Abstract
Summary
The real cumulative persistence probabilities with bisphosphonates after 5 years was 51.7%. Prescriptions by specialists other than gynecologists and rheumatologists (p < 0.001), male sex (p < 0.001), older age (≥65 years) (p = 0.001), and cyclical etidronate (p < 0.001) were significantly associated with low persistence. Success rates of switching bisphosphonate were 75.6%.
Introduction
Many patients discontinue daily bisphosphonate therapy prematurely due to the stringent dosing procedures and adverse events. Consequently, some patients are receiving two or more sequential bisphosphonates in daily practice. Our objective was to study factors associated with the real cumulative persistence with bisphosphonate therapy including treatment courses with multiple sequential drugs in the real world setting.
Methods
We retrospectively analyzed 1,307 patients (male 197, female 1110) newly prescribed with bisphosphonates between January 1, 2000, and June 30, 2005.
Results
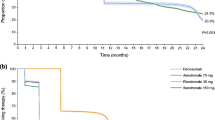
The real cumulative persistence probabilities with bisphosphonates after 1, 3, and 5 years were 74.8%, 60.6%, and 51.7%, respectively. Switching of bisphosphonates was observed 168 times in 146 patients. Adverse events occurred 126 times in 124 patients including 86 events with gastrointestinal complaints. Univariate analysis showed that prescriptions by specialists other than gynecologists and rheumatologists (p < 0.001), male sex (p < 0.001), older age (≥65 years) (p = 0.001), and cyclical etidronate (p < 0.001) were significantly associated with low persistence. Success rates of switching bisphosphonate were 75.6%.
Conclusions
Switching of bisphosphonates was not uncommon. Despite switching bisphosphonates to improve persistence, the real cumulative persistence with bisphosphonate was suboptimal, especially among patients of certain physician specialties and male sex.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bisphosphonates are potent inhibitors of the osteoclast-mediated resorption of bone and, thus, useful for increasing bone mass [1]. Long-term adherence to bisphosphonates is required to realize the full benefits of treatment [1, 2]. Medication adherence consists of persistence (i.e., the length of time on therapy) and compliance (i.e., the consistency and accuracy with which the prescribed regimen is followed). These terms have been used interchangeably in the literature, which has led to misconceptions, and must be standardized [3]. Variable percentages of persistence have been documented for patients who do start treatment with antiresorptive agents, with levels from 24.2% [4] to 90.3% [5] after 1 year. Many issues may impact long-term persistence with osteoporosis medication, including cost and availability, real or perceived adverse events, dosing frequency and convenience, the number of concomitant diseases and medications, and patients’ understanding of their test results and need for therapy [6]. The causes of discontinuation to medical therapy for osteoporosis in patients treated in clinical practice are complex and poorly defined, and the rates are likely to be worse than those reported in patients participating in clinical trials, where the latter are probably healthier and better counseled than patients in clinical practice.
Most of persistence studies of medications in the treatment and prevention of osteoporosis deal with a single drug. However some patients are receiving two or more sequential bisphosphonates for various reasons in daily practice. In a sense, these patients are “really bisphosphonate persistent”, if they were taking different bisphosphonates sequentially.
The aim of our retrospective cohort study was to identify the proportion of patients who stayed on sequential bisphosphonates, the incidence of adverse events in non-research settings, and to define which factors determined real persistence with bisphosphonates at a single university hospital in Japan. We report here the rate and possible determinants of low persistence with bisphosphonates in a large number of patients in a routine clinical setting.
Methods
Yokohama City University Medical Center is a tertiary referral hospital with 720 beds in Yokohama City, Japan. A computer database to monitor all consecutive patients seen at Yokohama City University Medical Center has been maintained since January 1, 2000. The computer database includes pharmacy records of prescriptions, laboratory data, as well as information on patients characteristics. Patients were included in this study when bisphosphonates were newly started at Yokohama City University Medical Center during the period from January 1, 2000 to June 30, 2005. By means of chart review and computer database, we collected data on the patients’ age at the start of bisphosphonates, sex, the dates of starting and ending of bisphosphonates, types of bisphosphonates used, specialties of prescribers, dates and reasons for incidental discontinuation. The following were the types of bisphosphonates studied: (1) cyclical etidronate 200 mg or 400 mg daily (etidronate is administered for 14 days every 3 months) approved in Japan in July, 1996; (2) alendronate 5 mg daily approved in Japan in August, 2001; (3) risedronate 2.5 mg daily approved in Japan in May, 2002. In Japan, weekly alendronate or risedronate therapy was not approved during this study period. The study endpoint was the discontinuation of therapy with any bisphosphonates. Patients treated with two or more sequential bisphosphonates (switching of bisphosphonates), actually discontinued a single bisphosphonate, but they were regarded as “really bisphosphonate persistent” if they were taking bisphosphonates sequentially. If the gap between the end of 1 prescription and the start of the next prescription was less than 3 months [7, 8], the treatment was considered to be uninterrupted, even if an alternative new bisphosphonate was started. The treatment period was measured as the time span between the start of the first prescription and the end of the final prescription.
We checked the prescriptions of bisphosphonates and investigated reasons for the termination of bisphosphonates at the end of the study. Major reasons for the termination of bisphosphonates were registered and classified as adverse event, health problem, patient’s request, doctor’s careless lack of refilling a prescription, and other reason. The category “patient’s requests” indicates discontinuation at the wish of the patient, e.g., due to anxiety over adverse events or unwillingness to take medication. Adverse events leading to bisphosphonate’s withdrawal were categorized as: subjective adverse events (such as gastrointestinal (GI) complaints, eruption, arthralgia, etc.), laboratory abnormalities, and miscellaneous.
Statistical analysis was carried out using SPSS version 11.0 (SPSS Inc., Chicago, Illinois, USA). Life table analysis data were used to calculate cumulative drug persistence probability. Univariate and multivariate analysis were carried out by means of Cox regression. In a univariate analysis the relation between various clinical factors and persistence with bisphosphonates were studied. A p value <0.05 was considered significant. Significant parameters on univariate analysis were entered into a multivariate Cox regression model to identify independent predictors of persistence.
Results
Using the computer database, we identified 1,307 patients eligible for our study. Baseline patient’s characteristics are listed in Table 1. The mean (SD) age of the study population was 61.3 (14.8) years (range 13.3–91.6 yrs). One thousand one hundred and ten patients (84.9%) were female. Overall, 1,307 patients received total of 1475 bisphosphonate prescriptions. One hundred and forty-six patients received two or more sequential drugs with switching of bisphosphonates in 168 cases. 1161 patients (88.8%) were prescribed with one bisphosphonate. One hundred and twenty-six patients (9.6%), 18 patients (1.4%), and 2 patients (0.2%) were prescribed with two, three, and four bisphosphonates, respectively.
Six hundred and ninety-seven patients younger than 65 years were classified as young group, and 610 patients (≥65 years) were classified as old group. Seven hundred and twenty-nine patients (55.8%) received bisphosphonates from rheumatologists, 311 patients (23.8%) from orthopedists, 123 patients (9.4%) from gynecologists, and 144 patients (11.0%) from other specialists. Cyclical etidronate was prescribed 495 times (33.6%) newly or after switching, alendronate was prescribed 801 times (54.3%), and risedronate was prescribed 179 times (12.1%).
The real cumulative persistence probabilities of bisphosphonate treatment were 74.8% after 1 year, 60.6% after 3 years, and 51.7% after 5 years, respectively. Median time to discontinuation was 342.0 days. In the light of 1475 continuous bisphosphonate prescriptions, reasons for discontinuation included adverse events in 88 times (22.9% of 385 discontinuations). Switching of bisphosphonates occurred in 168 times (Table 2).
In total of 126 adverse events happened in 124 patients. Subjective adverse events were observed in 115 events (91.3% of all adverse events), and laboratory abnormalities in eight events (6.3%). Gastrointestinal events including gastric pain (60 events), diarrhea and/or constipation (12 events), stomatitis (eight events), and heartburn (6 events) were observed in 86 events. Laboratory abnormalities leading to discontinuation were observed in eight events (increase of creatinine: four events, elevated liver function test: three events, and increase of creatine kinase: one event) and all normalized after discontinuation. Two patients discontinued bisphosphonate in preparation for pregnancy.
Switching of bisphosphonates was occurred 168 times in 146 patients. Switching to cyclic etidronate was observed 47 times mainly for patient’s request against stringent dosing procedure of daily bisphosphonates (18 times). Switching to daily alendronate or daily risedronate was observed 77 and 44 times mainly for doctor’s request against their careless lack of refilling prescription. If subsequent bisphosphonates were prescribed for more than 6 months continuously, switching of bisphosphonates was considered as successful. Success rates of switching bisphosphonate were 68.1% in switching to cyclic etidronate group and 78.5% in switching to daily alendronate or daily risedronate group, which were not statistically significant different (Table 3). Among these cases, success rate of switching bisphosphonates due to adverse events, success rates were 68.8% in switching to cyclic etidronate group and 55.0% in switching to daily alendronate or daily risedronate group, which were not statistically significant different either (Table 4).
A univariate analysis showed that prescriptions by specialists other than gynecologists or rheumatologists (p < 0.001), male sex (p < 0.001), older age (≥65 years) (p = 0.001), and cyclical etidronate (p < 0.001) were significantly associated with low persistence. In a multivariate analysis, prescriptions by specialists other than gynecologists or rheumatologists (p < 0.001), and male sex (p < 0.001) remained significantly related to low persistence (Table 5).
Discussion
Our study found that the real cumulative persistence probabilities of bisphosphonates were 74.8% after 1 year, 60.6% after 3 years, and 51.7% after 5 years, respectively. Because we included patients treated with sequential drugs, our real bisphosphonate persistence probability is higher than those of previous studies with single drug.
One of the main reasons for the treatment discontinuation was adverse events, which accounted for a quarter (22.9%) of all discontinuation cases. The proportion of adverse events for treatment discontinuation is considerably lower than the 80% reported by Tosteson et al. [9], and is consistent with Rossini et al. (25%) [10]. The discrepancy might be due to the different methods of survey. Tosteson et al. conducted a telephone survey, and Rossini et al. did a nation-wide survey carried out in 141 Italian centers where the patients were asked to complete a questionnaire. We reviewed patients’ charts to obtain the reasons for the discontinuation of treatment and did not ask patients further. It is likely that failure to comply with bisphosphonates therapy is primarily a consequence of adverse events or the lack of noticeable symptoms associated with the condition [11]. Previous studies have found that gastrointestinal adverse events are the major reported reason for stopping oral bisphosphonates [12]. In our study, gastrointestinal complaints including gastric pain, diarrhea and/or constipation, stomatitis, and heartburn were observed in 86 events, which account for 68.3% (86/126) of total adverse events. Hamilton et al. reported that 76% of patients who discontinued treatment with risedronate did so because of gastrointestinal adverse events [13].
The specialty of prescribers was significantly associated with treatment persistence. In general, the global persistence to treatment is strongly related to the type of prescriber. Rossini et al. reported determinants of adherence to osteoporosis treatment in clinical practice [10]. They found that adherence was significantly poorer for patients of general practitioners (GPs) and orthopedists, primarily due to a lack of adequate doctor’s motivation. That is in agreement with another study showing that patients of GPs were more likely to discontinue their medications than the patients of internists [14]. In our study, prescriptions by gynecologists or rheumatologists resulted in high persistence (p < 0.001). Gynecologists who treat menopausal disorders generally have high motivation in the management of postmenopausal osteoporosis. They prescribe not only bisphosphonates but also raloxifene or hormone replacement therapy. This may be the reason for the high persistence by gynecologists, regardless of the lower number of treatment courses treated by gynecologists (123 courses, 9.4%). Rheumatologists prescribed bisphosphonates in more than half of the treatment courses (729 courses, 55.8%) in our center. In addition to the treatment of patients with post-menopausal osteoporosis, rheumatologists have more opportunities for prescribing bisphosphonates to prevent glucocorticoid-induced osteoporosis (GIOP) than other specialists and general practitioners. Curtis et al. investigated 6,281 patients who were prescribed with glucocorticoids in 2001–2003. Among them, 3449 patients (54.9%) were treated by rheumatologists. They concluded that the odds of bone mass measurement were highest among the patients who were prescribed glucocorticoids by rheumatologists (OR 1.48), though the patients prescribed by rheumatologists were no more likely to be treated with bisphosphonates than by any other specialists [15]. In our study, patients with prescription from rheumatologists resulted in high persistence. In 729 treatment courses by rheumatologists, 526 courses (72.2%) were co-prescribed with glucocorticoid. On the contrary, only 160 courses were co-prescribed with glucocorticoid in 578 courses by other specialties (27.7%) (p < 0.001). To avoid GIOP, rheumatologists were eagerly prescribing bisphosphonates.
Success rates of switching bisphosphonates were investigated. Switching to cyclic etidronate was observed mainly for patient’s request against stringent dosing procedure of daily bisphosphonates. Switching to daily alendronate or daily risedronate was observed 77 and 44 times mainly for doctor’s request against their careless lack of refilling prescription. Success rates of switching bisphosphonate were 75.6% (127/168) totally. Success rates of switching bisphosphonates due to adverse events were 61.1% (22/36) totally, which was lower than total success rate (75.6%). Adverse events did not happen in 22 courses resulting in successful switching. In 14 courses, subsequent bisphosphonates were discontinued resulting in switching failure. The following were the reasons for failure: adverse events (ten), patient’s requests (dosing procedure) (two), and doctor’s careless lack of refilling a prescription (two). The same adverse events recurred in seven failure courses after switching to another formulation, which were all gastrointestinal events. Switching bisphosphonates were done 121, 27, 18, and two times by rheumatologist, orthopedist, gynecologist, and other specialist, respectively. Success rates were 74.4%(90/121), 77.8%(21/27), 88.9%(16/18), and 0%(0/2), respectively. Rheumatologists, orthopedists, and gynecologists frequently tried to switching bisphosphonates, and acquired high success rates than other specialists (p = 0.012).
Persistence may also be affected by dosing regimen. Cyclic etidronate was one of the risk factors for discontinuation (p < 0.001). In our study, doctor’s careless lack of refilling a prescription all occurred in the etidronate treatment group. Cyclical etidronate is administered for 14 days every 3 months. This interval results in the tendency of doctor’s careless lack of refilling a prescription. In Europe and Canada, etidronates are dispensed in 90-day combination packages, including 14 tablets of 400 mg etidronate and 76 tablets of 500 mg calcium carbonate [5, 16]. This regimen might improve the persistence with cyclical etidronates.
In a meta-analysis of the efficacy of bisphosphonates in the treatment of osteoporosis, only two agents, alendronate and risedronate provided convincing evidence for nonvertebral fracture reduction, and cyclic etidronate did not [17]. Another study determined that cyclic etidronate is significantly less potent in increasing bone mineral density of the lumbar spine (L2-L4 BMD) than risedronate [18]. Considering the strong evidence of alendronate and risedronate, doctors may have a tendency of switching cyclical etidronate to alendronate or risedronate. In our study, 168 times were switched of bisphosphonates. Among them, 97 times (57.7%) previously prescribed with cyclical etidronate, switched to alendronate or risedronate.
Alendronate 5 mg, or risedronate 2.5 mg is given daily and it must be taken with a glass of water, on an empty stomach, with nothing to eat or drink for at least 30 min and without any other medication [5]. Some patients find this dosing protocol to be challenging which may lead to higher discontinuation rates. An assessment of medication use of alendronate found that 30% of the reasons for discontinuation of alendronate were due to issues with administration [19]. The fact that persistence with alendronate therapy may have been influenced by its dosing regimen suggests that the more recent availability of a once-weekly therapy as well as other bisphosphonate with less frequent dosing may improve persistence.
Male sex was an independent determinant of low persistence with bisphosphonates (p < 0.001). Tanaka et al. investigated persistence with alendronate and the reason for the discontinuatin of treatment for 327 Japanese osteoporotic patients [20]. Although it was not significant, they found that alendronate persistence was higher in women than in men. They assumed that it might have been due to the different lifestyles between sexes.
Patient’s age, particularly for those younger than 65 years of age, contributed to bisphosphonates persistence, even though it is not an independent determinant (p = 0.063). This may be explained by the balancing of decreasing general persistence with advancing age and the increased motivation for treatment for the severity of the disease [10].
There are several limitations of the approach used in this study: (1) Only persistence, not compliance, was examined. It is unknown whether patients actually took the dispensed drug; however, it seems likely that patients who obtain prescription refills do take their medication based on chart review. (2) Heterogeneity of patients population. For example, diagnosis of osteoporosis, and reasons for bisphosphonate prescription were not examined; (3) lack of data concerning bone mineral density and previous fracture.; (4) Data from a tertiary university hospital, which may not necessarily reflect common daily clinical practice. (5) Ethnic diversity which might be responsible for the incidence of adverse events and/or inefficacy of bisphosphonate, that could influence the difference of persistence between Japan and Western countries. (6) Differences of medical treatment costs. All Japanese citizens are required to participate in one of two general categories of public health coverage, the Employees’ Health Insurance (EHI) or the National Health Insurance (NHI) [21]. In addition, medical treatment cost payment system was designed to reduce the cost recovering from public funds for the patients with severe and/or rare intractable diseases (45 such conditions are currently specified) [22]. We did not differentiate patients with or without medical treatment cost payment system.
There are some strengths in our study. Some studies have investigated persistence with bisphosphonate therapy and determinants to persistence previously. Most studies use huge drug-dispensing database systems that include heterogeneous patient populations treated by heterogeneous physicians. In addition, most of the previous studies targeted only postmenopausal women or chronic glucocorticoid users. In this study, the patients’ age ranged widely from 13.3 years to 91.6 years, and not only women but also men were studied. The long observational period (5.5 years) is another strength. To our knowledge, this is a unique study conducted at one university hospital over a long period. Finally, and most importantly, we investigated “real bisphosphonate persistence”, which might reflect real clinical practice well.
In this retrospective study of 1,307 patients at a single university hospital, real persistence with bisphosphonates was higher than most of the previous studies with single drug, although it was still suboptimal. Specialty of prescribers and sex were independent determinants of persistence with bisphosphonates therapy. One of the main reasons for discontinuation of treatment were side effects, which were mainly gastrointestinal symptoms. To improve the long-term outcome of patients with osteoporosis, further studies are needed to examine factors associated with bisphosphonates discontinuation and compliance. Newer strategies to promote longterm persistence are needed to improve bisphosphonate therapeutic effectiveness.
References
McClung MR (2000) Bisphosphonates in osteoporosis: recent clinical experience. Expert Opin Pharmacother 1:225–238
Bone HG, Hosking D, Devogelaer JP, Tucci JR, Emkey RD, Tonino RP et al (2004) Ten years’ experience with alendronate for osteoporosis in postmenopausal women. N Engl J Med 350:1189–1199
Gold DT, Alexander IM, Ettinger MP (2006) How can osteoporosis patients benefit more from their therapy? Adherence issues with bisphosphonate therapy. Ann Pharmacother 40:1143–1150
McCombs JS, Thiebaud P, McLaughlin-Miley C, Shi J (2004) Compliance with drug therapies for the treatment and prevention of osteoporosis. Maturitas 48:271–287
Papaioannou A, Ioannidis G, Adachi JD, Sebaldt RJ, Ferko N, Puglia M et al (2003) Adherence to bisphosphonates and hormone replacement therapy in a tertiary care setting of patients in the CANDOO database. Osteoporos Int 14:808–813
Emkey RD, Ettinger M (2006) Improving compliance and persistence with bisphosphonate therapy for osteoporosis. Am J Med 119:S18–S24
Weycker D, Macarios D, Edelsberg J, Oster G (2006) Compliance with drug therapy for postmenopausal osteoporosis. Osteoporos Int 17:1645–1652
Curtis JR, Westfall AO, Allison JJ, Freeman A, Saag KG (2006) Channeling and adherence with alendronate and risedronate among chronic glucocorticoid users. Osteoporos Int 17:1268–1274
Tosteson AN, Grove MR, Hammond CS, Moncur MM, Ray GT, Hebert GM et al (2003) Early discontinuation of treatment for osteoporosis. Am J Med 115:209–216
Rossini M, Bianchi G, Di Munno O, Giannini S, Minisola S, Sinigaglia L et al (2006) Determinants of adherence to osteoporosis treatment in clinical practice. Osteoporos Int 17:914–921
Cramer JA, Silverman S (2006) Persistence with bisphosphonate treatment for osteoporosis: finding the root of the problem. Am J Med 119:S12–S17
Cryer B, Bauer DC (2002) Oral bisphosphonates and upper gastrointestinal tract problems: what is the evidence? Mayo Clin Proc 77:1031–1043
Hamilton B, McCoy K, Taggart H (2003) Tolerability and compliance with risedronate in clinical practice. Osteoporos Int 14:259–262
Pickney CS, Arnason JA (2005) Correlation between patient recall of bone densitometry results and subsequent treatment adherence. Osteoporos Int 16:1156–1160
Curtis JR, Westfall AO, Allison JJ, Becker A, Casebeer L, Freeman A et al (2005) Longitudinal patterns in the prevention of osteoporosis in glucocorticoid-treated patients. Arthritis Rheum 52:2485–2494
Penning-van Beest FJ, Goettsch WG, Erkens JA, Herings RM (2006) Determinants of persistence with bisphosphonates: a study in women with postmenopausal osteoporosis. Clin Ther 28:236–242
Cranney A, Guyatt G, Griffith L, Wells G, Tugwell P, Rosen C (2002) Meta-analyses of therapies for postmenopausal osteoporosis. IX: summary of meta-analyses of therapies for postmenopausal osteoporosis. Endocr Rev 23:570–578
Fukunaga M, Kushida K, Kishimoto H, Shiraki M, Taketani Y, Minaguchi H et al (2002) A comparison of the effect of risedronate and etidronate on lumbar bone mineral density in Japanese patients with osteoporosis: a randomized controlled trial. Osteoporos Int 13:971–979
Mersfelder T, Armitstead JA, Ivey MF, Cedars M (1999) A medication use evaluation of alendronate: compliance with administration guidelines. Pharm Pract Manag Q 18:50–58
Tanaka I, Hayakawa K, Oshima H (2003) Tolerance of alendronate in patients with osteoporosis. Osteoporosis Jpn 11:252–255
Naito H (2006) The Japanese health-care system and reimbursement for dialysis. Perit Dial Int 26:155–161
Yoshida M, Takada T, Kawarada Y, Hirata K, Mayumi T, Sekimoto M et al (2006) Health insurance system and payments provided to patients for the management of severe acute pancreatitis in Japan. J Hepatobiliary Pancreat Surg 13:7–9
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ideguchi, H., Ohno, S., Hattori, H. et al. Persistence with bisphosphonate therapy including treatment courses with multiple sequential bisphosphonates in the real world. Osteoporos Int 18, 1421–1427 (2007). https://doi.org/10.1007/s00198-007-0406-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-007-0406-0