime risk of experiencing an osteoporotic fracture is approximately 40–50% in women and 13–22% in men [1]. The most serious of these, hip fracture, is associated with significant morbidity and mortality. It has been estimated that 20–30% of patients die in the first year after a hip fracture [2–4] and many others do not regain their independence [5, 6].
The majority of patients treated for osteoporosis are prescribed bisphosphonates. Whilst these drugs are efficacious and generally considered to have good safety profiles, they are associated with upper gastrointestinal problems, such as dyspepsia, acid regurgitation and oesophageal reactions. In prescription event-monitoring studies of alendronate and risedronate, dyspeptic symptoms were the most commonly reported side effect, with the incidence being four to five times seen in comparable patients in previous studies [7, 8]. Additional drugs may be prescribed in order to control emergent side effects. Roughead et al. [9] found that compared to controls, patients newly initiated onto bisphosphonate therapy were three times more likely to see their general practitioner (GP) within 6 weeks because of indigestion/dyspepsia and were consequently prescribed acid-suppressant medications. Three quarters of these returning patients were prescribed a proton pump inhibitor (PPI).
Recent studies have found an association between acid-suppressive medication and an increased risk of fracture. Yang et al. [10] conducted a nested case control study using the UK General Practice Research Database (GPRD) and found that chronic acid-suppressive medication was associated with an increased risk of hip fracture in patients aged 50 years and older. The effect was evident for both PPIs and H2RAs but was most pronounced with the former, where the risk of hip fracture increased with both higher doses of PPI and with longer durations of treatment. In a case-control study using Danish medical records, Vestergaard et al. [11] found that recent use of PPIs was associated with an increased risk of any hip and vertebral fracture; however, recent H2RA use was associated with a decreased risk of hip fracture. In the Study of Osteoporotic Fractures, the use of acid-suppressive medication was associated with an increased risk of nonspine fracture, but there were no effects on bone mineral density [12].
The main objective of this study was to further explore the risk of fracture in patients receiving acid-suppressive medication and to investigate whether concomitant prescription might attenuate the antifracture efficacy of bisphosphonates. The secondary objective was to describe the utilisation of acid-suppressant medication in bisphosphonate users.
Methods
Data source
The data for this study were obtained from the GPRD, which contains the computerised medical records of general practitioners in the UK. The current study included 418 practices. The data recorded in the GPRD include demographic information, prescription details, clinical events, specialist referrals and hospital admissions and their major outcomes. Clinical data are recorded and retrieved historically by means of Oxford Medical Information Systems codes and more recently by the Read code system. The GPRD is owned by the UK’s Department of Health.
Study population and outcome assessment
A retrospective cohort study was conducted in permanently registered male and female patients, who started either acid-suppressive medication (proton pump inhibitors or H2 receptor antagonists) or bisphosphonate therapy between 1st January 1988 and 2nd February 2007. The first prescription (i.e. the index date) occurred within the patients’ period of valid data collection, and there must have been 12 months of active follow-up prior to this. All individuals were followed up from the moment they have 1 year of valid history until the first prescription of acid-suppresive medication or bisphosphonates. Only patients aged 40 years or older at the date of first prescription were included. Patients with a history of Paget’s disease or cancer were excluded. The three resulting cohorts were mutually exclusive.
The period of follow-up was defined from the first bisphosphonate or acid-suppressive medication prescription up to latest GPRD data collection, patient’s transfer out of the practice or patient’s death, whichever date came first. The exposure variables were the use of bisphosphonates (alendronate, risedronate, ibandronate or etidronate) and acid-suppressive medication (PPIs or H2RAs). For the acid-suppressive medication, dosages were expressed as World Health Organisation defined daily doses (DDD). One DDD is equivalent to 20 mg omeprazole, 40 mg pantoprazole, 30 mg lansoprazole, 20 mg rabeprazole or 30 mg esomeprazole (PPIs), and to 800 mg cimetidine, 300 mg ranitidine, 40 mg famotidine or 300 mg nizatidine (H2RAs).
The period of follow-up was divided into periods of current and past exposure for bisphosphonate and for acid-suppressive medication. The period of current exposure was defined as the period from the date of prescribing up to 91 days after the estimated end of the prescription. Patients could move between exposure categories over the duration of follow-up. At the start of each period, prescribed daily dose of the current prescription and the cumulative duration of previous exposure to ASM were determined. In order to determine whether concomitant use of bisphosphonates and acid suppressants (i.e. prescriptions within 6 months before start of 3 months bisphosphonate episodes) attenuated fracture risk, we compared with users of bisphosphonates alone (i.e. patients who had never used acid suppressants or who had stopped taking acid suppressants for at least 6 months).
The outcome of interest was the first fracture after the index date. The classification of fractures was based on ICD ninth revision categories. The following types of fractures were examined: all fractures (ICD9 800–829.99), osteoporotic fractures (hip/femur (ICD9 820/821), vertebral (ICD9 805), radius/ulna (ICD9 813) and proximal humerus (ICD9 812)) and individual fractures including those of the hip/femur, vertebrae and radius/ulna. Previous studies have shown the GPRD to have high levels of completeness and validity with respect to fractures [13].
Covariates
Factors associated with fractures and considered as potential confounding variables included diabetes mellitus, rheumatoid arthritis, inflammatory bowel disease, congestive heart failure, cerebrovascular accident, chronic obstructive pulmonary disease, hysterectomy/early menopause, hormone replacement therapy, thiazide diuretics, anxiolytics, hypnotics, antidepressants, anti-Parkinson drugs, anticonvulsants, systemic corticosteroids, inhaled corticosteroids, bronchodilators, aluminium- and magnesium-containing antacids and calcium or vitamin D supplements. Smoking status (history, no history or unknown), body mass index (BMI) and a history of any fracture were also included [14]. All covariates were assessed prior to the index date; prescriptions in the 6 months before the index date and medical conditions at any point in the available history, except for age and the number of previous non-steroidal anti-inflammatory drug (NSAID) prescriptions, which were calculated in the one year before each acid suppressant prescription (none, 1–4, >4).
Statistical analysis
Adjusted relative rates (ARR) and 95% confidence intervals (95% CI) were estimated using time-dependent Cox regression. In non-users of bisphosphonates, the risk of fracture in current users of acid-suppressive medication was compared to the risk of fracture in past users. In the bisphosphonate cohort, fracture risk in users of bisphosphonates plus acid suppressants was compared to users of bisphosphonates only. The analyses were stratified by class (PPI or H2RA), daily dose and duration of use of acid suppressive medication. The Cox regression analyses included age and gender and the covariates. Differences between dose categories were tested using the Wald statistic.
Time to initiation of acid suppressive medication in bisphosphonate users was investigated using Kaplan–Meier life-table analysis. This analysis was stratified by age and gender. For patients who started a PPI or H2RA on the same day or after bisphosphonate therapy commenced, Kaplan–Meier life-table analysis was also used to investigate their persistence with acid-suppressive medication.
Sensitivity analysis
Treatment adherence with bisphosphonates may be reduced among patients taking concomitant ASM. In a sensitivity analysis, we estimated a medication possession ratio (MPR) at the start of each new bisphosphonate prescription. The MPR was equal to the total number of days of prior bisphosphonate exposure, divided by the time since the start of follow-up. We considered patients with MPRs between 0.7 and 1.0 as compliant and patients with MPRs <0.7 as non-compliant. Non-compliance was included as a confounder in the statistical models and as a multiplicative interaction variable composed of non-compliance and concomitant use of bisphosphonates and acid suppressants. In a second sensitivity analysis, we added an interaction variable between past use of bisphosphonates and past use of ASM.
Results
The acid suppressant population comprised 234,144 in the PPI cohort and 166,798 patients in the H2RA cohort, with 21,240 patients contributing to both groups. In the PPI group, the mean duration of follow-up was 3.5 years, during which the cohort received 2,802,266 PPI prescriptions: 45% omeprazole, 40% lansoprazole, 8% rabeprazole, 4% pantoprazole and 4% esomeprazole. Duration of follow-up in the H2RA group was 6.3 years. A total of 1,348,696 H2RA prescriptions were received: 62% ranitidine, 27% cimetidine, 10% famotidine and 1% nizatidine.
In the bisphosphonate cohort, 67,309 patients received one or more bisphosphonate prescriptions, and they were followed up for a mean of 3.3 years. These patients received a total of 1,144,682 prescriptions: 62% alendronate (53% weekly, 9% daily dosage packs), 22% risedronate (17% weekly, 5% daily dosage packs), 16% etidronate and 1% ibandronate.
Table 1 summarises the baseline characteristics of the acid suppression and bisphosphonate groups. The PPI and H2RA groups were similar in terms of age and gender split, with a mean age of 62 years and 61 years, respectively, and with just over half of patients being female. The most frequently recorded medical condition was early menopause/hysterectomy, followed by anaemia and diabetes, whilst NSAIDs were the most common medication, with almost a quarter of patients receiving at least one prescription in the 6 months prior to their index date. The mean age in the BP cohort was 72 years, and over 80% of the patients were female. The most common medical conditions were again early menopause/hysterectomy and anaemia followed by COPD. The most frequently prescribed medications in the 6 months before the index date were systemic corticosteroids and NSAIDs. In terms of previous acid-suppression medication use, 20.1% of patients had received a prescription for a PPI and 7.5% a prescription for a H2RA, in the 6 months before initiating bisphosphonate treatment.
Table 2 shows the fracture risk associated with current use of acid-suppressant medication compared to past use, both overall and stratified by dose, in patients who did not receive bisphosphonate treatment during follow-up. The risk of any fracture was significantly increased with current PPI use (ARR 1.15; 95% CI, 1.10–1.20) compared to past use but not for current H2RA use (ARR 1.03; 95% CI, 0.98–1.08). When the risk of any fracture with current PPI use was stratified by dose, there was some evidence of increasing fracture risk with increasing daily dose. Examination of fracture risk by site also showed an increased risk of fracture with current PPI use for the osteoporotic grouping and for hip and vertebral fractures. The risk of hip fracture increased by 22% (ARR 1.22, 95% CI, 1.10–1.37) and again there was evidence of a dose-dependent effect, with the increase in risk rising from 27% with medium dose PPI (ARR 1.27, 95% CI, 1.12–1.45) to 45% with higher doses (ARR 1.45, 95% CI, 1.06–1.99). The dose-dependent trends were less clear when the risks of osteoporotic and vertebral fractures were stratified by daily dose. Whilst not associated with an increase in all fractures, concomitant use of H2RAs was associated with an increase in osteoporotic and hip fractures, although no clear dose effect was observed. No association between acid-suppressant use and radius/ulna fractures was observed.
Stratifying the data by cumulative duration of use (Table 3), the risk of any fracture with current use of PPI was greatest in the first (ARR 1.18; 95% CI 1.10–1.27) and second years of use (ARR 1.17; 95% CI 1.08–1.27) but reduced with prolonged use (>3 years, ARR 1.11; 95% CI 1.03–1.20). A similar pattern was seen for vertebral fractures, with an increased risk of fracture observed in the first (ARR 1.83; 95% CI 1.25–2.68) and second year (ARR 1.63; 95% CI 1.08–2.45), before decreasing after >3 years of use (ARR 1.24; 95% CI 0.72–2.13). Hip fracture risk was also increased in the first (ARR 1.31; 95% CI 1.09–1.58) and second year (ARR 1.34; 95% CI 1.10–1.63), before it fell after >3 years of use, (ARR 1.17; 95% CI 0.98–1.41). In a sensitivity analysis, we compared current PPI users with distant past users (i.e. patients who had stopped taking PPIs for 3 years or longer, yielding a similar attenuation of fracture risk with prolonged PPI use). ARR of hip fracture were 1.39; 95% CI 1.07–1.82 for exposure <1 year, 1.32; 95% CI 0.99–1.76 for exposure 1–2 years, 1.15 95% CI 0.84–1.57 for exposure 2–3 years and 1.19; 95% CI 0.96–1.49 for use >3 years.
Table 4 shows the fracture risk associated with concomitant bisphosphonate and acid suppressant compared to current use of bisphosphonate use alone. For concomitant use of H2RAs, there was a significant association between current use and risk of vertebral fracture (ARR 1.56; 95% CI 1.24–1.96), which also showed evidence of a dose-dependent effect, although the number of cases was very small when considered by individual fracture site. There were no significant associations at the other fracture sites. Concomitant use of PPIs was associated with an increased risk of any fracture (ARR 1.08; 95% CI, 1.01–1.16) and hip fracture (ARR 1.24, 95% CI, 1.08–1.42). When these data were stratified by daily dose, there was some evidence of a dose-dependent trend. There was no significant association between concomitant use of bisphosphonate and PPI compared to bisphosphonate use alone and risk of osteoporotic fracture, radius/ulna fracture or vertebral fracture.
In a sensitivity analysis, we adjusted for non-compliance, using the MPR, and tested for a statistical interaction, but this did not alter the results (ARR 1.08; 95% CI 1.01–1.15 for any fracture and ARR 1.20, 95% CI 1.04–1.38 for hip fracture). In a second sensitivity analysis, we added a variable indicating previous use of acid suppressants and a multiplicative interaction variable between past bisphosphonate use and past acid suppressant use to the statistical model used for the analyses in Table 4. The risk of fracture remained unchanged when comparing concomitant current use of PPIs and bisphosphonates to current use of bisphosphonates alone (ARR 1.19; 95% CI 1.03–1.38 for hip fracture and ARR 1.09; 95% CI 1.02–1.17 for any fracture), and when comparing concomitant current use of H2RAs and bisphosphonates to current use of bisphosphonates alone (ARR 1.03; 95% CI 0.81–1.30 for hip fracture and ARR 1.09; 95% CI 0.97–1.22 for any fracture).
When PPIs were taken concomitantly with bisphosphonates, increased risk of fracture was observed at the hip after the first year (ARR 1.40; 95% CI 1.15–1.71), after which the effect attenuated (Table 5). For H2RAs, a similar pattern was observed for risk of vertebral fracture, with statistically significantly increased risk being observed in the first year only (ARR 1.97, 95% CI 1.32–2.95).
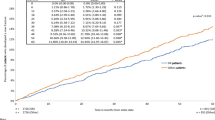
The time to initiation of acid-suppressive medication in patients starting bisphosphonate therapy is shown in Fig. 1. Overall, 8.5% of patients were prescribed a PPI and 2.7% H2RA on the same day they were initiated onto a bisphosphonate. In patients with no history of acid-suppression use, the figures were 2.9% and 0.7%, respectively. Within 3 months of continuous bisphosphonate use, 23.9% of patients had received a PPI and 9.6% H2RA, with these figures rising to 31.0% and 13.7% by 12 months, respectively. In patients with no history of acid-suppressive medication prior to initiation of bisphosphonates, the figures at 3 months were 5.4% and 1.5% and at 12 months, 10.8% and 3.8%, for PPI and H2RAs, respectively.
Life-table analysis of the time to the first acid suppressant prescription after start of bisphosphonate treatment among continuous users of bisphosphonates (with treatment gaps that did not exceed 3 months). Patients could have been exposed to acid suppressants before the first bisphosphonate prescription
Figure 2 shows the persistence with acid-suppressive medication in patients taking bisphosphonates. Persistence with both PPIs and H2RAs was approximately 99% in the first 3 months after initiation of bisphosphonates. Persistence dropped off after 3 months; however, almost a third of PPI users and a quarter of H2RA users were still on treatment 1 year after initiation. There was little difference in persistence between those patients with a history of acid-suppressive use and those who were newly initiated onto therapy.
Discussion
This study found a significant increase in the risk of any osteoporotic, hip and vertebral fracture in patients currently taking PPIs and increases in the risk of osteoporotic, hip and vertebral fracture in current users of H2RA, when compared to past users. In patients taking concomitant bisphosphonate and acid-suppressive medication, increases in risk were observed for any fracture and hip fracture with PPIs and for vertebral fracture with H2RAs. When these overall effects were stratified by defined daily dose, fracture risk increased with higher doses. However, increasing durations of use of acid-suppressive medication was associated with an attenuation of fracture risk.
The findings from the acid-suppressant cohort are broadly in line with previous studies of fracture risk and acid-suppressive medication. As with Yang et al. [10], a significant increase in the risk of hip fracture and trends with dose for both PPI and H2RA use were observed. However, the magnitude of effect was smaller in this study, and it did not demonstrate the same pattern of effects with cumulative use over time, as reported by Yang et al. and Targownik et al., who conducted a case-control study within a Canadian administrative claims database [10, 15]. Other than the study designs, the major difference between these studies was the choice of comparison group. Both case-control studies [10, 15] compared patients who had used acid-suppressive medication with those who had never used such drugs; whilst here, a time-dependent approach was used along with a comparison of current to past use in the acid-suppressant cohort. This allows the recency of exposure as well as intermittent use to be taken into account and reduces the likelihood of confounding by indication. The pattern of results and magnitude of effect are also comparable to those of Vestergaard et al. [11], with the exception of the increased risk of hip fracture with H2RA. As with Vestergaard et al. [11], we observed increases in any hip and vertebral fracture risk in those with current (or recent) use of PPIs, whilst no effects were observed at the radius/ulna. The lack of effect at this site may be due to these fractures tending to occur in younger age groups and to the role of non-skeletal factors. However, Vestergaard et al. [11] observed a protective effect on hip fracture risk, in contrast to this and previous studies [10, 16]. It is not clear why this should be; however, it is interesting to note that the reduction in hip-fracture risk was still apparent even in patients who had not been recently exposed to H2RAs, suggesting that it may not be related to the drug per se.
No previous studies examining the risk of fracture with concomitant acid-suppressant and bisphosphonate use have been located. In this study, increases in the risk of any and hip fracture were found for patients taking PPIs and bisphosphonates compared to bisphosphonates alone and increases in vertebral fracture risk for patients receiving H2RAs and bisphosphonates compared to bisphosphonates alone. The increased risk of hip fracture among patients taking concomitant bisphosphonate and PPI was of a similar magnitude to that observed in current versus past PPI users not using bisphosphonates. These findings suggest that bisphosphonate use does not cancel out the increased risk of fracture seen with acid-suppressant use.
The use of acid-suppression medication was widespread in this osteoporotic population. Over 20% of patients had received a prescription for a PPI or H2RA in the 6 months before they initiated bisphosphonate therapy, and in the 6 months after, over a quarter of patients had received an acid suppressant, 6% of whom had no history of their use. The initiation of acid-suppression medication in the first month in previous non-users was similar to that observed by Roughead et al. [9], who also found it represented a threefold increase in use compared to a control group. The first couple of months after the initiation of a new drug is the most likely period for drug-related adverse events to manifest. Therefore, it is likely that the excess prescriptions for acid-suppression medication seen by Roughead et al. [9] were prescribed in order to manage the dyspeptic symptoms that can be associated with bisphosphonate therapy. In this study, some patients were prescribed both acid suppressants and bisphosphonates on the same day, which may be an attempt by GPs to prevent the emergence of bisphosphonate-induced upper GI effects. In terms of persistence with acid-suppressive medication, this is high for the first 3 months of treatment, and although it subsequently falls rapidly, over a third of previous users and nearly a quarter of new users remain on treatment at 1 year.
The potential mechanism of action for the observed increased risk of fracture is not clear. An acidic environment facilitates the release of ionised calcium from insoluble calcium and, therefore, reducing the level of acidity in the stomach may lead to malabsorption of calcium. O’Connell et al. [17] found that 20 mg of omeprazole significantly reduced the absorption of calcium carbonate taken under fasting conditions in women aged 65 years and older. However, a study among 18 healthy adults did not find differences in calcium absorption after omeprazole treatment (intragastric pH 6.4) compared to non-users (intragastric pH 3.6) [18]. PPIs may also inhibit the osteoclastic proton transport system, which could potentially reduce bone resorption, an action that might be expected to provide a beneficial effect on fracture risk [19], although the effect of omeprazole is considerably more marked at the gastric proton pump than at the osteoclast proton pump [20], which may explain why no reduction in fracture risk was observed. In the Study of Osteoporotic Fractures, the use of acid-suppressive medication was not associated with changes in bone mineral density [12].
In our study, there was inverse association between duration of use of acid-suppressive medications and fracture risk, which does not support adverse effects on the bone. An alternative explanation for the observed increased risk of fracture is falls. No studies have been located which look explicitly at this issue; however, dizziness is listed in the Summary of Product Characteristics for omeprazole and lansoprazole [21, 22], which together accounted for 85% of the PPI prescriptions, and for ranitidine, which comprised almost two thirds of the H2RA prescriptions in this study. However, if falling were the main cause of the increased fracture risk, then an effect on fracture risk of the radius/ulna might be expected, along with a rapid attenuation of the risk of hip fracture after cessation of PPI treatment. However, no increase in fracture risk for the radius/ulna was observed and whilst the hazard rates for hip fracture decreased over time, they did so gradually over a period of months, rather than in days or weeks (data not shown). Furthermore, falling does not explain the increased risk of vertebral fracture seen with H2RA use.
Within the bisphosphonate cohort, it is feasible that those requiring the initiation of acid suppressants to counter the upper GI side effects may have poorer compliance with their osteoporosis treatment, thus, leading to an increased risk of fracture. Penning-van Beest et al. [23] found that gastrointestinal adverse events as measure by the new initiation of drugs such as antacids, H2RAs and PPIs was associated with lower persistence with bisphosphonates, whilst Rossini et al. [24] found the use of gastro-protective agents to be associated with both discontinuation and poor compliance. Although it is possible that poorer compliance may contribute to the increased risk of fracture, we did not find evidence for this when adjusting for poor bisphosphonate compliance. Furthermore, other factors must also play a role, given that the risks are similar to those seen with current PPI use.
The limitations of this study include the availability of antacids, calcium and vitamin D supplements over-the-counter; the lack of complete data on risk factors for fracture, such as diet, exercise, smoking, body mass index and family history and the use of prescriptions as a proxy for actual drug use, given that patients may be non-compliant with both acid suppressants [25] and bisphosphonates [26]. Although we adhered to the WHO definitions, it can be argued whether 20 mg omeprazole is equivalent to 30 mg esomeprazole. However, the impact of this potential misclassification is not high as only 4% of our PPI prescriptions regarded esomeprazole. A potential shortcoming of our study design is that we compared current users of acid suppressive medication to past users. The advantage of comparing current PPI users to past PPI users instead of non-users is that the severity of the underlying disease is better taken into account. We have used a similar study design to evaluate risk of fracture among users of oral glucocorticoids [27]. In this study, we have used the same assumption that any PPI-induced fracture risk is reversible after discontinuation. A sensitivity analysis showed that comparing current PPI users to patients who had stopped taking PPIs for >3 years did not substantially change the inverse duration-response relationship between PPI use and hip fracture risk.
In conclusion, this study found an association between the use of acid-suppressive medication and an increased risk of fracture, most notably, a dose-dependent association between hip fracture and PPI use, either alone or in combination with bisphosphonates. The increased fracture risk attenuated with prolonged use of acid-suppressive medication. Given the frequency of co-prescription of acid-suppressive medication and bisphosphonates, this issue requires further attention.
References
Dennison E, Mohamed MA, Cooper C (2006) Epidemiology of osteoporosis. Rheum Dis Clin N Am 32:617–629
Bass E, French DD, Bradham DD et al (2007) Risk-adjusted mortality rates of elderly veterans with hip fractures. Ann Epidemiol 17(7):514–519
Leibson CL, Tosteson AN, Gabriel SE et al (2002) Mortality, disability, and nursing home use for persons with and without hip fracture: a population-based study. J Am Geriatr Soc 50(10):1644–1650
Van Staa TP, Dennison EM, Leufkens HGM et al (2001) Epidemiology of fractures in England & Wales. Bone 29(6):517–522
Nevalainen TH, Hiltunen LA, Jalovaara P (2004) Functional ability after hip fracture among patients home-dwelling at the time of fracture. Cen Eur J Public Health 12(4):211–216
Osnes EK, Lofthus CM, Meyer HE et al (2004) Consequences of hip fracture on activities of daily life and residential needs. Osteoporos Int 15(7):567–574
Biswas PN, Wilton LV, Shakir SAW (2003) Pharmacovigilance study of alendronate in England. Osteoporos Int 14:507–514
Barrera BA, Wilton LV, Harris S et al (2005) Prescription-event monitoring study on 13, 164 patients prescribed risedronate in primary care in England. Osteoporos Int 16:1989–1998
Roughead EE, McGeechan K, Sayer GP (2004) Bisphosphonate use and subsequent prescription of acid suppressants. Br J Clin Pharmacol 57(6):813–816
Yang YX, Lewis JD, Epstein S et al (2006) Long-term proton pump inhibitor therapy and risk of hip fracture. JAMA 296(24):2947–2953
Vestergaard P, Rejnmark L, Mosekilde L (2006) Proton pump inhibitors, histamine H2 receptor antagonists, and other antacid medications and the risk of fracture. Calcif Tissue Int 79(2):76–83
Yu E, Shinoff C, Blackwell T, Ensrud K, Hillier T, Bauer C (2006) Use of acid-suppressive medications and risk of bone loss and fracture in postmenopausal women. J Bone Min Res 21(Suppl. 1):S281
Van Staa TP, Leufkens HGM, Abenhaim L et al (2000) Use of oral corticosteroids and risk of fracture. J Bone Miner Res 15(6):993–1000
Van Staa TP, Leufkens HGM, Cooper C (2002) Utility of medical and drug history in fracture risk prediction among men and women. Bone 31(4):508–514
Targownik LE, Lix LM, Metge CJ, Prior HJ, Leung S, Leslie WD (2008) Use of proton pump inhibitors and risk of osteoporosis-related fractures. CMAJ 179(4):319–326
Grisso JA, Kelsey JL, O’Brien LA et al (1997) Risk factors for hip fracture in men. Hip Fracture Study Group. Am J Epidemiol 145(9):786–793
O’Connell MB, Madden DM, Murray AM et al (2005) Effects of proton pump inhibitors on calcium carbonate absorption in women: a randomized crossover trial. Am J Med 118:778–781
Serfaty-Lacrosniere C, Wood RJ, Voytko D, Saltzman JR, Pedrosa M, Sepe TE, Russell RR (1995) Hypochlorhydria from short-term omeprazole treatment does not inhibit intestinal absorption of calcium, phosphorus, magnesium or zinc from food in humans. J Am Coll Nutr 14(4):364–368
Zaidi M (1990) Modularity of osteoclast behaviour and “mode-specific” inhibition of osteoclast function. Biosci Rep 10(6):547–556
Mattsson JP, Väänänen K, Wallmark B et al (1991) Omeprazole and bifailomycin, two proton pump inhibitors: differentiation of their effects on gastric, kidney and bone H(+)-translocating ATPases. Biochim Biophys Acta 1065(2):261–268
AstraZeneca (2008) Losec (omeprazole). Summary of Product Characteristics. AstraZeneca, London
Wyeth (2007) Zoton FasTab (lansoprazole). Summary of Product Characteristics. Wyeth, Madison
Penning-van Beest FJ, Goettsch WG, Erkens JA et al (2006) Determinants of persistence with bisphosphonates: a study in women with postmenopausal osteoporosis. Clin Ther 28(2):236–242
Rossini M, Bianchi G, Di Munno O et al (2006) Determinants of adherence to osteoporosis treatment in clinical practice. Osteoporos Int 17:914–921
Hungin AP, Rubin G, O’Flanagan H (1999) Factors influencing compliance in long-term proton pump inhibitor therapy in general practice. Br J Gen Pract 49(443):463–464
Cramer JA, Gold DT, Silverman SL et al (2007) A systematic review of persistence and compliance with bisphosphonates for osteoporosis. Osteoporos Int 18(8):1023–1031
De Vries F, Bracke M, Leufkens HGM, Lammers JW, Cooper C, van Staa TP (2007) Fracture risk with intermittent high-dose oral glucocorticoids therapy. Arthritis Rheum 56(1):208–214
Acknowledgements
This study was funded by Servier Laboratories Limited, UK. GPRD is owned by the UK Department of Health and operates within the Medicines and Healthcare products Regulatory Agency (MHRA). GPRD is funded by the MHRA, Medical Research Council, various universities, contract research organisations and pharmaceutical companies. The Department of Pharmacoepidemiology and Pharmacotherapy, Utrecht Institute for Pharmaceutical Sciences has received unrestricted funding for pharmacoepidemiological research from GlaxoSmithKline, Novo Nordisk, private–public funded Top Institute Pharma (www.tipharma.nl and includes co-funding from universities, government, and industry), the Dutch Medicines Evaluation Board and the Dutch Ministry of Health. The views expressed in this paper are those of the authors and do not reflect the official policy or position of the Medicines and Healthcare products Regulatory Agency, UK.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
de Vries, F., Cooper, A.L., Cockle, S.M. et al. Fracture risk in patients receiving acid-suppressant medication alone and in combination with bisphosphonates. Osteoporos Int 20, 1989–1998 (2009). https://doi.org/10.1007/s00198-009-0891-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-009-0891-4