Abstract
We studied the effect of proton pump inhibitors, histamine H2 receptor antagonists, and other types of antacid drugs on fracture risk. All cases were subjects with any fracture sustained during the year 2000 (n = 124,655). For each case, three controls (n = 373,962) matched on age and gender were randomly drawn from the background population. The primary exposure variables were use of proton pump inhibitors, histamine H2 antagonists, and other antacid drugs. Adjustments were made for several confounders, including diagnosis of an ulcer, nonsteroidal anti-inflammatory drug use, use of histamine H1 antagonists, stomach resection, previous fracture, and use of corticosteroids. The effect of dose was examined by stratifying for cumulated dose (defined daily dose). Use of proton pump inhibitors was associated with an increase in fracture risk for use within the last year [odds ratio (OR) = 1.18, 95% confidence interval (CI) 1.12–1.43 for overall fracture risk; OR = 1.45, 95% CI 1.28–1.65 for hip fractures; and OR = 1.60, 95% CI 1.25–2.04 for spine fractures). Histamine H2 antagonists were associated with a decreased fracture risk if they had been used within the last year (OR = 0.88, 95% CI 0.82–0.95 for any fracture, OR = 0.69, 95% CI 0.57–0.84 for hip fractures). Other antacids were not associated with overall fracture risk but were associated with hip and spine fractures. Proton pump inhibitors appeared to be associated with a limited increase in fracture risk, in contrast to histamine H 2 antagonists, which seemed to be associated with a small decrease in fracture risk. In all cases, the changes in risk estimates were small and the clinical significance was limited.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Drugs used to inhibit gastric acidity include proton pump inhibitors (PPIs), histamine H2 receptor antagonists (H2 blockers), and other antacid medications including bicarbonate-containing preparations and preparations containing aluminum and magnesium along with agents with specific effects on prostaglandin synthesis. These drugs may interfere with bone metabolism and thus affect the risk of fracture. PPIs, such as omeprazole, esomeprazole, pantoprazole, etc., inhibit the proton pump in the gastric mucosa, thus reducing acid output into the stomach and duodenum, in contrast to H2 blockers, which decrease acid secretion by interfering with the H2 receptor. Osteoclasts also possess proton pumps, which are used during the excretion of H+ ions for the resorption of bone [1–4]. Osteoclast-selective PPIs may therefore be interesting antiresorptive agents [5] with a potential to prevent fractures [6–9]. However, no fracture studies exist.
In men, the use of cimetidine (H2 blocker) has been linked to a 2.5-fold increase in hip fracture risk [10]. However, H2 receptor blockers have been found to have no influence on bone mineral density (BMD) in humans [11]. H2 blockers may thus be potentially harmful in humans.
Aluminum-containing antacids may inhibit intestinal phosphate absorption, inducing hypophosphatemia and impaired mineralization. In patients with impaired renal function, aluminum may impair mineralization. Calcium-containing antacids may increase calcium absorption and thus increase the bone mineral. These drugs may thus have clinically relevant influences on fracture risk.
PPIs may thus differ from other antacids, and particularly from the histamine H2 receptor blockers, in their effects on bone turnover, BMD, and thus eventually fracture risk.
We therefore undertook a population-based study on fracture risk among users compared to never users of PPIs, histamine H2 blockers, and other antacid drugs in order to investigate if these drugs were associated with a decreased or increased fracture risk. Any change in fracture risk associated with use of antacid drugs may have a significant impact at the population level as these drugs are widely used.
Subjects and Methods
Source Population
The Danish population comprises approximately 5.3 million individuals. The population is relatively homogeneous, with most individuals being Caucasian. The data were retrieved from registers managed by the National Board of Health, the Danish Medicines Agency, and the National Bureau of Statistics for administrative purposes.
Study Design
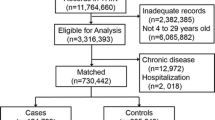
The study was designed as a case-control study. All subjects sustaining a fracture during the year 2000 in Denmark were included as cases (n = 124,655), and for each case three subjects of the same age (same birth year) and gender were randomly selected from the background population as controls (n = 373,962). Controls were selected using the incidence-density sampling technique [12]; i.e., controls had to be alive and at risk for fracture diagnosis at the time the corresponding case was diagnosed. The follow-up time was time until fracture in cases and a corresponding dummy date among controls. Cases occurred only once in the analyses, with the first occurrence of a fracture during the year 2000.
End Points
The study end points were occurrence of any fracture (ICD-10 codes S02.0–S02.9, S07.0–S07.9, S12.0–S12.9, S22.0–S22.9, S32.0–S32.8, S42.0–S42.9, S52.0–S52.9, S62.0–S62.9, S72.0–S72.9, S82.0–S82.9, S92.0–S92.9) between January 1, 2000, and December 31, 2000. In Denmark, almost all patients with fractures are managed in the hospital system (including emergency rooms) [13], and even fractures sustained abroad are registered upon return, for insurance reasons. The capture of fractures is thus very high. The validity of a fracture diagnosis is around 93% [14].
Exposure Variables
The exposure variables were (1) use of PPIs, (2) use of histamine H2 antagonists, (3) use of other antacids, (4) use of antihistamine drugs (histamine H1 antagonists), (5) prior use of nonsteroidal anti-inflammatory drugs (NSAIDs), (6) prior stomach or duodenal ulcer, and (7) prior stomach or duodenal resection.
The confounders were (1) ever use of other drugs important to fracture risk (corticosteroids [15], anxiolytics and sedatives, neuroleptics, antidepressants, antiepileptics [16]); (2) comorbidity (expressed as the Charlson index, see below), number of bed days in 1999 (the year before the fracture), and number of contacts to general practitioner or practising specialist; (3) social variables (income, education level, living alone or with someone, working or not); and (4) other important variables associated with fracture risk (prior fracture [17], alcoholism). The Charlson index is an index of 19 comorbid conditions including heart disease, lung disease, liver disease, kidney disease, cancer, and acquired immunodeficiency syndrome (AIDS) [18].
Presence of alcoholism or a prior fracture was defined as a prior contact under such a diagnosis from 1977 to the date of censoring from the National Hospital Discharge Register or from 1968 to the date of censoring from the Psychiatric Central Register or at least one prescription of disulfiram from 1996 to the date of censoring from the National Pharmacoepidemiological Database [19].
Registers Used
We retrieved the information on fracture occurrence and occurrence of other diseases, prior fractures, and diagnosis of alcoholism from the National Hospital Discharge Register between 1977 and the date of censoring [20] and the Psychiatric Central Register for the period 1968 to the date of censoring [21]. We obtained information on the use of prescribed drugs from the Danish Medicines Agency for the period 1996–2000. The average daily dose of drug was calculated as the cumulated dose divided by the time from the date of first prescription to the date of censoring. In the actual analyses, the data do not contain information on drugs sold over the counter.
The National Hospital Discharge Register was founded in 1977 [20]. It covers all inpatient contacts from 1977 to 1994 and, from 1995, also all outpatient visits to hospitals, outpatient clinics, and emergency rooms [20]. Upon discharge, the physician codes the reason for the contact using the International Classification of Diseases (ICD) system. The code used is at the discretion of the individual physician. The register has a nationwide coverage and almost 100% capture of contacts [20]. In general, the validity of registrations is high [22], especially for fractures, where a precision of 97% has been reported for those treated both on an inpatient and on an outpatient basis via emergency rooms (e.g., forearm fracture) [14].
The Psychiatric Central Register was founded in 1968 and covers all in- and outpatient contacts to Danish mental hospitals [21]. It has nationwide coverage, and high validity of diagnoses has been reported [13]. This register also uses the ICD system for coding contacts.
The Danish Medicines Agency keeps a nationwide register of all drugs sold at pharmacies throughout the country from 1996 on (National Pharmacological Database run by Danish Medicines Agency, http://www.dkma.dk). Any drugs bought are registered with ATC (Anatomical therapeutic chemical classification system) code, dosage sold, and date of sale for the period January 1 1996 to December 31, 2000. As all sales are registered to the individual who redeemed the prescription, the capture and validity are high [23].
PPIs were available only on prescription during the study period, while H2 blockers and other antacids were also available over the counter.
Exposure was calculated as cumulated number of defined daily dosages (DDDs) redeemed of the drug group in question from January 1, 1996, to the date of fracture or the date of censoring among cases or controls. DDD in this report is thus the sum of drugs used. Also, an analysis of average daily use (DDD/day) was performed. In this analysis, the cumulated number of DDDs used during the year 2000 was divided by the time from first use in the year 2000 to the day of fracture or comparable dummy date in controls. This approach was chosen as many of these drugs are not taken regularly but rather for a period of time while symptoms of dyspepsia are present; i.e., 15 DDDs bought may not be consumed during 15 days but for, say, 5 + 7 + 3 days over maybe 3 months.
In this report, DDDs were used to better allow comparison of different drugs, which come in a variety of doses. The DDD system is validated and based on the World Health Organisation Collaborating Centre for Drug Statistics Methodology (http://www.whocc.no/atcddd/, accessed December 8, 2005).
To compare the consumption in the study sample (only sales on prescription), use among controls (DDD/participant/year) was compared to that of the general population (sales on prescription and over the counter, not available on an individual basis). Data on sales are available from the Danish Medicines Agency (http://www.dkma.dkw.dkma.dk).
We linked these sources of information through the Central Person Register Number, which is a unique registration code given to every inhabitant—to some degree similar to the U.S. social security number—that allows registration on an individual basis.
The project was approved by the National Board of Health and is subject to control by the National Data Protection Agency.
Statistical Analyses
Mean and standard deviation were used as descriptive statistics. Crude and adjusted odds ratios (ORs) and 95% confidence intervals (CIs) were calculated. A conditional logistic regression analysis was used to assess the association between any fracture and the exposure variable.
Crude and adjusted ORs were calculated. Adjusted ORs were compared by direct comparison of estimates [24].
Analyses were performed using STATA 8.1 (StataCorp, College Station, TX) and SPSS 13.0 (SPSS Inc., Chicago IL), both in the Unix version.
Results
Table 1 shows baseline characteristics of the fracture cases and controls. The cases and controls were well matched concerning age and gender. The fracture cases more often were retired and, thus, had a lower income. The cases also more often were unmarried. The comorbidity and use of drugs in general were higher among cases than controls.
Table 2 shows age and gender characteristics of users of the different types of antacids. Users of PPIs and histamine H2 antagonists were of approximately similar age and had a similar gender distribution, while users of other antacids were older and more frequently women.
Table 3 shows the relative risk of any fracture associated with the use of different drugs used for treatment of gastric and duodenal ulcers. PPIs and the other antacids were associated with a small increase in overall fracture risk, while a decrease was seen for H2 antagonists. Histamine H1 antagonists were only slightly associated with fracture risk. Ulcers of the duodenum and stomach were associated with a limited increase in fracture risk, especially if the ulcer had occurred within the last year. A similar but more pronounced trend was seen for NSAID use and for patients who had undergone surgery with gastric resection.
An association with time since last use was seen. For less than 1 year since last use, the decrease in relative fracture risk associated with H2 antagonists was more pronounced and the increase in relative fracture risk with PPIs and other antacids was more pronounced. For more than 1 year since last use, the risk disappeared for PPIs and other antacids.
Table 4 shows the relative fracture risk at osteoporotic fracture sites. For hip and spine fractures, a pattern similar to that for overall fracture risk was seen, with a decrease for H2 blockers and an increase for PPIs and the other antacids. For forearm fractures, no change in risk was associated with any of the drug classes. Ulcers were not associated with fracture risk. Histamine H1 antagonists were not associated with fracture risk. Again, an association with time since last use was seen, with a more pronounced association for less than 1 year since last use and a disappearance of the association with more than 1 year since last use.
Table 5 shows the adjusted relative risk stratified by dose of the drug in question. For forearm fractures, no relationship was observed with any of the drug classes. For PPIs, an increase in relative fracture risk without relationship to dose was seen for overall fracture risk as well as hip and spine fracture risk. For H2 blockers, a trend toward a decrease in relative fracture risk was seen with increasing dose for any fracture and hip fractures. A decrease with no trend was seen for spine fractures. Histamine H1 antagonists in general were not associated with fracture risk.
For other types of antacids, a biphasic pattern was seen: no increase at low doses, a significant increase at medium doses, and a decline in relative fracture risk from medium to high doses.
A direct comparison of estimates showed that the ORs were significantly lower for H2 blockers than for PPIs at all doses for any fracture type and for hip fractures and at 25–99 DDD and ≥100 DDD for the spine.
Table 6 shows the same associations as Table 4 but for daily dose. Again, there was an increase in relative fracture risk for PPIs and other antacids for overall fracture risk and the risk of hip and spine fractures, whereas a decrease was seen for histamine H2 receptor antagonists. In the forearm, no general association was seen.
No overall gender differences were observed (data not shown).
During the observation period, the mean numbers of DDDs/year among controls were 2.97 for H2 blockers, 4.35 for PPIs, and 0.78 for other antacids. From the Danish Medicines Agency, numbers for the entire population were 2.39 for H2 blockers, 4.92 for PPIs, and 2.96 for other antacids; i.e., our numbers were close to those for the entire population for PPIs and H2 blockers but significantly underestimated for other antacids.
Discussion
In this large-scale case-control study, we observed a trend toward a decrease in relative fracture risk with histamine H2 receptor blockers and an increase with PPIs, the difference being statistically significant. There was a dose-response relationship for H2 blockers, supporting a causal relationship, while no dose-response relationship was present for PPIs.
The results on H2 blockers are in conflict with those of Grisso et al. [10], who reported an increase in hip fracture risk with use of cimetidine. That study was much smaller than the present study. They adjusted for smoking, body mass index, and comorbidity and had data for education level and marital status as socioeconomic variables [10]. However, neither education level nor marital status was included in their final model. In the study by Grisso et al. [10], the estimate for hip fractures changed only little (from 2.5 to 2.0) upon adjustment, in contrast to our study. They did not include social class [10], and this may account for some of the differences between the results as the risk associated with H2 blockers was significantly attenuated after introduction of covariates in our study. This is probably caused by the fact that ulcers and, thus, use of antacids may be more frequent in subjects from lower social classes, who also may be more prone to fractures due to, e.g., alcoholism as alcoholism may be linked to gastritis and ulcers. Grisso et al. [10] adjusted for alcohol intake but not for social class, and alcohol intake may be underreported.
In rats, cimetidine has been shown to prevent osteopenia by preventing osteoclast differentiation induced by histamine [25]. Furthermore, studies in rats on histamine H2 antagonists have demonstrated antiresorptive properties [26, 27]. In this context, H2 receptors seem to play a more central role for osteoclasts than H1 receptors [28], in accordance with our findings of no effects of H1 receptor blocking drugs (antihistamines). H2 blockers may thus increase BMD, and this could be one mechanism underlying the decrease in fracture risk.
Omeprazole has been shown to inhibit gastric proton pumps at physiological concentrations, whereas the inhibition of osteoclast and other tissue H+-ATPase activity such as osteoclast proton pumps was much less pronounced [29], and this may explain why no decrease in fracture risk was seen in our study.
In humans, administration of omeprazole has been shown to alter biochemical markers of bone turnover when patients with gastric ulcers on stable histamine H2 blocker therapy were switched to omeprazole (PPI) treatment [30]. Among patients shifted from H2 blockers to omeprazole, decreases in urine hydroxyproline and calcium were observed in comparison to patients on continued H2 blocker therapy [30]. However, it should be noted that the study did not compare changes over time and, upon direct comparison, the changes over time in patients treated with PPIs seemed similar to those in patients treated with H2 blockers [30]. Serum intact parathyroid hormone, alkaline phosphatase, osteocalcin, and tartrate-resistant phosphatase all increased among patients shifted to omeprazole compared to patients on continued H2 blocker therapy [30], suggesting combined antiresorptive and anabolic properties of PPIs. Again, upon comparison to the changes over time in patients treated with PPIs, the results seemed similar to those in patients treated with H2 blockers [30]. In the evaluation of this study [30], it should be remembered that the effect was observed in patients already on H2 therapy and may thus signal reactions to removal of the H2 blockers. In patients with cystic fibrosis on lanzoprazole, bone mineral content has been shown to increase [31]. In rats, no effect of omeprazole on bone mineral content has been observed [32].
The reasons PPIs were associated with an increase in fracture risk while H2 blockers were not are not clear from this study. Theoretical considerations point at an antiresorptive potential [5]; however, the clinical effect on osteoclasts may be too low for a significant effect on bone mineral [29]. The increased risk may be linked to a decrease in calcium absorption, with secondary hyperparathyroidism leading to a negative calcium balance despite the decrease in urine calcium [30]. The increase in PTH may induce bone loss and increased fracture risk [24]. Further studies are thus needed.
PPIs were available only on prescription, while H2 blockers and other antacids were available over the counter. This may have underestimated the risk associated with these drugs. However, for H2 blockers and PPIs, the study did not seem to significantly under- or overestimate consumption. On the other hand, a doctor may have diagnosed those redeeming a prescription, and the likelihood of an ulcer may be higher in them than in patients buying the drugs over the counter.
As the risk estimates associated with H2 blockers and PPIs in general were small, the clinical consequences were limited. In this view, the antacid drugs may be rather safe in terms of fracture risk.
NSAIDs were associated with an increased fracture risk, an effect not countered by the antacid drugs. The association between gastric surgery and fracture risk may be due to either malabsorption of calcium and other nutrients or lack of specific hormones, e.g., ghrelin.
The main strengths of our study are the uniformly organized health-care system, allowing a large-scale population-based design and the use of data on exposure and confounders that are collected before the date of fracture. Thus, recall bias did not influence data collection.
The weaknesses include potential selection bias, e.g., the use of routine hospital discharge diagnoses of fractures coded by hospital doctors to ascertain case status. Some coding errors probably occurred. However, misclassification of case status is unlikely to be related to prescription of antacid drugs before hospitalization, and any nondifferential misclassification will lead to underestimation of our risk estimates. Moreover, the positive predictive value of hip fracture discharge diagnoses from Danish hospitals has previously been shown to be as high as 93% [33], and the risk of misclassification of case status is thus most likely of minor importance.
We cannot exclude that information biases may have influenced our results; e.g., we had no information on patient compliance in our study since redeeming a prescription was used as a proxy for actual use of a drug. However, the patients had paid part of the cost of the drug, which increases the likelihood of compliance. Furthermore, data on drugs, including antacid drugs, administered during hospitalization are not registered in the prescription database and, therefore, were not included in our study. Both of these uncertainties could have led to misclassification of exposure. However, the contribution from this source is very limited as only few days are spent in hospital.
Although we adjusted for several potential confounding factors in the statistical analyses, our results may still be influenced by potential confounding factors not included in the analyses, e.g., smoking, physical activity, differences in body weight, use of calcium/vitamin D supplements, and sun exposure, or by residual confounding due to the use of crude measures (risk of falling).
In conclusion, PPIs appear to be associated with an increased fracture risk, in contrast to histamine H2 antagonists, which seem to be associated with a decreased fracture risk. The changes in risk estimates were small in all instances and may have limited clinical consequences. However, further studies in the field are needed.
References
Farina C, Gagliardi S (2002) Selective inhibition of osteoclast vacuolar H+-ATPase. Curr Pharm Des 8:2033–2048
Sahara T, Itoh K, Debari K, et al. (2003) Specific biological functions of vacuolar-type H+-ATPase and lysosomal cysteine proteinase, cathepsin K, in osteoclasts. Anat Rec A Discov Mol Cell Evol Biol 270:152–161
Sasaki T (1996) Recent advances in the ultrastructural assessment of osteoclastic resorptive functions. Microsc Res Tech 33:182–191
Shibata T, Amano H, Yamada S, et al. (2000) Mechanisms of proton transport in isolated rat osteoclasts attached to bone. J Med Dent Sci 47:177–185
Gagliardi S, Nadler G, Consolandi E, et al. (1998) 5-(5,6-Dichloro-2-indolyl)-2-methoxy-2,4-pentadienamides: novel and selective inhibitors of the vacuolar H+-ATPase of osteoclasts with bone antiresorptive activity. J Med Chem 41:1568–1573
Rzeszutek K, Sarraf F, Davies JE (2003) Proton pump inhibitors control osteoclastic resorption of calcium phosphate implants and stimulate increased local reparative bone growth. J Craniofac Surg 14:301–307
Sundquist K, Lakkakorpi P, Wallmark B, et al. (1990) Inhibition of osteoclast proton transport by bafilomycin A1 abolishes bone resorption. Biochem Biophys Res Commun 168:309–313
Visentin L, Dodds RA, Valente M, et al. (2000) A selective inhibitor of the osteoclastic V-H+-ATPase prevents bone loss in both thyroparathyroidectomized and ovariectomized rats. J Clin Invest 106:309–318
Xu J, Feng HT, Wang C, et al. (2003) Effects of bafilomycin A1: an inhibitor of vacuolar H+-ATPases on endocytosis and apoptosis in RAW cells and RAW cell-derived osteoclasts. J Cell Biochem 88:1256–1264
Grisso JA, Kelsey JL, O’Brien LA, et al. (1997) Risk factors for hip fracture in men. Hip Fracture Study Group. Am J Epidemiol 145:786–793
Adachi Y, Shiota E, Matsumata T, et al. (1998) Bone mineral density in patients taking H2-receptor antagonist. Calcif Tissue Int 62:283–285
Wacholder S, McLaughlin JK, Silverman DT, et al. (1992) Selection of controls in case-control studies. I. Principles. Am J Epidemiol 135:1019–1028
Vestergaard P, Emborg C, Støving RK, et al. (2002) Fractures in patients with anorexia nervosa, bulimia nervosa, and other eating disorders - a nation-wide register study. Int J Eat Disord 32:301–308
Vestergaard P, Mosekilde L (2002) Fracture risk in patients with celiac disease, Crohn’s disease, and ulcerative colitis: a nation-wide follow-up study in 16,416 patients in Denmark. Am J Epidemiol 156:1–10
Vestergaard P, Rejnmark L, Mosekilde L (2005) Fracture risk associated with systemic and topical corticosteroids. J Intern Med 257:374–384
Vestergaard P, Rejnmark L, Mosekilde L (2004) Fracture risk associated with use of anti-epileptic drugs. Epilepsia 45:1330–1337
Klotzbuecher CM, Ross PD, Landsman PB, et al. (2000) Patients with prior fractures have an increased risk of future fractures: a summary of the litterature and statistical synthesis. J Bone Miner Res 15:721–739
Charlson ME, Pompei P, Ales KL, et al. (1987) A method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chron Dis 40:373–383
Kanis JA, Johansson H, Johnell O, et al. (2005) Alcohol intake as a risk factor for fracture. Osteoporosis Int 16:737–742
Andersen TF, Madsen M, Jørgensen J, et al. (1999) The Danish National Hospital Register. Dan Med Bull 46:263–268
Munk-Jørgensen P, Mortensen PB (1997) The Danish Psychiatric Central Register. Dan Med Bull 44:82–84
Mosbech J, Jørgensen J, Madsen M, et al. (1995) The Danish National Patient Register: evaluation of data quality [in Danish]. Ugeskr Læger 157:3741–3745
Nielsen GL, Sørensen HT, Zhou W, et al. (1997) The pharmaco-epidemiologic prescription database of north Jutland. Int J Risk Saf Med 10:203–205
Vestergaard P, Mollerup CL, Frøkjær VG, et al. (2000) Cohort study of risk of fracture before and after surgery for primary hyperparathyroidism. BMJ 321:598–602
Yamaura K, Yonekawa T, Nakamura T, et al. (2003) The histamine H2-receptor antagonist, cimetidine, inhibits the articular osteopenia in rats with adjuvant-induced arthritis by suppressing the osteoclast differentiation induced by histamine. J Pharmacol Sci 92:43–49
Lesclous P, Guez D, Baroukh B, et al. (2004) Histamine participates in the early phase of trabecular bone loss in ovariectomized rats. Bone 34:91–99
Lesclous P, Guez D, Saffar JL (2002) Short-term prevention of osteoclastic resorption and osteopenia in ovariectomized rats treated with the H2 receptor antagonist cimetidine. Bone 30:131–136
Dobigny C, Saffar JL (1997) H1 and H2 histamine receptors modulate osteoclastic resorption by different pathways: evidence obtained by using receptor antagonists in a rat synchronized resorption model. J Cell Physiol 173:10–18
Mattsson JP, Vaananen K, Wallmark B, et al. (1991) Omeprazole and bafilomycin, two proton pump inhibitors: differentiation of their effects on gastric, kidney and bone H+-translocating ATPases. Biochim Biophys Acta 1065:261–268
Mizunashi K, Furukawa Y, Katano K, et al. (1993) Effect of omeprazole, an inhibitor of H+,K+-ATPase, on bone resorption in humans. Calcif Tissue Int 53:21–25
Tran TM, Van den NA, Hendriks JJ, et al. (1998) Effects of a proton-pump inhibitor in cystic fibrosis. Acta Paediatr 87:553–558
Persson P, Gagnemo-Persson R, Chen D, et al. (1993) Gastrectomy causes bone loss in the rat: is lack of gastric acid responsible? Scand J Gastroenterol 28:301–306
Hoidrup S, Grønbæk M, Gottschau A, et al. (1999) Alcohol intake, beverage preference, and risk of hip fracture in men and women. Am J Epidemiol 149:993–1001
Acknowledgments
Danmarks Statistik (Statistics Denmark) is acknowledged for the help without which this project would not have been possible. Research Librarian Ms. Edith Clausen is acknowledged for invaluable help with the references. The Danish Medical Research Council granted financial support (grant 22-04-0495).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vestergaard, P., Rejnmark, L. & Mosekilde, L. Proton Pump Inhibitors, Histamine H2 Receptor Antagonists, and Other Antacid Medications and the Risk of Fracture. Calcif Tissue Int 79, 76–83 (2006). https://doi.org/10.1007/s00223-006-0021-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-006-0021-7