Abstract
Summary
Osteoporosis beliefs were assessed in immigrant Chinese women in Chinatown, Chicago. Results from a survey utilizing the Osteoporosis Health Belief Scale showed that women expressed concern about osteoporosis but lacked both knowledge of preventive care and health motivation.
Introduction
The objective of this study was to assess osteoporosis beliefs in immigrant Chinese women in Chinatown, Chicago.
Methods
In a community-based health fair, osteoporosis knowledge and self-efficacy among postmenopausal Chinese immigrants were assessed using the translated Osteoporosis Health Belief Scale. Bone mineral density (BMD) was assessed with calcaneal ultrasound.
Results
The study population included 94 women with mean age of 51 ± 9 years, mean length of residence in the United States of 9 ± 7 years, and 73% (n = 76) of whom were recent immigrants. Women expressed concern about the seriousness of osteoporosis and their relative susceptibility to osteoporosis. In particular, women with a prior fracture reported higher seriousness to osteoporosis. Nonetheless, women exhibited low health motivation and low awareness of the benefits of calcium and exercise. Bone densitometry results corresponded to a T score of −1.2 ± 1.5. Multiple regression analysis revealed that a younger age and longer length of residence in the USA were associated with higher BMD.
Conclusion
Chinese immigrant women in Chicago exhibit concern regarding osteoporosis, but are unaware of the benefits of calcium and exercise, and exhibit low health motivation. Chinese women in Chinatown lack necessary knowledge about osteoporosis to develop adequate self-efficacy. Public health initiatives should be undertaken among recent immigrant Chinese women.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a chronic disease characterized by reduced bone strength and increased risk for fracture. Asian ancestry is considered a risk factor for osteoporosis [1]. The National Osteoporosis Risk Assessment (NORA) multi-ethnic cohort of 220,000 women identified that Asian-American women had the lowest bone mineral density (BMD) compared to other ethnicities including Caucasians, Latinos, African-Americans, and native Americans [2, 3]. Chinese women have been noted to have lower BMD at the lumbar spine, total hip, and femoral neck across a wide spectrum of age groups when compared to Caucasian women [4]. Furthermore, when compared to both Caucasian women and US-born Asian-American women, immigrant Chinese women have yet lower average BMD [5]. Thus, foreign-born Chinese women may be considered a high-risk group for osteoporosis. The need to assess Chinese women’s knowledge of osteoporosis remains high as health disparities continue to exist [6].
Minimizing the effects of osteoporosis in postmenopausal women entails adequate weight-bearing exercise, calcium intake, and appropriate medications; but successful promotion of these interventions, like all others, requires an assessment of knowledge, attitudes, and beliefs. Few studies have looked into general perceptions of osteoporosis among immigrant Chinese women. Prior studies that have looked into general knowledge of osteoporosis in this population in New York found that osteoporosis knowledge was low [3, 7]. Chinese women living in China are believed to have a general lack of knowledge regarding the effects and treatment options for menopause [8]. Similarly, immigrant Chinese-American women residing in New York City reported the belief that people with osteoporosis were in constant pain. Two thirds of the women believed that bone density testing also caused pain [3]. While limited data on bone health knowledge exist, there have been fewer studies that look at the perceptions of self-efficacy or motivations to maintain proper bone health among immigrant Chinese-American women.
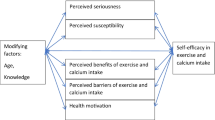
The objective of this study was to identify health beliefs in Chinese immigrants about osteoporosis. Knowledge of health beliefs held by this community is crucial in order to develop effective educational strategies. The two theoretical models employed include the health belief model (HBM) and the precaution adoption process model (PAPM); these models have been previously used in osteoporosis studies in Caucasian women [9–14]. Therefore, this study aims to assess osteoporosis health beliefs of Chinese immigrant women living in the ethnic enclave of Chinatown, Chicago.
Materials and methods
Survey development
The HBM [12] is a model frequently used to assess the likelihood of behavior change. The HBM proposes that health behaviors are more likely to occur if an individual feels a perceived susceptibility to an illness, that the consequences of the illness are serious, and that the barriers and benefits to the healthful action are cost-effective, and displays a sense of health motivation [15]. The osteoporosis health belief survey (OHBS) was developed by Kim et al. [16]. OHBS is a 35-item, five-point Likert scale that evaluates susceptibility and seriousness of osteoporosis, benefits and barriers to calcium and exercise, and general health motivation. These measures have been validated in prior studies [12, 17–19].
Precaution adoption process model
Behavior change is not an “all or none” event but is often a dynamic process, with individuals proceeding through a number of stages prior to adoption of a behavior. Weinstein proposed the PAPM [20]. Weinstein suggests seven possible stages in which an individual may be with respect to the adoption of a specific behavior change. In stage 1, an individual is unaware of the issue. Stage 2 finds the individual aware but “unengaged.” In stage 3, an individual decides whether he will take the suggested precaution (e.g., osteoporosis treatment). This decision leads one to either stage 4, where one has decided not to act, or stage 5, where one has made the decision to act. Stage 6 finds the individual acting (e.g., discussing with her physician the best course of action, such as beginning treatment), and stage 7 is the maintenance of these actions for at least 6 months [20, 21].
Participants
Chicago’s Chinese immigrant population is particularly concentrated in Chicago’s Cermak Chinatown. Participants were recruited from an annual community-run health fair located at the Chinese Consolidated Benevolent Association Community Center. The Chinatown health fair was advertised through fliers posted on Chinatown businesses and articles published in several Chinese newspapers serving the Chicago area. Approximately 300 people from the local Chinese community attended the health fair. Women older than 40 years of age were invited to participate in the study.
Data collection
Research staff personally conducted surveys with the assistance of interpreters. Consents and questionnaires were translated into written Chinese and then back translated by a blinded translator to assess for accuracy of translation. To ensure cultural sensitivity and overcome language barriers, female researchers fluent in Cantonese and Mandarin were present to obtain consent. Surveys were administered in written Chinese, and translators were available to assist illiterate patients.
Measures
Survey instrument
The survey included questions regarding fracture history, perceived likelihood of developing osteoporosis, stroke, heart disease, and breast cancer scored on a five-point Likert scale (0 = very unlikely to 5 = most likely) [21], the stage of change, and the OHBS.
Bone density testing
Calcaneal ultrasound (QUS-2 Quidel) was utilized to determine calcaneal bone density. Calcaneal ultrasound is as predictive of fracture risk as central dual-energy X-ray absorptiometry of the hip and spine [22]. As an ultrasound wave propagates through a medium, some of its energy is lost, a phenomenon known as attenuation. The attenuation is a function of frequency as determined by comparing the amplitude spectrum obtained through the reference material which is assumed to be nonattenuating (typically degassed water with an added surfactant) with the spectrum obtained through the sample. The QUS-2 test results are reported as broadband ultrasound attenuation (BUA) in units of decibels per megahertz. The BUA value is calculated based on propriety transient analysis algorithms that evaluate the heel’s low-pass filtering characteristics from analysis of the dominant early period. This method produces a very stable BUA value by minimizing the distorting effects of multipath signals [23]. Reference scores of T score below −1.0 are considered abnormal. Peripheral measurement of bone density is predictive of short-term risk of fracture [24].
Determinants of bone mineral density
We assessed demographic characteristics such as age, age at immigration, length of residence in the USA, and osteoporosis knowledge (susceptibility, seriousness, benefits of calcium and exercise, and stage of change) as possible determinants of BMD.
BMD results were provided to participants along with an evaluation for their risk of fractures. Women with abnormal bone density results (T score <−1.0) were recommended to a follow-up with a primary care physician or at the local free clinic.
Analysis
Analysis was conducted with SPSS 16.0. We performed descriptive analysis and categorical variables were analyzed by nonparametric analysis, Wilcoxon, and chi square regarding age, BMD, prior fracture history, stage of change, perceived likelihood of hip or spine fracture, heart attack, stroke, breast cancer, perceived susceptibility and seriousness of osteoporosis, knowledge of and barriers to calcium and exercise, and general health motivation. Multiple linear regression was employed to identify predictors of BMD.
The study protocol was approved by the Office of Protection of Research Subjects at Northwestern University, and all participants provided informed consent. Individuals who were illiterate provided a verbal assent.
Results
A total of 94 women, all Chinese-speaking immigrants, were included in the final analysis. Women were 40–70 years of age with a mean age 59.6 ± 10.3 years. The participants had immigrated from China or Hong Kong. The mean number of years they were living in the USA was 9.6 ± 7.9 years. Surveys were all conducted in Chinese.
The majority of women were Chinese-speaking, 30 (31%) of which were over the age of 65 years and had Medicare coverage. The majority of women (75%) received their medical care at a free clinic in Chinatown. The Chinese Benevolent Association provided information that most women participating in the health fair were Chinese literate, although educational level was not formally assessed.
Osteoporosis health belief
Chinese women identified osteoporosis as a serious condition (p = 0.044) and of high personal susceptibility (p = 0.03). However, they failed to understand the benefits of dietary and supplemental calcium intake (p = 0.339), exercise (p = 0.988), and demonstrated overall low health motivation (p = 0.266). In line with an elevated perceived personal susceptibility, immigrant Chinese women perceived a high likelihood of sustaining a hip (2.37/5) or spine fracture (2.27/5), and comparable to the risk of developing a heart attack (2.35/5) or stroke (2.26/5). They considered that an osteoporosis-related fracture was more likely to occur than breast cancer (1.95/5).
Bone densitometry
The mean BUA was 73.6 ± 16.6 dB/MHz corresponding to a T score of −1.2 ± 1.5.
Determinants of BMD
There was a negative association between age and BMD (Pearson r = −0.451; p < 0.001). Duration of residence in the United States was associated with higher BMD (r = 0.27; p = 0.15). Univariate analysis revealed that 18% of the BMD variance was explained by age (p < 0.001) and 10% by the number of years of residence in the United States (p < 0.001). Multiple regression analysis revealed that younger age and longer length of residence in the USA were associated with higher BMD (p < 0.04). A threshold effect was evident with residence in the USA of 10 years or more resulting in higher BMD than more recent immigrants (p = 0.04) (Fig. 1).
A prior fracture was reported by 16 women (17% of the population). Although women with a prior fracture reported greater perceived seriousness of osteoporosis (p < 0.04), they failed to consider the benefits of calcium supplementation (p = 0.66), were no more aware of their increased risk of spine (p = 0.86) and hip fracture (p = 0.56), and expressed similar health motivation toward osteoporosis (p = 0.26), compared to women without a prior fracture. Fifty-two percent (n = 51) of women reported being in at least in the contemplation stage (stage 3 or 4), which reflects that they were in the process of deciding on whether to have bone density testing or not. There was no association between age or length of US residence and stage of change.
Discussion
Our findings indicate that although immigrant Chinese women in Chicago identified the seriousness of osteoporosis and their personal susceptibility, they had low awareness of the benefit of calcium and exercise and presented low health motivation. Women who had sustained a fracture in the past, a particularly high-risk group for subsequent fractures, failed to understand their increased risk.
Our results contrast to findings from Chinese immigrants in New York where most women understood the benefits of dietary calcium and exercise. In comparison to prior studies on Caucasian women, immigrant Chinese women in Chicago tended to present greater feeling of susceptibility to osteoporosis (19.5 ± 5 vs. 14.5 ± 4.7) and perceived seriousness (18 ± 5 vs. 15.8 ± 5), without an increase in health motivation (21.5 ± 1.2 vs. 20.2 ± 3.1).This apparent disconnect between perceived susceptibility and seriousness and health motivation may be due to a number of factors, one of which may be education [13]. Lauderdale notes that Chinese-Americans in Chicago’s Chinatown are recent immigrants from south China with limited education and resources, with a mean age at immigration of 54 years, and 56% of women have only elementary education or none at all [5].
Another potential explanation may be the lack of osteoporosis health outreach. There may be different public health outreach among Chinese immigrants living in New York and Chicago [3]. In Chicago, there has been no public health outreach or community education about osteoporosis at least in the last 5 years [25]. Our results suggest that these Chinese women are not receiving adequate information about osteoporosis. Therefore, campaigns about osteoporosis should target increasing knowledge about the benefits of calcium and exercise and providing examples of ways that women may better incorporate such elements into their lives. For instance, women could be further encouraged to participate in community-organized Tai Chi programs, which may be a culturally appropriate method of promoting exercise among Chinese immigrant women.
A systematic review of the effects of Tai Chi in postmenopausal women, although limited by the quantity and quality of research to date, suggests that Tai Chi may be an effective, safe, and practical intervention for maintaining BMD in postmenopausal women. Additionally, Tai Chi can positively impact other risk factors associated with low BMD such as reduced fall frequency and increased musculoskeletal strength [26]. In addition, educational programs that encourage periodic osteoporosis screening and increased dietary calcium supplementation may also be helpful. Such education must be culturally appropriate and may be conducted at healthcare provider offices or at local community centers as group education sessions.
The association between greater length of residence in the USA and higher BMD in our cohort supports the notion of nutritional deficits being present in recent Chinese immigrants. It has been reported that BMD of Chinese mainland women was lower than BMD of non-Hispanic blacks, non-Hispanic whites, and Mexican-Americans [27]. The BMD seen in Asian women living in the USA was also lower when compared to Caucasian women. This finding has been attributed to decreased calcium intake, possibly associated with increased lactose intolerance among Asians, and decreased physical activity [28]. In our study, BMD among Chinese immigrant women living in Chicago’s Chinatown was found to be lower than that of Caucasian, Asian-American, and Asian women living in Hong Kong [4, 29]. We hypothesize that, as women do not understand the benefit of dietary calcium or exercise, they are unable to take steps to develop optimal peak bone mass. Other possible causes of low BMD may include low body weight, older age at immigration, poor nutrition in childhood, limited access to medical care, lack of health insurance, language barriers, and distrust of the healthcare system [30–32]. Some of those types of barriers contribute to the health disparities that exist among Asian-American women. Reducing health disparities is a goal of the National Institutes of Health. It is known that African-Americans, Hispanics, Native Americans and Asian/Pacific Islanders account for 25% of the nation’s population, and Asian-Americans are the fastest-growing population. Additionally, Asian-American women have the longest life expectancy than any other ethnic population in the United States. Given the expected growth of Asian-Americans, it remains important to assess the health beliefs in preventive care of osteoporosis [6, 33].
The stages of change model [34] shows that, for most persons, a change in behavior occurs gradually, with the patient moving from being uninterested, unaware or unwilling to make a change (precontemplation), to considering a change (contemplation), to deciding and preparing to make a change. Genuine, determined action is then taken and, over time, attempts to maintain the new behavior occur. Relapses are almost inevitable and become part of the process of working toward life-long change. Chinese immigrant women in this study were found to be in the process of deciding on choosing to have a BMD test (contemplation stage) and receiving treatment (preparation stage). The stages of change model is useful for selecting appropriate interventions. For example, providing women in the precontemplation stage with information about osteoporosis medications is ineffective, as they do not identify with their risk of disease. Therefore, future interventions should focus on discussing Chinese immigrant women about their risk for osteoporosis and fractures and ways to improve their BMD with calcium, exercise, or medications.
Chinese women consider that they are more likely to suffer an osteoporosis-related complication or fracture than a heart attack or breast cancer [21]. This contrasts with prior findings in Caucasian women in whom psychosocial and cancer concerns dominate major health concerns [35]. Some findings about minority populations come from the Commonwealth Fund survey in 1998 that showed that preventive care was lowest among Asian women with less than half of women having received standard preventive care. In addition, minority women do not receive education about health issues that could improve their quality of life or may experience more barriers to following through on health-promoting behaviors. Notably, prior studies have shown that familiarity with osteoporosis has been higher in Caucasian (41%) than in Asian women (17%), and calcium use was again higher in the Caucasian group [36].
Osteoporotic fractures lead to deformity and disability, limitation in activities, suffering, and increased risk for mortality. It has been reported that although women living in mainland China have lower bone mass, the incidence of hip fractures is far lower than in many other races in developed countries and regions [37–40]. Some researchers suggest that shorter hip axis lengths in Asians or differences in geometric shape of bone may be protective [41, 42]. The NORA evaluated Asian-Americans identifying similar fracture rates to Caucasian women [43].
Our study has some limitations which include having a small sample size of Asian women of Chinese origin; thus, findings may not be generalizable to other Asian ethnic subgroups. Our findings may be most applicable to foreign-born Chinese women living in densely concentrated ethnic enclaves such as Chinatown areas. In addition, more health-motivated individuals may have participated in this study as participants were obtained from a local health fair. Our comparison with Caucasian women is limited as Caucasian controls were historical.
Limited data exist on osteoporosis health beliefs among immigrant Chinese women. A better understanding of Chinese immigrant women’s beliefs about osteoporosis will allow health professionals and educators to develop culturally sensitive and targeted messages to promote bone health. Future research in this area and development of culturally specific interventions are needed.
Conclusions
Chinese women immigrants in Chicago exhibit awareness of the seriousness and personal susceptibility to osteoporosis. However, they are unaware of the benefits of calcium and exercise and exhibit low health motivation. Chinese women in Chinatown lack necessary knowledge about osteoporosis to develop adequate self-efficacy. Greater public health initiatives should be undertaken.
References
National Institutes of Health Osteoporosis and Related Bone Disease (2006) Osteoporosis and Asian American women. National Institutes of Health Osteoporosis and Related Bone Disease, Bethesda, MD
Siris E, Miller P, Barrett-Connor E, Faulkner K, Abbott T, Berger M, Santora A, Sherwood L (2001) Identification and fracture outcomes of undiagnosed low bone mineral density in postmenopausal women. JAMA 286:2815–2822
Babbar R, Handa AB, Lo CM, Guttmacher S, Shindledecker R, Chung W, Fong C et al (2006) Bone health of immigrant Chinese women living in New York City. J Community Health 31:7–23
Walker M, Babber R, Opotowsky A, Rohira A, Nabizadeh F, Badia M, Chung W, Chiang J, Mediratta A, McMahon D, Liu G, Bilezikian JP (2006) A referent bone mineral density database for Chinese American women. Osteoporos Int 17:878–887
Lauderdale DS, Kuohung V, Chang SL, Chin MH (2003) Identifying older Chinese immigrants at high risk for osteoporosis. J Gen Intern Med 18:508–515
Office of Minority Health and Health Disparities (2007) Available at http://www.cdc.gov/omhd/Populations/AsianAm/AsianAm.htm. Accessed July 2008
Chang S (2004) Explore the effectors of bone mineral density in community women. J Nurs Res 12:327–335
Haines C, Rong L, Chung T, Leung D (1995) The perception of the menopause and the climacteric among women in Hong Kong and Southern China. Prev Med 24:245–248
Sedlak C, Doheny MO, Estok PJ, Zeller RA, Winchell J (2007) DXA, health beliefs, and osteoporosis prevention behaviors. J Aging Health 18:742–756
Doheny M, Sedlak CA, Estok PJ, Zellar R (2007) Osteoporosis knowledge, health beliefs, and DXA T-scores in men and women 50 years of age and older. Orthop Nurs 26:243–250
Jachna C, Forbes-Thompson S (2005) Osteoporosis: health beliefs and barriers to treatment in an assisted living facility. J Gerontol Nurs 31:24–30
Cline RR, Farley JF, Hansen RA, Schommer JC (2005) Osteoporosis beliefs and antiresorptive medication use. Maturitas 50:196–208
Johnson CS, McLeod W, Kennedy L, McLeod K (2007) Osteoporosis health beliefs among younger and older men and women. Health Educ Behav 35:721–733
Mauck KF, Cuddihy MT, Trousdale RT, Pond GR, Pankratz VS, Melton LJ 3rd (2002) The decision to accept treatment for osteoporosis following hip fracture: exploring the woman’s perspective using a stage-of-change model. Osteoporos Int 13:560–564
Cummings K, Jette AM, Rosenstock IM (1978) Construct validation of the health belief model. Health Educ Monogr 6:394–405
Kim K, Horan ML, Gendler P, Patel MK (1991) Development and evaluation of osteoporosis health belief scale. Res Nurs Health 14:155–163
Hazavehei SM, Taghdisi MH, Saidi M (2007) Application of the health belief model for osteoporosis prevention among middle school girl students, Garmsar, Iran. Educ Health (Abingdon) 20:23
Tussing L, Chapman-Novakofski K (2005) Osteoporosis prevention education: behavior theories and calcium intake. J Am Diet Assoc 105:92–97
Cadarette SM, Beaton DE, Hawker GA (2004) Osteoporosis health belief scale: minor changes were required after telephone administration among women. J Clin Epidemiol 57:154–166
Weinstein ND, Lyon JE, Sandman PM, Cuite CL (1998) Experimental evidence for stages of health behavior change: the precaution adoption process model applied to home radon testing. Health Psychol 17:445–453
Edwards BJ, Ferkel E, Iris M, Feinglass J (2006) Women who suffer a minimal trauma fracture are rarely apprised of the presence of low bone mass or osteoporosis. Maturitas 53:260–266
Prins S, Jørgensen HL, Jørgensen LV, Hassager C (1998) The role of quantitative ultrasound in the assessment of bone: a review. Clin Physiol 18:3–17
Njeh CF, Nicholson PHF, Langton CM (1999) The physics of ultrasound applied to bone. In: Njeh CF (ed) Quantitative ultrasound. Martin Dunitz, London, pp 67–75
Miller P, Siris ES, Barrett-Conner E, Faulkner KG, Wehren LE, Abbott TA, Chen YT et al (2002) Prediction of fracture risk in postmenopausal white women with peripheral bone densitometry: evidence from the National Osteoporosis Risk Assessment. J Bone Miner Res 17:2222–2230
Personal communication from President of Chinese Benevolent Association of Chinatown and Susana Tan, 1 June 2008
Wayne PM, Kiel DP, Krebs DE, Davis RB, Savetsky-German J, Connelly M, Buring JE (2007) The effects of Tai Chi on bone mineral density in postmenopausal women: a systematic review. Arch Phys Med Rehabil 88:673–680
Siris E, Miller P, Barrett-Connor E, Abbott T, Sherwood L, Berger M (1998) Design of NORA, the National Osteoporosis Risk Assessment program: a longitudinal US registry of postmenopausal women. Osteoporos Int 8(Suppl 1):S62–S69
Pothiwala P, Evans EM, Chapman-Novakofski RD (2006) Ethnic variation in risk for osteoporosis among women: a review of biological and behavioral factors. J Womens Health 15:709–719
Lynn H, Lau EMC, Au B, Leung PC (2005) Bone mineral density reference norms for Hong Kong Chinese. Osteoporosis Int 16:1663–1668
Ma G (2000) Barriers to the use of health services by Chinese Americans. J Allied Health 29:64–70
Jang M, Lee E, Woo K (1998) Income, language, citizenship status: factors affecting the health care access and utilization of Chinese Americans. Health Soc Work 23:136–145
Tabora B, Flaskerus JH (1997) Mental health beliefs, practices, and knowledge of Chinese American immigrant women. Issues Ment Health Nurs 18:173–189
National Center on Minority Health Disparities—closing the gap. Available at http://ncmhd.nih.gov/hdFactSheet_gap.asp. Accessed September 2008
Prochaska JO, Velicer WF, Diclemente CC, Fava J (1988) Measuring processes of change: applications to the cessation of smoking. J Consult Clin Psychol 56:520–528
Walters V (1992) Women’s views of their main health problems. Can J Public Health 83:371–374
Collins K, Schoen C, Joseph S, Duchon L, Simantov E, Yellowitz M (1999) Health Concerns across a woman’s lifespan: the Commonwealth Fund 1998 survey of women’s health. Available at http://www.commonwealthfund.org/publications/publications_show.htm?doc_id=221554
Orimo H, Hashimoto T, Sakata K, Yoshimura N, Suzuki T, Hosoi T (2000) Trends in the incidence of hip fracture in Japan, 1987–1997: the third nationwide survey. J Bone Miner Metab 18:126–131
Moayyeri A, Soltani A, Larijani B, Naghavi M, Alaeddini F, Abolhassani F (2006) Epidemiology of hip fracture in Iran: results from the Iranian Multicenter Study on Accidental Injuries. Osteoporos Int 17:1252–1257
Suzuki T (2001) Risk factors for osteoporosis in Asia. J Bone Miner Metab 19:133
Schwartz AV, Kelsey JL, Maggi S, Tuttleman M, Ho SC, Jónsson PV, Poór G, Sisson de Castro JA, Xu L, Matkin CC, Nelson LM, Heyse SP (1999) International variation in the incidence of hip fractures: cross-national project on osteoporosis for the World Health Organization Program for Research on Aging. Osteoporos Int 9:242–253
Cummings SR, Cauley JA, Palermo L, Ross PD, Wasnich RD, Black D, Faulkner KG (1994) Racial differences in hip axis lengths might explain racial differences in rates of hip fracture. Study of Osteoporotic Fractures Research Group. Osteoporos Int 4:226–229
Nakamura T, Turner CH, Yoshikawa T, Slemenda CW, Peacock M, Burr DB, Mizuno Y, Orimo H, Ouchi Y, Johnston CC Jr (1994) Do variations in hip geometry explain differences in hip fracture risk between Japanese and white Americans. J Bone Miner Res 9:1071–1076
Siris ES, Brenneman SK, Miller PD, Barrett-Connor E, Chen YT, Sherwood LM, Abbott TA (2004) Predictive value of low BMD for 1-year fracture outcomes is similar for postmenopausal women ages 50–64 and 65 and older: results from the National Osteoporosis Risk Assessment (NORA). J Bone Miner Res 19:1215–1220
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tan, S., Ji, L., Tsai, J. et al. Greater osteoporosis educational outreach is desirable among Chinese immigrants in Chinatown, Chicago. Osteoporos Int 20, 1517–1522 (2009). https://doi.org/10.1007/s00198-008-0828-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-008-0828-3