Abstract
Summary
In 242 community-dwelling seniors, supplementation with either 1000 mg of calcium or 1000 mg of calcium plus vitamin D resulted in a decrease in the number of subjects with first falls of 27% at month 12 and 39% at month 20. Additionally, parameters of muscle function improved significantly.
Introduction
The efficacy of vitamin D and calcium supplementation on risk of falling in the elderly is discussed controversially. Randomized controlled trials using falls as primary outcome are needed. We investigated long-term effects of calcium and vitamin D on falls and parameters of muscle function in community-dwelling elderly women and men.
Methods
Our study population consisted of 242 individuals recruited by advertisements and mailing lists (mean [ ± SD] age, 77 ± 4 years). All serum 25-hydroxyvitamin D (25[OH]D) levels were below 78 nmol/l. Individuals received in a double blinded fashion either 1000 mg of calcium or 1000 mg of calcium plus 800 IU of vitamin D per day over a treatment period of 12 months, which was followed by a treatment-free but still blinded observation period of 8 months. Falls were documented using diaries. The study took place in Bad Pyrmont, Germany (latitude 52°) and Graz, Austria (latitude 46°).
Results
Compared to calcium mono, supplementation with calcium plus vitamin D resulted in a significant decrease in the number of subjects with first falls of 27% at month 12 (RR = 0.73; CI = 0.54–0.96) and 39% at month 20 (RR = 0.61; CI = 0.34–0.76). Concerning secondary endpoints, we observed significant improvements in quadriceps strength of 8%, a decrease in body sway of 28%, and a decrease in time needed to perform the TUG test of 11%.
Discussion
Combined calcium and vitamin D supplementation proved superior to calcium alone in reducing the number of falls and improving muscle function in community-dwelling older individuals.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
According to a Cochrane Review published in 2003, roughly 50% of osteoporotic fractures are non-vertebral, and falls appear to be the biggest contributor to such fractures [1]. Low bone mineral density, for instance has been shown to be less predictive than reported falls for future limb fractures in women across Europe [2]. Annual falls occur in 30% of people over the age of 65 years and in 50% of people over age 80 [3–5]. Increased risk of falling is associated with subsequent admission to a nursing home [6]. About 20% of fall incidents require medical attention, and approximately 10% result in fractures [3, 6–10].
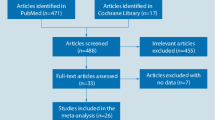
In a first pilot study, Pfeifer et al. [11] compared the short-term effect of vitamin D (800 IU) and calcium (1200 mg) daily versus 1200 mg of calcium alone in 148 healthy women aged 70 years or older [11]. Subjects were treated for eight weeks, but over the following year 28% of the individuals in the calcium group versus 16% of the combination group experienced a fall. This study also demonstrated an improvement in body sway in the vitamin D group, suggesting that vitamin D may improve postural stability [11]. Meanwhile, a variety of studies with vitamin D and calcium supplementation have been looking at falls. In a meta-analysis, Bischoff-Ferrari et al. summarized ten studies [11–20] investigating the effects of vitamin D and its metabolites on falls [21]. The performed sensitivity analysis involving 10,001 participants resulted in a small but significant effect size (corrected OR, 0.87; 95% CI = 0.80–0.96) and subgroup analyses suggested that this was independent of calcium supplementation, type of vitamin D, duration of therapy as well as gender [21]. Several questions remain, however, since most studies of the above mentioned meta-analysis did not include falls as a primary outcome [21]. For that reason, we set up a study dedicated to the outcome of “falls” as the primary study endpoint in long-term vitamin D and calcium supplemented community-dwelling older individuals. In addition, parameters of muscle function such as quadriceps force, body sway and timed-up-and-go test were included as secondary endpoints.
Materials and methods
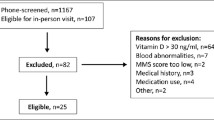
Study subjects
We studied healthy ambulatory women and men 70 years of age or older who were recruited through newspaper advertisements and mailing lists. The inclusion criterion was a 25-(OH)D serum level below 78 nmol/l [22], while the exclusion criteria included hypercalcemia or primary hyperparathyroidism; fractures of the extremities due to osteoporosis; therapy with a thiazide, bisphosphonate, calcitonin, vitamin D and vitamin D metabolites, estrogen, anti-estrogen in the past six months or fluoride treatment in the past two years. Furthermore, known intolerance to study medication, chronic renal failure (serum creatinine above 20% of the upper limit of the reference range), history of drug or alcohol abuse, nicotine abuse (more than 20 cigarettes per day), more than seven cups of coffee daily, scheduled holidays along the geographic longitude during the study period, diabetes mellitus and severe cardiovascular disease were exclusion criteria. Three hundred and fifteen subjects were invited for screening out of which 242 (77%) could finally be enrolled. The protocol was approved by the responsible ethics committees of Graz (Austria) and Hanover (Germany), and written informed consent was obtained from each subject.
Study design and supplements
During a 20-month, double-blind, controlled trial, subjects were randomly assigned to either the calcium mono or the calcium plus vitamin D group. Following month 12, treatment was stopped and study subjects were followed without treatment for an additional 8 months without unblinding the initial treatment code. At study entry, a complete physical examination and assessment of the subjects’ medical history, diet, and physical activity were performed. The subjects were advised to maintain their usual diets and to avoid taking supplemental calcium and vitamin D on their own. The study participants took either one tablet containing 500 mg of elemental calcium in the form of calcium carbonate or one tablet with 500 mg of elemental calcium and 400 IU of cholecalciferol at breakfast and dinner together with the meals. Study medication was provided by Meda Pharma Inc., Vienna, Austria.
The study took place in Bad Pyrmont, Germany (latitude 52°N) and Graz, Austria (latitude 46°N), and commenced in May 2001, when vitamin D levels are starting to rise in spring, and terminated in March 2003 at the end of winter, when vitamin D levels are known to be at their lowest.
Status of subjects and compliance
Treatment compliance was estimated by recording the number of tablets handed out at the visits and the number of tablets returned at visits. Overall compliance was then calculated as a percentage of tablets actually taken by the patient and the number of treatment days between baseline visit and month 12. Eighteen subjects with an overall compliance below 80% were rated as non-compliant. One subject started treatment with raloxifene, and another 12 subjects did not return to all visits. Therefore, 31 subjects were excluded from the per protocol data set.
The number of falls was recorded by fall diaries. Each day the participants had to make a cross depending on whether a fall had occurred or not. Every two months, the study subjects were also asked via telephone interviews whether a fall had happened. If so, it was clarified whether the fall was injurious or non-injurious and further diagnostic procedures like for instance x-rays had been performed or the subject had been admitted to a hospital. A fall was defined as falling onto the floor or ground or hitting an object like a chair or stair. Not included as falls were controlled or intentional movements towards a chair or bed or a near fall in which the participant caught oneself before falling onto the floor or ground. All fractures were the result of falls and were verified by x-rays and medical reports.
Measurements
The calcium and vitamin D intake of the subjects was assessed semi-quantitatively by a food-frequency questionnaire. Physical activities, as well as consumption of alcohol and nicotine, were also determined by questionnaires. Height was measured with a stadiometer, and weight with a digital scale.
Body sway was measured by using a sway meter that measures displacements of the body at the level of the waist in thirty second periods [23]. The device consists of a rod attached to the subject at waist level by a firm belt. The rod is 40 cm in length and extends behind the subject. A digitising tableau is fixed on an adjustable height table located behind the subject. The height of the table is adjusted so that the rod is in a horizontal plane and the tip of a pen can record the movements of the subject via digitising tableau to a computerised system. Displacements of the body in frontal and sagittal direction were recorded. In addition, the sway area was calculated by multiplying the frontal diameter with the sagittal diameter. The coefficients of variation for the measurements were 1.7% (frontal diameter), 1.5% (sagittal diameter), and 2.5% (area) [11, 26].
This study used the timed-up-and-go test (TUG) described by Podsiadlo and Richardson [24, 25]. A special clinical examination room was used to perform all TUG tests. Subjects were observed and timed from the instant they rose from an armchair (seat height 48 cm; arm height 68 cm), walked 3 metres, navigated an obstacle on the floor (i.e. a brick placed at a distance of 3 meters from the chair), and returned to a fully seated position in the chair. Subjects wore their regular footwear and were allowed to use the arms of the chair to get up. Subjects began the test on the word, “go” and were instructed to “walk at a comfortable fast and secure pace”. Each subject performed the TUG test three times and the fastest of these three trials was finally recorded. The score used describes the time in seconds that the subject needed to complete the test. The test-retest reliability of the TUG test performance scores was assessed on a random sample of 20 subjects at each center. Spearman`s rank correlation coefficients were used to assess inter-rater reliability (Inter-rater reliability = 0.91 in Graz and 0.92 in Bad Pyrmont) and intra-observer-reliability (0.96 in Graz and 0.94 in Bad Pyrmont, respectively).
Maximum isometric leg extensor strength was assessed at the non-dominant leg with a computerised strain gauge dynamometer (Digimax, Hamburg, Germany) in the seated position: the hip and knee set at 90° [26]. The force data were analyzed using computer software provided by the manufacturer, and in all strength measurements, the best result of the three consecutive recordings was used in the final statistical analysis. Calibration of the dynamometer was carried out daily prior to the measurements and a cross-calibration between both centers was performed at the beginning and after 12 months of the study.
Laboratory analyses
Blood was drawn between 8:00 and 9:00 a.m. after the subjects had fasted for at least eight hours. Serum 25-(OH)D was measured by radioimmunoassay following extraction (Immunodiagnostic Systems, Boldon, UK). To validate the in-house performance of the assay system we also measured 102 patient samples by HPLC which yield an overall correlation of r = 0.96 and r = 0.92. Parathyroid hormone was analyzed using Elecsys Intact PTH (Roche Diagnostics). Serum creatinine was determined by the Jaffé method, gamma-GT by the Szasz method, and albumin by the bromkresolgreen method. The coefficients of variation for the assays ranged from 5.5% to 7.9%. All samples, except for the screening samples, were frozen at –80°C and analysed at the same time.
Outcome measures
The main outcome measure was the occurrence of falls at months 20 as determined by diaries. Secondary endpoints included non-vertebral fractures, isometric leg extensor strength, body sway total path length, TUG test score, serum 25-(OH)D, and parathyroid hormone levels.
Quality assurance and statistical analyses
Quality assurance was conducted by the contract research organisation (CRO) Dr. Robert Heinz & Partners, Medical Consulting (Vienna, Austria). A start-up meeting with investigators and monitors took place before the start of the clinical trial. Follow-up meetings were performed after 12 months and at the end of the study. Periodical monitoring was conducted every 2 months by designated monitors.
Statistical calculations were conducted with the statistical software of IDV, Gauting, Germany, using the Testimate part of the program (Test & Estimation, version 5.2). All study subjects, who were initially randomized and received study medication had been included into the analysis (intention-to-treat analysis).
The sample size was calculated based on the following considerations: Pfeifer et al. [19] observed a total of 30 falls in the calcium mono group (45% of study subjects sustained at least one fall), and 17 falls in the calcium plus vitamin D group (24% of study subjects) over a one-year period. With α = 0.05 and β = 0.20, a significantly better effect of the calcium plus vitamin D combination should be demonstrated with respect to the primary study parameter “number of falls”. In order to identify such a statistically significant effect in a two-sided test, 97 study subjects were required in each group, which totals a number of 194 analysable subjects. Given the age range of study participants, a drop-out rate of 20% was assumed and 242 study subjects (121 per treatment group) were included in this clinical trial.
With regard to the primary target parameter, “number of falls during the course of the study”, statistical comparisons for the two treatment groups were conducted using the Wilcoxon–Mann–Whitney U-test, whereas type I statistical error was set at 0.05. In addition, a Kaplan–Meier analysis had been calculated in order to demonstrate differences over time.
The time to first fracture was analyzed separately using a Cox regression analysis providing a 95% confidence interval.
Statistical comparisons of secondary target parameters comprised inter-group and intra-group calculations. Both comparisons were conducted with the Wilcoxon–Mann–Whitney U-test.
Results
Of the 315 subjects who underwent screening, 242 (77%) fulfilled all inclusion and exclusion criteria and their 25-(OH)D serum level was below 78 nmol/l. The baseline characteristics of the 242 subjects enrolled in this trial are shown in Table 1. Both treatment groups did not differ in terms of age, height, weight, gender, serum 25(OH)D, nutritional calcium intake, and intact parathyroid hormone (PTH) levels. An intense homogeneity analysis of these data sets did not reveal any clinically relevant differences between the two centers. For that reason a combined data analysis of the two sites was performed.
Compared to baseline an expected increase in mean serum 25(OH)D level was observed after 12 months of treatment in the calcium plus vitamin D treated group whereas 25(OH)D levels were similar to baseline in the calcium mono group (Table 2). By the end of the treatment-free observation period 25(OH)D levels had decreased to below baseline levels in both groups and were still significantly higher in the calcium plus vitamin D group. In both groups serum PTH levels showed a similar decline by month 12 and were no longer different to baseline values by the end of the observation period.
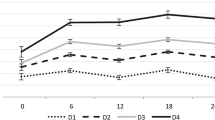
Quadriceps strength at the left leg was significantly higher in the calcium plus vitamin D group at month 12 when compared to either baseline (p < 0.001) or the calcium mono group (p < 0.01). This difference remained statistically significant at the end of the observation period. Similar results were observed with respect to the timed-up-and-go test: significant decreases in the mean time needed to perform the test were observed during treatment with calcium plus vitamin D compared to baseline (p < 0.001) as well as to the calcium mono group (p < 0.05). These differences remained significant at the end of the trial (p < 0.001 compared to baseline versus p < 0.05 compared to calcium mono). Interestingly, no differences in body sway were seen at month 12 in comparison to baseline. At the end of the observation period; however, the former calcium plus vitamin D group showed a significant improvement in body sway compared to baseline (p < 0.001) as well as to the calcium mono group (p < 0.05).
Falls were followed by diaries and decreased significantly over time. The cumulative development of the number of subjects with no falls is shown in a Kaplan–Meier analysis in Fig. 1. During this 20 months lasting clinical trial, 63% of the individuals in the calcium mono group versus 40% in the calcium plus vitamin D group experienced at least one fall (p < 0.001). The mean number of falls per group was 1.41 in the calcium mono group and 0.63 in the calcium plus vitamin D group (p < 0.001). This translated into a total number of falls of 171 in the calcium mono group and to 76 falls in the calcium plus vitamin D group (Tables 3 and 4).
The time to first fall was evaluated using a Cox regression analysis providing a 95% confidence interval. Concerning the time to first fall, we observed at month 12 a 27% reduction in the vitamin D plus calcium group as compared to the calcium mono group. This reduction was statistically significant (RR = 0.73; 95% CI 0.54–0.96; p < 0.01). At month 20 this comparable reduction reached 39% and was also statistical significant (RR = 0.61; 95% CI 0.34–0.76; p < 0.01).
This reduced number of falls was accompanied by a reduction in the number of fractures: we observed 19 fractures in the calcium mono group and 12 fractures in the calcium plus vitamin D group (p = 0.12). This study, however, was not powered to detect a significant reduction in the number of fractures. In total, 13 subjects in the calcium mono group and seven participants in the calcium plus vitamin D group experienced at least one fracture, a result that did not reach the level of statistical significance (p = 0.08).
Discussion
In this study, long-term supplementation with vitamin D and calcium reduced the number of falls and improved parameters of muscle function in community-dwelling men and women 70 years of age or older in the communities of Bad Pyrmont, Germany (latitude 52°) and Graz, Austria (latitude 46°). Essentially, these results are in accordance with the meta-analysis published by Bischoff-Ferrari et al., who demonstrated in a sensitivity analysis of 10 RCTs that vitamin D supplementation may reduce the risk of falls by 16% [21]. In addition, our observed improvements in functional measures (quadriceps strength, body sway, and timed-up-and-go test) are consistent with a RCT by Bischoff-Ferrari et al., in which 122 elderly women in long-stay geriatric care showed a significant increase in overall musculoskeletal function (knee flexor and extensor strength, grip strength, and timed-up-and-go test) after supplementation of daily doses of 800 IU vitamin D and 1200 mg calcium [12]. However, most of the studies available so far did not measure quadriceps force, body sway, or perform the timed-up-and-go test in community-dwelling older individuals.
Furthermore, Bischoff-Ferrari et al. demonstrated in a population-based survey of the ambulatory US population aged 60 to >90 years (n = 4,100) that higher 25(OH)D concentrations were associated with better lower-extremity function as assessed by an eight-foot walk test [27].
Among 124 nursing home residents, Broe et al. demonstrated a significant reduction in the number of falls after a relatively short period of time of 5 months [28]. Participants who received 800 IU of vitamin D per day had a 72% lower rate ratio of falls than those taking only placebo over the 5 months (RR = 0.28; 95% CI = 0.11–0.75). The results of this study demonstrate very clearly that baseline risk for falling may determine the outcome after vitamin D and calcium supplementation. With a mean age of 89 years, nursing home residents have a higher risk of falling than ambulatory elderly with a mean age of 77 years. This may also be due to a lower rate of sun exposure and vitamin D synthesis in the skin among this group of nursing home residents.
In another long-term study, Bischoff-Ferrari et al. treated 199 ambulatory men and 246 women at the age of 65 years or older with either 700 IU of cholecalciferol plus 500 mg of calcium citrate or placebo in a double-blind manner over a period of three years [29]. At the end of this clinical trial vitamin D plus calcium reduced the risk of falling only in women (OR = 0.54; 95% CI = 0.30–0.97) but not in men (OR = 0.93; 95% CI = 0.50–1.72) [29]. In our study population men represent only 25% and for that reason it was not possible to perform a separate analysis for men. Men tend to have a higher muscle mass and in this study they had a slightly higher baseline 25(OH)D level than women. One might expect, however, that with increasing age and frailty men also may profit from vitamin D and calcium supplementation, but this requires further studies.
In 2005 two other important studies demonstrating positive effects of a vitamin D and calcium supplementation on risk of falls have been published: the first by Larsen et al. showing a decrease in the number of severe falls in 5,771 elderly community-dwelling women [30]. Those women, who received treatment of 400 I.U. of vitamin D and 1000 mg of elemental calcium had a 12% risk reduction in severe falls (RR 0.88; 95% CI = 0.79–0.98; p < 0.05; NNT 9) in comparison to women, who were offered home safety inspection with health advice for fall prevention. The second clinical trial was published by Flicker et al., who demonstrated a significant decrease in the risk of falls among 625 residents of hostels and nursing homes across Australia [31]. The participants with a mean age of 83 years and serum 25(OH)D levels between 25 and 90 nmol/l received either 1000 I.U. of vitamin D or placebo for 2 years. In addition, all subjects received 600 mg of elemental calcium daily. In an intention-to-treat analysis, the incident rate ratio for falling was 0.73 (95% CI = 0.57–0.95; p < 0.05).
In sharp contrast to all of these findings are two large double-blind RCTs from the UK also published in 2005 [32, 33]. The so-called RECORD trial tested 800 I.U. of vitamin D with or without calcium among 5,292 people aged 70 years or older who were mobile before developing a low-trauma fracture [32]. The incidence of new, low-trauma fractures did not differ significantly between participants allocated to 800 I.U. of vitamin D per day and those without treatment (OR 1.02; 95% CI = 0.88–1.19). These results, however, may be explained by a rather low adherence rate, which was 60% at 12 months and 47% at 24 months among subjects who returned the 4-month questionnaire. A low adherence rate was also observed in the second trial published by Porthouse et al. [33]. In this open-label pragmatic trial in a primary care setting, 3,314 women aged 70 and over with one or more risk factors for hip fracture were randomized to either supplementation of 800 I.U. vitamin D and 1000 mg calcium or no treatment. Furthermore, both groups received an information leaflet on dietary calcium intake and prevention of falls. Adherence rates in the intervention group were 63% at 12 months and 59% at 18 months. In both trials, the assessment of falls was not performed using diaries and that may have biased the results since falls may have been forgotten by the study subjects. In clinical trials using falls as a primary endpoint diaries may be a prerequisite [34, 35].
In both trials from the UK, rather low rates of compliance may have contributed to a relatively small increase in serum levels of 25(OH)D. In the RECORD trial, for example, mean 25(OH)D values in the treatment group reached 62 nmol/l. This value is below a threshold of 75 nmol/l (=30 ng/ml), which was proposed by an expert panel as the serum 25(OH)D concentration at which older men and women will be at a lower risk of fracture [36]. In our study mean serum 25(OH)D values above 80 nmol/l were reached in the treatment group. Seasonal variations, however, interfered with our results: differences between treatment and control group were most pronounced at the end of winter, when 25(OH)D serum levels were at their lowest. This is in accordance with the findings by Pasco JA et al., who demonstrated in a population-based study that seasonal periodicity was seen with reduced serum 25(OH)D, increased serum PTH, and increased bone resorption in winter [37]. Furthermore, this was associated with an increased proportion of falls resulting in fracture and an increased risk of wrist and hip fractures [37]. Interestingly, in our study, we still observed significant differences in 25(OH)D levels between treatment and control groups after month 20 indicating that part of the vitamin D stored during treatment was still available eight months following cessation of supplementation.
Our study demonstrates that long-term supplementation with 800 I.U. of vitamin D and 1000 mg of elemental calcium is effective in reducing the risk of falls in elderly community-dwelling people with 25(OH)D serum levels below the desirable range of 75 nmol/l. In this context, it should be noted that our study subjects, who were recruited by newspaper advertisements or mailing lists out of the general population were probably healthier than their age-related counterparts. Between centers and different latitudes, we only observed small differences without clinical relevance. In addition, our results provide good evidence that this effect on the risk of falls is mediated by an improvement in parameters of muscle function particularly of the lower extremities. The ability to store vitamin D over a longer period of time is a vital prerequisite to survive seasonal periodicity of sunshine and UVB-radiation on earth.
References
Gillespie LD, Gillespie WJ, Robertson MC, Lamb SE, Cumming RG, Rowe BH (2003) Interventions for preventing falls in elderly people. The Cochrane Database of Systematic Reviews, Issue 4, Art. No.: CD000340
Kaptoge S, Benevolenskaja LI, Bhalla AK et al (2005) Low BMD is less predictive than reported falls for future limb fractures in women across Europe: Results from the European Prospective Osteoporosis Study. Bone 36:387–398
Tinetti ME, Speechley M, Ginter SF (1988) Risk factors for falls among elderly people living in the community. N Engl J Med 319:1701–1707
O’Loughlin JL, Robitaille Y, Boivin JF, Suissa S (1993) Incidence of and risk factors for falls and injurious falls among the community-dwelling elderly. Am J Epidemiol 137:342–354
Blake AJ, Morgan K, Bendall MJ et al (1998) Falls by elderly people at home: prevalence and associated factors. Age Ageing 17:365–372
Reinsch S, MacRae P, Lachenbruch PA, Tobis JS (1992) Attempts to prvent falls and injury: a prospective community study. Gerontologist 32:450–456
Tinetti ME, Baker DL, McAvay G et al (1994) A multifactorial intervention to reduce the risk of falling among elderly people living in the community. N Engl J Med 331:821–827
Campbell AJ, Borrie MJ, Spears GF, Jackson SL, Brown JS (1990) Circumstances and consequences of falls experienced by a community population 70 years and over during a prospective study. Age Ageing 19:36–41
Berg WC, Alessio HM, Mills EM, Tong C (1997) Circumstances and consequences of falls in independent community-dwelling older adults. Age Ageing 26:261–268
Tinetti ME, Williams CS (1997) Falls, injuries due to falls, and the risk of admission to a nursing home. N Engl J Med 337:1279–1284
Pfeifer M, Begerow B, Minne HW, Abrams C, Nachtigall D, Hansen C (2000) Effects of a short-term vitamin D and calcium supplementation on body sway and secondary hyperparathyroidism in elderly women. J Bone Miner Res 15:1113–1118
Bischoff HA, Stähelin HB, Dick W et al. (2003) Effects of vitamin D and calcium supplementation on falls. J Bone Miner Res 343–351
Latham NK, Anderson CS, Lee A, Bennett DA, Moseley A, Cameron ID (2003) A randomised, controlled trail of quadriceps resistence exercise and vitamin D in frail older people: the Frailty Interventions Trail in Elderly Subjects (FITNESS). J Am Geriatr Soc 51:291–299
Graafmans WC, Ooms ME, Hofstee HM, Bezemer PD, Bouter LM, Lips P (1996) Falls in the elderly: a prospective study of risk factors and risk profiles. Am J Epidemiol 143:1129–1136
Dukas L, Bischoff HA, Lindpaintner S et al (2004) Alfacalcidol reduces the number of fallers in a community-dwelling elderly population with a minimum calcium intake of more than 500 mg daily. J Am Geriatr Soc 52:230–236
Trivedi DP, Doll R, Khaw (2003) Effect of four monthly oral vitamin D3 (cholecalciferol) supplementation on fractures and mortality in men and women living in the community. Br Med J 326–329
Gallagher JC, Fowler SE, Detter JR, Sherman SS (2001) Combination treatment with estrogen and calcitriol in the prevention of age-related bone loss. J Clin Endorcinol Metab 86:3618–3628
Larsen ER, Mosekilde L, Foldspang A (2004) Vitamin D and calcium supplementation prevents osteoporotic fractures in elderly community dwelling residents: a pragmatic population-based 3-year intervention study. J Bone Miner Res 19:370–378
Chapuy MC, Pamphile R, Paris E et al (2002) Combined calcium and vitamin D3 supplementation in elderly women. A confirmative study: Decalyos II. Osteoporos Int 13:257–264
Harwood RH, Sahota O, Gaynor K, Masud T, Hosking D (2004) A randomised controlled comparison of different calcium and vitamin D supplementation regimens in elderly women after hip fracture: The Nottigham Neck of Femur (NoNOF) Study. Age Ageing 33:45–51
Bischoff-Ferrari HA, Dawson-Hughes B, Willett WC et al (2004) Effect of vitamin D on falls: a meta-analysis. J Am Med Assoc 291:1999–2006
Chapuy MC, Preziosi P, Maamer M et al (1997) Prevalence of vitamin D insufficiency in an adult normal population. Osteoporos Int 7:439–443
Lord SR, Clark RD, Webster IW et al (1991) Postural stability and associated physiological factors in a population of aged persons. J Gerontol 46:M69–M79
Podsiadlo D, Richardson S (1991) The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc 39:142–148
Bischoff HA, Stähelin HB, Monsch AU et al (2003) Identifying a cut-off point for normal mobility: a comparison of the timed “up and go” test in a community-dwelling and institutionalized elderly women. Age and Aging 32:315–320
Pfeifer M, Begerow B, Minne HW et al (2001) Vitamin D, muscle strength, body sway, falls, and fractures among 237 postmenopausal women with osteoporosis. Exp Endocrinol Metab Diabetes 109:87–92
Bischoff-Ferrari HA, Dietrich T, Orav EJ et al (2004) Higher 25-hydroxyvitamin D concentrations are associated with better lower-extremity function in both active and inactive persons aged >60 y. Am J Clin Nutr 80:752–758
Broe KE, Chen TC, Weinberg J, Bischoff-Ferrari HA, Holick MF, Kiel DP (2007) A higher dose of vitamin D reduces the risk of falls in nursing home residents: a randomized, multiple-dose study. J Am Geriatr Soc 55:234–239
Bischoff-Ferrari HA, Orav EJ, Dawson-Hughes B (2006) Effect of cholecalciferol plus calcium on falling in ambulatory older men and women: a 3-year randomized controlled trial. Arch Intern Med 166:424–430
Larsen ER, Mosekilde L, Foldspang A (2005) Vitamin D and calcium supplementation prevents severe falls in elderly community-dwelling women: a pragmatic population-based 3-year intervention study. Aging Clin Exp Res 17:125–132
Flicker L, MacInnis RJ, Stein MS et al (2005) Should older people in residential care receive vitamin D to prevent falls ? Results of a randomized trial. J Am Geriatr Soc 53:1881–1888
Grant AM, Avenell A, Campbell MK et al (2005) Oral vitamin D3 and calcium for secondary prevention of low-trauma fractures in elderly people (Randomised Evaluation of Calcium Or vitamin D, RECORD): a randomised placebo-controlled trial. Lancet 365:1621–1628
Porthouse J, Cockayne S, King C et al (2005) Randomised controlled trial of calcium and supplementation with cholecalciferol (vitamin D3) for prevention of fractures in primary care. BMJ 330:1003–1009
Cummings SM, Nevitt MC, Kidd S (1988) Forgetting falls: the limited recall of falls in the elderly. J Am Geriatr Soc 36:613–616
Nevitt MC, Cummings SR, Kidd S, Black D (1989) Risk factors for recurrent nonsyncopal falls. J Am Med Assoc 261:2663–2668
Dawson-Hughes B, Heaney RP, Holick MF, Lips P, Meunier PJ, Vieth R (2005) Estimates of optimal vitamin D status. Osteoporos Int 16:713–716
Pasco JA, Henry MJ, Kotowicz MA et al (2004) Seasonal periodicity of serum vitamin D and parathyroid hormone, bone resorption, and fractures: the Geelong osteoporosis study. J Bone Miner Res 19:752–758
Acknowledgements
We are grateful to Dr. D. Lazarescu M.P.H. (Advanced Statistics Wiesbaden, Germany), who performed the Cox regression analysis and to Dr. H.A. Griesser, editor-in-chief of our local newspaper (DEWEZET, Hameln, Germany). for his help in recruiting the participants of this study. Meda Pharma Inc. Vienna, Austria, which markets vitamin D and calcium, provided the drugs and funding for the study. However, Meda had no control over the decision to approve or submit the manuscript for publication. Audits have been performed routinely by the Austrian Ministry of Health (Ministerium für Familie, Frauen und Gesundheit), Vienna, Austria and by the corresponding German Ministry for the approval of investigational products (Bundesamt für Arzneimittel und Medizinprodukte), Bonn, Germany.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pfeifer, M., Begerow, B., Minne, H.W. et al. Effects of a long-term vitamin D and calcium supplementation on falls and parameters of muscle function in community-dwelling older individuals. Osteoporos Int 20, 315–322 (2009). https://doi.org/10.1007/s00198-008-0662-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-008-0662-7