Abstract
Summary
The Brazilian Osteoporosis Study (BRAZOS) is the first epidemiological study carried out in a representative sample of Brazilian men and women aged 40 years or older. The prevalence of fragility fractures is about 15.1% in the women and 12.8% in the men. Moreover, advanced age, sedentarism, family history of hip fracture, current smoking, recurrent falls, diabetes mellitus and poor quality of life are the main clinical risk factors associated with fragility fractures.
Introduction
The Brazilian Osteoporosis Study (BRAZOS) is the first epidemiological study carried out in a representative sample of Brazilian men and women aged 40 years or older with the purpose of identifying the prevalence and the main clinical risk factors (CRF) associated with osteoporotic fracture in our population.
Methods
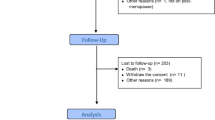
A total of 2,420 individuals (women, 70%) from 150 different cities in the five geographic regions in Brazil, and all different socio-economical classes were selected to participate in the present survey. Anthropometrical data as well as life habits, fracture history, food intake, physical activity, falls and quality of life were determined by individual quantitative interviews. The representative sampling was based on Brazilian National data provided by the 2000 and 2003 census. Low trauma fracture was defined as that resulting of a fall from standing height or less in individuals 50 years or older at specific skeletal sites: forearm, femur, ribs, vertebra and humerus. Sampling error was 2.2% with 95% confidence intervals. Logistic regression analysis models were designed having the fragility fracture as the dependent variable and all other parameters as the independent variable. Significance level was set as p < 0.05.
Results
The average of age, height and weight for men and women were 58.4 ± 12.8 and 60.1 ± 13.7 years, 1.67 ± 0.08 and 1.56 ± 0.07 m and 73.3 ± 14.7 and 64.7 ± 13.7 kg, respectively. About 15.1% of the women and 12.8% of the men reported fragility fractures. In the women, the main CRF associated with fractures were advanced age (OR = 1.6; 95% CI 1.06–2.4), family history of hip fracture (OR = 1.7; 95% CI 1.1–2.8), early menopause (OR = 1.7; 95% CI 1.02–2.9), sedentary lifestyle (OR = 1.6; 95% CI 1.02–2.7), poor quality of life (OR = 1.9; 95% CI 1.2–2.9), higher intake of phosphorus (OR = 1.9; 95% CI 1.2–2.9), diabetes mellitus (OR = 2.8; 95% CI 1.01–8.2), use of benzodiazepine drugs (OR = 2.0; 95% CI 1.1–3.6) and recurrent falls (OR = 2.4; 95% CI 1.2–5.0). In the men, the main CRF were poor quality of life (OR = 3.2; 95% CI 1.7–6.1), current smoking (OR = 3.5; 95% CI 1.28–9.77), diabetes mellitus (OR = 4.2; 95% CI 1.27–13.7) and sedentary lifestyle (OR = 6.3; 95% CI 1.1–36.1).
Conclusion
Our findings suggest that CRF may contribute as an important tool to identify men and women with higher risk of osteoporotic fractures and that interventions aiming at specific risk factors (quit smoking, regular physical activity, prevention of falls) may help to manage patients to reduce their risk of fracture.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fragility fractures are a significant public health problem in the entire world. The incidence of osteoporosis-related fractures, especially hip fractures, increases with age and are associated with significant reductions in quality of life and high mortality. The mortality rate stemming from hip fractures in developed countries is about 25% in the first 12 months following the event [1–2]. Higher mortality rates for hip fractures have been reported in the Brazilian population (21% to 30%) [3–4]. A significant association between low bone mass and higher overall and cardiovascular mortality has been found among elderly Brazilian women, regardless of age and the presence of co-morbidities [5]. The age-adjusted annual incidence of hip fractures in the Brazilian population ranges from 5.59 to 13 and 12.4 to 27.7 per 10,000 inhabitants for men and women, respectively [6–8]. Racial, genetic, anthropometrical, socio-cultural, economic and nutritional differences contribute toward the divergences in the incidence and prevalence of fractures and the use of public health resources in different countries [1, 2].
A number of clinical risk factors (CRF) for low bone mass and fractures have been identified. No one risk factor alone is able to predict bone mass or the risk of fractures on an individual basis. Osteoporosis is a multi-factor disorder, which is 70% dependent upon genetic factors and 30% dependent upon environmental factors [2, 9]. Nonetheless, the early identification of individuals at risk using clinical risk factors is fundamental to the implementation of effective strategies for the prevention, diagnosis and treatment of osteoporosis [9]. The use of CRF to identify patients at risk for osteoporosis has the potential of allowing the modification of living habits and may also be used to enhance the performance of clinical densitometry in identifying patients at a high risk for fractures. The clear advantages of using such risk factors on populations are the low cost and easy execution, especially in developing countries where healthcare resources are scarce.
A number of population-based studies in Europe, the United States and Asia have confirmed the importance of clinical risk factors as determinants for fragility fractures [10–13] and low bone mass [14–17]. The sensitivity and specificity of such instruments in identifying individuals, especially post-menopausal Caucasian women, with low bone mass or fractures is about 75–95% and 35–60%, respectively [10–17]. Nevertheless, none of these studies evaluated the performance of CRF in identifying fractures among men, pre-menopausal women and non-Caucasian populations.
A number of clinical risk factors for fractures (previous fracture, old age, low weight, use of glucocorticoids, current smoking habit and family history of hip fracture) play a significant role as determinants for osteoporotic fractures. In recent years, a number of studies have evaluated the performance of combined approaches (bone mass measurements and CRF) for determining the absolute risk of fractures, identify patients at the highest risk and clear implications on the direct and indirect costs associated with the management of the osteoporosis [18].
There have been few data on the prevalence and relevance of CRF for fractures in the Latin America population and in Brazil specifically. The aim of the present study was to identify the prevalence and main clinical risk factors associated with fragility fractures in a representative sample of the Brazilian population aged 40 years or older.
Methods
A total of 2420 individuals (725 men and 1695 women) aged 40 years or older were evaluated through a quantitative cross-sectional survey. The participants included in the study were from all socioeconomic classes, educational levels and different occupations. The survey was conducted through face-to-face interviews at the participant’s home administered by a trained, specialized team. Individuals from 150 cities (under 20,000 inhabitants; 20,000 to 100,000 inhabitants; over 100,000 inhabitants) throughout Brazil were surveyed. Household income was calculated based on its relation to the monthly minimum wage.
Brazil has continental dimensions, with 8,514,215.3 km2, and consists of 27 confederated units, with a total of 5,507 cities. At the time of the last census, the population consisted of about 169,799,170 inhabitants (86,223,155 women), most from a mixed ethnic background. Officially, the population consists of the following ethnic groups: white (53.8%), mixed race (50.2%), African descent (6.2%), Asian descent (0.45%) and Native Brazilian indigenous (0.43%). Most of the Brazilian population lives in urban areas (81.2%) [19].
The sample size for the present study was calculated by probabilistic sampling in order to represent both the urban and rural Brazilian population as reported by the 2000 Brazilian National Census (IBGE, Brazilian Institute of Geography and Statistics) [19] and the 2003 National Survey of Domicile Sampling (PNAD 2003) [20]. The sample was selected in three phases, with control of gender, age and occupation; homes were randomly selected. Interviews were performed on weekdays and weekends both day and night, in order to maximize the possibility of encountering the target population at home. Mean time for administering the questionnaire was 60 minutes for each individual. Distortions regarding gender and age were purposely performed in order mainly to include women and individuals 65 years old or older, which is the population most at risk for osteoporosis. Sample distribution according to social class, education, marital status, ethnic group and geographic region mimicked official data for the Brazilian population. The data were further weighted with respect to the distribution and proportionality of the overall Brazilian population. The sampling error was 2.2%, with 95% confidence intervals.
Individuals with cognitive deficiencies that could hinder consistent responses to the questionnaire (such as neurological diseases or senile dementia) were excluded from the study. Homes with more than two individuals aged 40 years or older were also excluded form the survey.
A structured questionnaire was especially designed for the present study based on a literature review [9–18]. The main parameters evaluated were age, demographic, anthropometric and socioeconomic data, general knowledge of osteoporosis, previous falls and circumstances of falls in the previous year, medical history, previous fractures, gynecological and reproductive history, family history of hip fracture after 50 years of age in first-degree relatives, quality of life (SF-8) [21], medication use and co-morbidities, classified according to the International Classification of Diseases, 10th revision.
The food frequency questionnaire was based on a 24-hour diet recall. The interviewers were trained by a nutritionist specialized in food frequency questionnaires for nutritional evaluation. Current and past habits as smoking, alcohol consumption, exposure to sunlight and physical activity [22] were also determined in all individuals.
Fragility or low-impact fracture was defined as that associated with a fall from standing height or less after 50 years of age. Skeletal sites for fragility fractures were axial (ribs, lumbar and thoracic vertebrae) and peripheral bones (forearm, humerus and femur). Traumatic fractures and those occurring at sites not characteristic of bone fragility (face, skull, tibia, fibula and femoral diaphysis) were excluded from the analysis. Individuals experiencing two or more falls in the previous 12 months were defined as chronic fallers [23].
All questionnaires were reviewed by an independent supervisor and underwent a continuous process of critical examination and consistency assessments. Inconsistently filled out questionnaires were returned for correction. About 25% of the questionnaires were verified either in loco or post hoc through phone calls.
All participants gave written informed consent prior to participation in the study and the research ethics committee of the Universidade Federal de São Paulo/Escola Paulista de Medicina approved the protocol.
Anthropometrical data were measured, with all participants wearing light clothing and no shoes. Weight (m) and height (kg) were measured using a portable anthropometric scale (Filizola®). Body mass index (BMI) was calculated as kg/m2.
Statistical analysis
Data are presented as mean and standard deviation (SD). The Student’s T-test was used to compare variables. The chi-square test was employed to determine correlations between continuous and categorical variables. Category construction was based on the distribution of tertiles of frequency of the sample for all continuous variables. BMI categories were very similar to the World Health Organization (WHO) classification criteria for obesity. Logistic regression analysis models were designed, with low-impact fracture as the dependent variable and all other parameters as independent variables.
The SPSS/PC for Windows version 12 and SAS (Statistical Analysis System) for Windows, version 8.02, were used for all statistical analyses. The level of significance was set as p < 0.05.
Results
Tables 1 and 2 display the anthropometrical and demographic data for the study population (individuals over 40 years of age).
As demonstrated in Table 3, most of the population was classified as overweight or obese (60% of men and 59% of women), especially among socioeconomic classes A and B [Brazilian Socioeconomic Classification from A (highest level of income) to E (lowest level of income)]. The prevalence of overweight and obesity did not differ significantly between the different geographic regions for both men and women. There were also no significant differences between geographic regions in terms of age, weight, height, BMI and socioeconomic class distribution of the population (data not shown).
The most frequently reported diseases were hypertension (29%), lower back pain (18%), arthritis (14%), dyspepsia (13%), depression (11%), diabetes mellitus (8%), dyslipidemia (6%) and osteoporosis (6%). About 33% of the population reported no diseases. All reported co-morbidities were more common among women, except for dyspepsia and diabetes mellitus, which had similar frequencies between men and women.
Mean age for first menstruation and menopause were 13 ± 1.8 and 47 ± 5.1 years, respectively. About 35% of the women were pre-menopausal. Prolonged use of glucocorticoids was found in 4% of the individuals. Nearly 25% of the sample was using medication known to affect bone metabolism, such as hormone replacement therapy (HRT) (15%) and bisphosphonates (4%). There were no statistically significant differences in terms of gender, social class, age and geographic region for these parameters.
Only 24% of the individuals exercised regularly in the previous 12 months. Physical activity was significantly more prevalent among social classes A and B and among individuals from the southern and southeastern region regions (30%) (p < 0.05). About 25% of the individuals were current smokers; the prevalence of smoking was higher among men than women (28% versus 21%). Nearly half of the men (47%) reported regular alcohol consumption in the previous year, especially among individuals from socioeconomic classes A and B. Most of the women (53%) reported no regular use of alcoholic beverages. Regular alcohol consumption in the previous year was reported by 41% of the men (11% daily ingestion and 30% weekend use) and 18% of the women (3% daily and 15% on weekends).
About 15.1% of the women and 12.8% of the men reported fragility fractures. Anthropometrical data for the population with fractures are shown in Table 4. Women with fractures were significantly older than those without, while men with fractures had significantly low weight than those without. The mean age at first menstruation for women with fractures was significantly higher than those without fractures. Women with fractures had shorter menacme period and greater number of children (data not shown).
Smoking was significantly more prevalent among men with fractures than those without (18.4 ± 0.78 versus 6.19 ± 2.26 pack/years, respectively). No significant difference in smoking habit was found between women with and without fractures (7.86 ± 0.42 versus 7.14 ± 1.62 pack years, respectively).
Men and women with fractures reported significantly less physical activities than those without (16.9 versus 44.8% and 8.1 versus 32.7% for men and women, respectively). Family history of hip fracture was more prevalent among women with fractures than those without (14.5 versus 7.1%, respectively; p = 0.037); this correlation was not observed among men. Previous use of contraception pills was significantly more prevalent among women without fractures than those with fractures (50.1 versus 33.9%, respectively; p = 0.009), while oophorectomy and early menopause were more prevalent among women with fractures than those without (20.4 vs. 8.2%, respectively; p = 0.02). Current use of glucocorticoids, sunlight exposure and alcohol use did not differ significantly between men and women with and without fractures. HRT, hysterectomy and amenorrhea did not differ between women with and without fractures (data not shown).
The main fracture sites were distal forearm (30%), femur (12%), humerus (8%), ribs (6%) and vertebrae (4%). No significant difference in the presence of fracture was found between the five geographic regions, according to gender and socioeconomic class. However, fractures were more prevalent in women living in metropolitan areas than those living in smaller communities. There was a trend for higher prevalence of fractures among men in the northeastern region as compared to other geographic regions (Table 5).
For the women in the present study, univariate analyses demonstrated that fragility fracture was associated with age (65 years old and over), Caucasian ethnic background, marital status (widowed), early menopause, bilateral oophorectomy prior to menopause, multiparity, family history of hip fracture, poor quality of life, higher phosphorus and protein intake and lower calcium intake (all adjusted for energy), recurrent falls, presence of co-morbidities (depression, diabetes mellitus, osteoporosis, osteoarthritis and urolithiasis) and current medication use (calcium channel blockers, insulin, benzodiazepine compounds, anti-vertigo drugs) (data not shown). After adjustments for potential confounders, the CRF significantly associated with fracture were identified and are displayed in Table 6. The model demonstrated excellent adjustment by the Hosmer–Lemeshow method (p = 0.513). There was a tendency toward a greater risk of fractures in women having more than 20 cigarettes per day and in multiparas (p = 0.06). Anti-diabetes drugs (sulfonylureas and biguanides) and insulin also tended toward an association to low-impact fracture, but this association was lost when adjusted for the presence of diabetes mellitus. Similarly, the use of anti-vertigo drugs was initially associated with fractures, but the association lost significance when corrected by number of falls in the previous year. Weight, BMI, age at first menstruation and menopause as well as current HRT and alcohol use were not significantly associated with fractures in the multivariate model.
In men, the presence of fragility fractures was significantly associated with working conditions (unemployed/retired), poor quality of life, family history of hip fracture, higher consumption of protein, co-morbidities (depression, chronic anemia, gastritis and rheumatoid arthritis) and current use of medications (oral anti-diabetes and neuroleptics) in the univariate model (data not shown). After adjustments for potential confounders, CRF for fractures in men were identified and are displayed in Table 7. The model demonstrated excellent agreement (p = 0.93). Demographic and anthropometric variables and alcoholism did not correlate with the presence of fractures.
Discussion
The BRAZOS is the first epidemiological study designed to identify the main CRF associated with fragility fracture in a representative sample of the Brazilian adult population. Prior to this study, the incidence and the major CRF for osteoporotic fractures in both men and women were unknown in Brazil and estimated from international studies.
Our results demonstrate that a sedentary lifestyle, current smoking habits, poor quality of life and diabetes mellitus are the most relevant CRF for fragility fractures in Brazilian men. Among women, the most important factors are advanced age, early menopause, sedentary lifestyle, poor quality of life, higher phosphorus intake, diabetes mellitus, recurrent falls, chronic use of benzodiazepine drugs and family history of hip fracture. These factors reflect the involvement of several structural aspects in the determination of a greater risk of fractures, such as genetic disposition (family history of hip fracture), living habits (physical activity, smoking and eating habits), quality of life, falls and the aging process itself, leading to the deterioration of bone quality.
Although the CRF in populations at high risk for osteoporosis and fractures are quite well established, especially in international studies, their prevalence in the general population is still not clearly defined. In the BRAZOS study, we evaluated the risk of fractures in individuals with and without associated diseases and with and without the presence of concomitant medications, characterizing a general population—“real life” scenario—and not only individuals at the highest risk for osteoporosis.
In Brazil, a number of retrospective or cross-sectional studies with poorly representative samples have found several risk factors for low bone mass, such as a lack of estrogen, menopause, low exposure to sunlight, alcoholism, low calcium intake, sedentary lifestyle, family history of osteoporosis, smoking habits, low weight, low stature, advanced age, lower levels of schooling, late first menstruation, early menopause and low BMI [5, 24, 25]. The BRAZOS study did not evaluate factors associated with low bone mass, but one may expect that risk factors for low bone mass are similar to those associated with fragility fractures. Ramalho et al. reported that the main risk factors associated with hip fracture in the elderly were low BMI, sedentary lifestyle and greater number of gestations [25]. Evaluating 275 post-menopausal women, Pinheiro et al. [26] demonstrated that the major risk factors associated with osteoporotic fractures were a low score on the stiffness index and femoral neck BMD, family history of hip fracture, advanced age and low weight. The authors also demonstrated that the combination of CRF with BMD measurements may improve the identification of patients at a greater risk for fractures.
In a recent study including 3,214 individuals from Pelotas-RS (southern region of Brazil), Siqueira et al. [27] found that the risk factors associated with fragility fractures were prior history of osteoporosis, falls in the previous year, male gender, Caucasian or mixed ethnic background and lower level of schooling. The prevalence of fractures throughout life reported in the study was nearly twice as high (28.3%) as that reported in the BRAZOS study. In the Siqueira et al. study, the prevalence of fractures throughout life was 37.5% for men, principally resulting from the practice of sports and leisure activities outside the home, and 21.3% for women, especially resulting from falls inside the home (p < 0.001). Interestingly, men had a 50% greater risk of fractures than women in the previous 12 months (p = 0.09). In the BRAZOS study, we found a significantly higher prevalence of fractures among women (15.1%) than men (12.8%), which corroborates previous studies (1–8). The study in the southern region of the country included more young individuals (20 years old and over) than the present study as well as both traumatic and non-traumatic fractures. These aspects may have contributed toward the higher prevalence of fractures in men in the study.
Results from the BRAZOS study are in agreement with a previous study by Albrand et al. [28], who identified the following main risk factors for fractures in 672 post-menopausal women: age above 65 years old, falls, low femur BMD, low grip strength, maternal history of fractures, sedentary lifestyle and previous fractures. Weight, loss of height, loss of weight, smoking habits and HRT were not associated with fragility fractures in the final model.
Low weight is considered an important risk factor for low bone mass [1, 2, 11, 15–17] and fractures [12–13], principally in populations at the highest risk for osteoporosis. In our study, however, we were unable to demonstrate any significant association between anthropometric parameters and fractures in either gender, although we took care to measure and weigh all individuals accurately. We believe that the high number of younger individuals in our sample (34% were between 40 and 50 years old), associated with the high prevalence of overweight and obesity, may explain our findings regarding the correlation between body size and bone fragility. In an American population-based study, Taylor et al. [29] also found no significant impact of body weight on the risk of hip fracture among 6787 elderly women. Likewise, Robbins et al. [30], evaluating other large epidemiological studies (WHI—Women’s Health Initiative; CHS—the Cardiovascular Health Study; EPIDOS—EPIDemiologie de l’OSteoporose), also found no predictive value of BMI regarding bone density, although they did not study its impact on fracture frequency.
A number of studies demonstrate that the eating habits of western women, characterized by high phosphorus intake and low calcium consumption, may lead to an increased risk of osteoporosis. Low calcium consumption has been emphasized by a number of national studies on women [31] and adolescents [32]. In the present study, calcium intake was indeed lower (daily national average of 400 mg) than that previously reported (600–800 mg/ day). In women, there was a tendency toward a greater risk of fractures in those with daily calcium intake lower than 300 mg. Low vitamin D intake was noted in all social classes and regions of the country in both men and women alike. This corroborates the finding of an increased prevalence of hypovitaminosis D (deficiency in 15.4% and insufficiency in 41.9% of the patients) recently demonstrated among the elderly living in the city of Sao Paulo [33]. These findings may be connected with the greater risk of osteoporotic fractures in our population.
The imbalance of calcium and phosphorus intake has become more pronounced with the recent modifications of preferences in the diet and the growing use of food additives containing phosphorus. The elevated consumption of phosphorus and reduced calcium intake can cause a persistent increase of PTH as well as compromise renal production and the serum concentration of calcitriol. The resultant secondary hyperparathyroidism leads to bone loss in animal models. In humans, the potential harmful role of increased ingestion of foods rich in phosphorus has not yet been well established [34]. The BRAZOS study is the first population-based study to demonstrate the negative role of high dietary intake of phosphorus in the risk of fragility fractures. Thus, the low calcium and vitamin D intake associated with the elevated consumption of phosphorus, a sedentary lifestyle, recurrent falls and smoking habits can contribute toward the greater risk of fracture in our population.
Our findings indicate that diabetes mellitus (DM) is associated with a greater risk of fragility fractures in both men and women alike. Studies on the impact of DM on skeletal health are controversial, as the disease affects bone tissue through different mechanisms. Modifications in the levels of insulin and IGF-1, the accumulation of glycation end products, a reduction in renal function, obesity, hypercalciuria associated with glycosuria, lower intestinal absorption of calcium, inappropriate homeostatic response to PTH secretion, complex modifications in the regulation of vitamin D, angiopathy, inflammation and neuropathy have all been described as potential factors influencing bone status in diabetic patients. Type I DM is associated with a reduction in BMD and a greater risk of osteoporotic fracture [35], whereas Type II DM has been associated with higher bone mass and greater risk of fragility fractures, especially non-vertebral fractures. It seems that bone quality and remodeling play a special role in determining the risk of fractures in these patients, along with other extra-skeletal factors, such as the risk of falls associated with neuropathic and microangiopathic complications [36].
Postural hypotension and dizziness are frequent complaints among elderly individuals and are related to prolonged immobilization as well as a greater risk of falls and fractures [37]. Recent meta-analysis to determine the risk of fractures in users of psychotropic drugs showed that benzodiazepine, antidepressants, non-barbiturate anticonvulsants, barbiturate anticonvulsants, anti-psychotic, hypnotics and opioids are all associated with greater risk of fracture [38]. In the BRAZOS study, only the current use of benzodiazepine drugs was associated with greater risk of fractures in adult women.
Studies on Brazilian men over 50 years of age [39–40] have found a positive and significant correlation between BMD and current and past practice of physical exercise, even after adjustments for age and BMI. In these studies, the main CRF for low BMD were BMI, current physical activity, age, smoking habits, Caucasian race, maternal history of fracture and no current use of thiazides.
A prospective cohort of 5,995 old men found a high prevalence of smoking habits (59%) and consumption of alcoholic beverages (47%), with average BMI similar to that of the present study (26.9 kg/m2). In the cohort, there were more reports of fractures (17%) than that seen in the BRAZOS study (12.8%). The main risk factors for fragility fractures were use of antidepressant drugs, previous fracture, number of falls in the previous year, age above 80 years, depressed mood and lower bone density in the hip [41]. In the BRAZOS study, we found that a sedentary lifestyle and current smoking habits were significantly associated with a greater risk of fractures in women and men alike, suggesting that the encouragement of physical exercise and to stop smoking should be considered as a simple relevant measure for the prevention of fractures in our population.
Genetic aspects importantly influence the acquisition of peak bone mass, bone loss associated with aging, hormonal factors and fragility fractures. The Brazilian population is characterized by a high degree of interbreeding and no national study has managed to demonstrate a robust, significant association between genetic polymorphism [vitamin D receptor—VDR [42] and COL1A1 [43] and BMD. In the BRAZOS study, a family history of hip fracture after 50 years of age in first degree relatives was significantly associated with a greater risk of fractures in women, which corroborates reports by other authors [10, 11, 26].
Osteoporotic fractures are associated with a significant reduction in quality of life [44]. In the present study, a strong association was observed between worse quality of life and the presence of fractures in both men and women alike. Patients with osteoporosis and fractures have significantly more chronic pain, reduced physical capacity and social activities, lower perception of wellbeing and a more depressed mood than individuals without fractures. However, no significant association was found between fractures and mental aspects, as seen with other questionnaires [44, 45]. Normative data are of special interest in determining whether group or individual scores are below or above the expected average, considering the peculiarities of country, gender and age group. A number of countries have published normative data on quality of life, but there are none yet in Brazil.
Some limitations of our study need to be pointed out. First of all, radiographic examination of the spine was not performed. Thus, highly prevalent non-symptomatic vertebral fractures cannot be ruled out. The prevalence of some co-morbidities may be underestimated, as they were only reported by the participants and no clinical (blood pressure, etc.) or lab tests (fasting glucose, cholesterol, etc.) were performed. Although laboratory analyses were not performed, it should be noted that a detailed clinical evaluation was carried out in order to exclude potential secondary causes of osteoporosis. The fact that some aspects of the survey were based on the memory of individuals and recall capacity is another limitation of the present study.
The actual prevalence of osteoporosis in the Brazilian population is probably higher than that reported here (6%). We believe that by using bone densitometry we would be able to identify a significantly higher prevalence of osteoporosis in our population. Moreover, considering the high prevalence of fragility fractures in our population associated with the concept of osteoporosis according to the WHO [46], we could say that at least 12.8% of the men and 15.1% of the women 40 years of age or older living in Brazil have osteoporosis.
The present survey helps identify Brazilian adult individuals with a greater risk of fragility fractures and improve the effectiveness of measures for the promotion of bone health and prevention of bone disease. Through a simple, quick clinical evaluation, the identification of the CRF associated with fractures in the present study may help select individuals for bone densitometry or distinguish individuals at high risk of fractures from those at low risk.
Currently, the clinical decision for therapeutic intervention in patients with osteoporosis or increased risk of fragility fractures is based on the evaluation of risk factors and bone mass measurements. BMD parameters have been regularly used to guide therapeutic intervention (T-score lower than – 2.5), while the use of CRF is still not standardized as a routine in therapeutic decisions. It is interesting to note densitometric criteria was developed to identify patients with a greater risk of fractures and not to guide therapeutic intervention. More recently, there has been a tendency toward a more individualized evaluation of the risk of fracture – absolute risk of fracture – with the combination of CRF and bone densitometry. This strategy seems to be more suitable for the decision-making process than using BMD measurements alone.
Our results demonstrate that clinical risk factors for fragility fractures are very important and should be included in routine medical practice in order to determine the risk of fractures and, probably, to calculate the absolute risk of fractures in our population.
References
Kanis JA, Oden A, Johnell O, Jonsson B, de Laet C, Dawson A (2001) The burden of osteoporotic fractures: a method for setting intervention thresholds. Osteoporos Int 12(5):417–427
Johnell O, Kanis J (2005) Epidemiology of osteoporotic fractures. Osteoporos Int 16(Suppl 2):S3–S7
Garcia R, Leme MD, Garcez-Leme LE (2006) Evolution of Brazilian elderly with hip fracture secondary to a fall. Clinics 61(6):539–544
Vidal EI, Coeli CM, Pinheiro RS, Camargo KR (2006) Mortality within 1 year after hip fracture surgical repair in the elderly according to postoperative period: a probabilistic record linkage study in Brazil. Osteoporos Int 17(10):1569–1576
Pinheiro MM, Castro CM, Szejnfeld VL (2006) Low femoral bone mineral density and quantitative ultrasound are risk factors for new osteoporotic fracture and total and cardiovascular mortality: a 5-year population-based study of brazilian elderly women. J Gerontol A Biol Sci Med Sci 61(2):196–203
Castro da Rocha FA, Ribeiro AR (2003) Low incidence of hip fractures in an equatorial area. Osteoporos Int 14(6):496–499
Silveira VA, Medeiros, Coelho-Filho JM et al (2005) Hip fracture incidence in an urban area in Northeast Brazil. Cad Saude Publica 21(3):907–912
Komatsu RS, Ramos LR, Szejnfeld VL (2004) Incidence of proximal femur fractures in Marilia, Brazil. J Nutr Health Aging 8(5):362–367
Abrahamsen B, Rejnmark L, Nielsen SP et al (2006) Ten-year prediction of osteoporosis from baseline bone mineral density: development of prognostic thresholds in healthy postmenopausal women. The Danish Osteoporosis Prevention Study. Osteoporos Int 17(2):245–251
Black DM, Steinbuch M, Palermo L et al (2001) As assessment tool for predicting fracture risk in postmenopausal women. Osteoporos Int 12:519–528
Siris ES, Miller PD, Barrett-Connor E et al (2001) Identification and fracture outcomes of undiagnosed low bone mineral density in postmenopausal women: results from the National Osteoporosis Risk Assessment. JAMA 286(22):2815–2822
Dargent-Molina P, Douchin MN, Cormier C, Meunier PJ, Breart G, and EPIDOS Study Group (2002) Use of clinical risk factors in elderly women with low bone mineral density to identify women at higher risk of hip fracture: The EPIDOS prospective study. Osteoporos Int 13(7):593–599
Henry MJ, Pasco JA, Sanders KM, Nicholson GC, Kotowicz MA (2006) Fracture Risk (FRISK) Score: Geelong Osteoporosis Study. Radiology 241(1):190–196
Black DM, Palermo L, Pearson J, Abbott T, Johnell O (1998) A simple, useful risk factor system can identify the large majority of women with osteoporosis. Bone 23(Suppl 5):605
Cadarette SM, Jaglal SB, Kreiger N, McIsaac WJ, Darlington GA, Tu JV (2000) Development and validation of the Osteoporosis Risk Assessment Instrument to facilitate selection of women for bone densitometry. CMAJ 162(9):1289–1294
Koh LK, Sedrine WB, Torralba TP et al (2001) Osteoporosis Self-Assessment Tool for Asians (OSTA) Research Group. A simple tool to identify Asian women at increased risk of osteoporosis. Osteoporos Int 12(8):699–705
Sen SS, Rives VP, Messina OD et al (2005) A risk assessment tool (OsteoRisk) for identifying Latin American women with osteoporosis. J Gen Intern Med 20(3):245–250
Kanis JA, Oden A, Johnell O, Johansson H et al (2007) The use of clinical risk factors enhances the performance of BMD in the prediction of hip and osteoporotic fractures in men and women. Osteoporos Int 18(8):1033–1046
Instituto Brasileiro de Geografia e Estatística 2000. http://www.ibge.gov.br/home/estatistica/populacao/censo2000/default.shtm
Pesquisa Nacional por Amostras de Domicílios 2003. http://www.ibge.gov.br/home/estatistica/populacao/trabalhoererendimento/pnad2003/coeficiente_brasil.shtm
Ware JE, Kosinski M, Dewey JE et al (2001) How to score and interpret single-item health status measures: a manual for users of the SF-8 Health Survey. Lincoln RI: Quality Metric Incorporated
Florindo AA, Latorre M do R, Jaime PC, Tanaka T, Zerbini CA (2004) Methodology to evaluation the habitual physical activity in men aged 50 years or more. Rev Saude Publica 38(2):307–314
Schwartz AV, Villa ML, Prill M et al (1999) Falls in older mexican-American women. J Am Geriatr Soc 47(11):1371–1378
Rodrigues Camargo MB, Cendoroglo MS, Ramos LR et al (2005) Bone mineral density and osteoporosis among a predominantly Caucasian elderly population in the city of Sao Paulo, Brazil. Osteoporos Int 16(11):1451–1460
Ramalho AC, Lazaretti-Castro M, Hauache O, Vieira JG, Takata E, Cafalli F, Tavares F (2001) Osteoporotic fractures of proximal femur: clinical and epidemiological features in a population of the city of Sao Paulo. Sao Paulo Med J 119(2):48–53
Pinheiro MM, Castro CH, Frisoli A, Szejnfeld VL (2003) Discriminatory ability of quantitative ultrasound measurements is similar to dual-energy X-ray absorptiometry in a Brazilian women population with osteoporotic fracture. Calcif Tissue Int 73(6):555–564
Siqueira FV, Facchini LA, Hallal PC (2005) The burden of fractures in Brazil: a population-based study. Bone 37(2):261–266
Albrand G, Munoz F, Sornay-Rendu E, DuBoeuf F, Delmas PD (2003) Independent predictors of all osteoporosis-related fractures in healthy postmenopausal women: the OFELY study. Bone 32(1):78–85
Taylor BC, Schreiner PJ, Stone KL et al (2004) Long-term prediction of incident hip fracture risk in elderly white women: Study of Osteoporotic Fractures. J Am Geriatr Soc 52(9):1479–1486
Robbins J, Schott AM, Azari R, Kronmal R (2006) Body mass index is not a good predictor of bone density: results from WHI, CHS, and EPIDOS. J Clin Densitom 9(3):329–334
Montilla RNG, Aldrighi JM, Marucci MFN (2004) Calcium/protein relation of women on the climacteric. Rev Assoc Med Bras 50(1):52–54
Lerner BR, Lei DLM, Chaves SP et al (2000) Consumption of calcium by adolescents from public schools em Osasco, São Paulo, Brazil. Rev Nutr 13(1):57–63
Saraiva GL, Cendoroglo MS, Ramos LR et al (2005) Influence of ultraviolet radiation on the production of 25 hydroxyvitamin D in the elderly population in the city of Sao Paulo (23 o 34¢S), Brazil. Osteoporos Int 16(12):1649–1654
Heaney RP (2001) Constructive interactions among nutrients and bone-active pharmacologic agents with principal emphasis on calcium, phosphorus, vitamin D and protein. J Am Coll Nutr 20(5 Suppl):403S–409S
Miao J, Brismar K, Nyren O, Ugarph-Morawski A, Ye W (2005) Elevated hip fracture risk in type 1 diabetic patients: a population-based cohort study in Sweden. Diabetes Care 28(12):2850–2855
Carnevale V, Romagnoli E, D’Erasmo E (2004) Skeletal involvement in patients with diabetes mellitus. Diabetes Metab Res Rev 20(3):196–204
Pluijm SM, Smit JH, Tromp EA, Stel VS, Deeg DJ, Bouter LM, Lips P (2006) A risk profile for identifying community-dwelling elderly with a high risk of recurrent falling: results of a 3-year prospective study. Osteoporos Int 17(3):417–425
Takkouche B, Montes-Martinez A, Gill SS, Etminan M (2007) Psychotropic medications and the risk of fracture: a meta-analysis. Drug Saf 30(2):171–184
Florindo AA, Latorre M do R, Jaime PC, Tanaka T, Pippa MG, Zerbini CA (2002) Past and present habitual physical activity and its relationship with bone mineral density in men aged 50 years and older in Brazil. J Gerontol A Biol Sci Med Sci 57(10):M654–M657
Tanaka T, Latorre MR, Jaime PC, Florindo AA, Pippa MG, Zerbini CA (2001) Risk factors for proximal femur osteoporosis in men aged 50 years or older. Osteoporos Int 12(11):942–949
Lewis CE, Ewing SK, Taylor BC, Shikany JM, Fink HA, Ensrud KE, Barrett-Connor E, Cummings SR, Orwoll E and Osteoporotic Fractures in Men (MrOS) Study Research Group (2007) Predictors of non-spine fracture in elderly men: the MrOS study. J Bone Miner Res 22(2):211–219
Lazaretti-Castro M, Duarte-de-Oliveira MA, Russo EM, Vieira JG (1997) Vitamin D receptor alleles and bone mineral density in a normal premenopausal Brazilian female population. Braz J Med Biol Res 30(8):929–932
Barros ER, Kasamatsu TS, Ramalho AC, Hauache OM, Vieira JG, Lazaretti-Castro M (2002) Bone mineral density in young women of the city of Sao Paulo, Brazil: correlation with both collagen type I alpha 1 gene polymorphism and clinical aspects. Braz J Med Biol Res 35(8):885–893
Brenneman SK, Barrett-Connor E, Sajjan S, Markson LE, Siris ES (2006) Impact of recent fracture on health-related quality of life in postmenopausal women. J Bone Miner Res 21(6):809–816
Fechtenbaum J, Cropet C, Kolta S, Horlait S, Orcel P, Roux C (2005) The severity of vertebral fractures and health-related quality of life in osteoporotic postmenopausal women. Osteoporos Int 16(12):2175–2179
Kanis JA (1994) Assessment of fracture risk and its appication to screening for postmenopausal osteoporosis: synopsis of a WHO report. WHO Study Group. Osteoporos Int 4(6):368–381
Acknowledgements
This study was funded by a grant from Wyeth Healthcare Consumer.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pinheiro, M.M., Ciconelli, R.M., Martini, L.A. et al. Clinical risk factors for osteoporotic fractures in Brazilian women and men: the Brazilian Osteoporosis Study (BRAZOS). Osteoporos Int 20, 399–408 (2009). https://doi.org/10.1007/s00198-008-0680-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-008-0680-5