Abstract
Summary
Meaured spinal kyphosis, as a predictor of prevalent and incident vertebral deformity, was examined in older women (>70 years) and found to not have sufficient sensitivity or specificity to justify its use as a predictor of present or future vertebral deformity risk.
Introduction
Kyphosis may be attributable to vertebral deformity and was investigated as a clinical tool for predicting the presence and future risk of vertebral deformity.
Methods
Kyphosis was measured in 434 women aged 70 years or older and the kyphosis index (KI) calculated. Prevalent and incident vertebral deformities were assessed by morphometric X-ray absorptiometry (MXA). The predictive value of KI was examined.
Results
Severity of kyphosis was categorised by tertile of KI; 65% of anterior thoracic deformities occurred in the 33% of subjects in the highest (most kyphotic) tertile. Using this tertile as a predictor of anterior thoracic deformity, the probability for a positive test rose from 14% for the whole population to 28% and for a negative test the probability fell to 8%. For any spinal deformity the highest tertile of KI increased the probability of a positive test from 34% to 42% and reduced the probability for a negative test to 30%. The incidence of new deformities was 6% over 4 years; a high KI tertile did not increase the probability of any vertebral deformity.
Conclusions
Severe kyphosis does not increase the probability of detection of a prevalent or incident spinal deformity sufficiently to make it a useful method of selecting patients for further evaluation of spinal deformity.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Vertebral fractures, a serious complication of osteoporosis, go undiagnosed in over 50% of cases [1]. This is of concern because spinal fractures are associated with decreased quality of life [2] and increased mortality [3–5]. The occurrence of a vertebral fracture results in a marked increase in the risk of subsequent vertebral fractures in an individual [6]. Thus, simple clinical markers of the presence of vertebral fractures would be of considerable benefit in predicting further fracturing, reduced quality of life and increased mortality. In recent years, the outcomes of three large studies have suggested that a risk factor assessment may prove useful in detecting patients at high risk of fracture for further diagnostic testing [7–9]. A recent study found that women who were classified as hyperkyphotic (defined as requiring a block of 1.7 cm thick under the patients neck in order to achieve a neutral neck position when lying flat) had a 1.7-fold increase of future vertebral fracture risk [10]; however, no data on its clinical value using modern methods of assessing clinical utility using sensitivity and specificity were presented.
In this study, vertebral structure and its abnormal variation was assessed by a morphometric X-ray (MXA) method using dual energy X-ray absorptiometry (DXA). Assessment of vertebral deformity involves placement of points around the edge of the vertebral body, abnormal distances between these points define the presence of a deformity. This technique has been shown to detect vertebral deformities with reasonable precision in comparison with X-ray techniques [11, 12] and has some advantages and disadvantages compared with the clinical vertebral fracture end point. The advantages of the use of vertebral deformities is that they are determined by objective criteria concerning the shape of the vertebral body and do not require the patient to present with back pain, which occurs in only about half of patients with radiographically identified fracture [13]. Vertebral deformity is also associated with some functional limitations, independently of pain [14], and is predictive of future vertebral fracture [15]. A disadvantage is that the technique does not utilise all the shape data in making the diagnosis, as does radiographic assessment. In this study, thoracic curvature was assessed objectively using a previously reported flexicurve ruler method [16]. The validity and reliability of the flexicurve ruler method of kyphosis assessment in osteoporotic subjects has been compared with roentgenographic assessment and found to have close agreement [17].
Thus, the aim of this study was to evaluate the prevalence of kyphosis using a flexicurve ruler in a population-based sample of elderly women and determine its predictive ability for prevalent and incident vertebral deformities. It was hypothesised that if an objective measure of kyphosis proved useful in prediction of deformity then a clinical algorithm for detection of patients at increased risk of prevalent or incident fractures could be developed.
Materials and methods
Four hundred and thirty-four patients were recruited at random as part of a large population-based prospective study of women aged between 70 and 82, mean age 75 ± 3 years, living at home [18]. Demographic data, height and weight were collected by standard measures. Informed consent was obtained and the Human Rights Committee of the University of Western Australia approved the study.
Kyphosis index
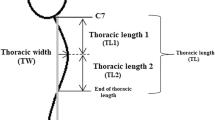
Thoracic curvature was measured using a flexicurve ruler [16]. The subjects were asked to stand adopting their normal posture and the ruler was pressed against their back with the top end placed on the seventh cervical spine in the midline. The ruler was moulded into the shape of the subject’s spine in the midline to the level of the lumbosacral joint. The flexicurve ruler was removed and the shape of the spine was then traced onto paper and analysed as shown in Fig. 1. The kyphosis index (KI) was calculated as the ratio of B to E, multiplied by 100. The larger the KI, the more marked the kyphosis. The coefficient of variation for KI of 6.6%, as determined from duplicate measurements performed in 20 randomly selected subjects from the cohort reported in this study by a group of trained assessors on the same day, was half that reported by others [19]. The validity and reliability of the flexicurve ruler method of kyphosis assessment in osteoporotic subjects has been compared with roentgenographic assessment and found to have close agreement [17].
Morphometric spinal deformities
The reference data for the ascertainment of spinal deformities was determined from measurement of MXA data of 120 randomly selected patients of the same age as the study patients and recruited from the same population but who did not have the KI measured and were thus not available to be part of this study. The patients used for the reference data did not differ in age, weight or height from the study subjects. Single energy high-definition lateral MXA scans of vertebra T4-L4 were performed using a Hologic QDR 4500A. The patient was positioned longitudinally in the centre of the scan table using the positioning laser. A PA centreline scan was then performed, which was used by the machine to maintain a constant distance between the spine and the X-ray tube during acquisition of the lateral image, therefore correcting for the magnification effect of the fan beam. The centreline scan also sets the start point for the subsequent lateral scan.
For each vertebra, a single operator placed six reference markers at the corners and in the middle of the upper and lower surface of each vertebral image. The height was measured as the distance between the markers at the edge of the superior and inferior endplates of that vertebra as described by the operator’s manual. The mean coefficient of variation in MXA measurements of the anterior, central and posterior heights was determined for the single operator who undertook the assessment of all the MXA scans by undertaking point placement from L4 to T12 in duplicate measurements from 30 subjects randomly selected from the study cohort. The mean coefficients of variation were 4.5% for posterior height measurements, 4.5% for central height measurements and 5.3% for anterior height measurements.
As described by McCloskey et al. [20], the ratio of the anterior to posterior height, the central to posterior height and the posterior to the predicted posterior height was calculated for the reference data and expressed as the 5% trimmed mean and SD (Table 1). The predicted posterior height was calculated from the two adjacent vertebrae above and below the vertebra of interest, or for T4 the four vertebrae below and for L4 the four vertebrae above. The posterior/predicted posterior ratio was calculated from the measured compared with the predicted height for that vertebra.
Prevalent wedge vertebral deformities were defined as both an anterior/posterior height ratio and anterior/posterior predicted height ratio 3 SDs below the normative mean anterior to posterior value at that level; central deformities were defined as both a central/posterior height ratio and central/posterior predicted height ratio three SD below the normative value at that level; and prevalent crush vertebral deformities were defined as both a posterior/predicted posterior height ratio 3 SDs below the normative value at that level and anterior/posterior predicted height ratio 3 SDs above the normative value at that level for that measurement in our reference population [20]. Incident vertebral deformities over the subsequent 4 years were defined as a reduction in the posterior, mid or anterior vertebral height of 20% or more from baseline in MXA scans performed by the same operator using the same method as for the baseline scans.
Statistical analyses
All statistical analyses were performed using SPSS Windows Version 11.5 (SPSS, Chicago, USA). These data were examined for normal distribution by the Kolmogorov-Smirnov goodness-of-fit test. The KI was categorised into tertiles. For the normally distributed variables mean±SD were reported. Frequency of thoracic spinal deformities was calculated. Logistic regression analyses were used to examine the relationship between KI and spinal deformities determined by MXA after adjustment for confounding factors. A receiver operator curve (ROC) analysis was used to determine the sensitivity of KI as a predictor of one or more anterior deformities. The predictive value of a positive test was calculated as the percentage of individuals who had an anterior vertebral deformity and were above the selected KI index indicated. The predictive value of a negative test was calculated as the percentage of individuals who did not have an anterior vertebral deformity and were below the selected KI index indicated. The likelihood ratio for a positive test was calculated as the sensitivity (true positive/false positive) rate. The likelihood ratio for a negative test was calculated as the specificity (true negative/false negative) rate. All statistical tests were two tailed. Probability values less than 5% were considered significant.
Results
Demography of vertebral deformity and KI
As described in the methods section, the normative data from which the presence of vertebral deformities was calculated are shown in Table 1. The demographic variables of the 434 patients recruited at random as part of a large population-based prospective study of women living at home are shown in Table 2. Overall, 34% had sustained a lumbar or thoracic vertebral deformity between T4 and L4, 22% had sustained one vertebral deformity and 12% had sustained more than one vertebral deformity. The frequency of deformities was bimodal, with peaks at T8 and T12 and at least one anterior, crush or central deformity between T4 and L4 was present in 18%, 17% and 6% of the population, respectively (Fig. 2). Thoracic deformities from T4 to T12 occurred in 32% of individuals of the whole group; anterior deformities, crush deformities and central deformities were present in 14%, 13%, and 5% of the subjects, respectively. Six percent of patients with one thoracic anterior deformity also had other deformed vertebrae in the thoracic spine approximately equally distributed between crush, central or other anterior deformities. To examine the diagnostic utility of kyphosis assessment the patients were grouped into three tertiles of KI (Table 2). Subjects in tertile three of the KI were significantly shorter than those in KI tertile 2. There was no difference in age or years since menopause between the three groups; however, those in tertile 2 and tertile 3 had a significantly higher body weight than those in tertile 1.
Thoracic deformities
The percentage of thoracic anterior deformities increased with KI tertile; however, there was no difference in thoracic central or crush deformities between the groups (Fig. 3). Logistic regression with thoracic anterior deformity as the dependent variable was used to determine the odds of having a thoracic anterior deformity with increasing KI. The odds of an anterior deformity were three- (95% CI 1–7) and nine-times (95% CI 4–22) greater in the second and third tertiles, respectively, compared with those in the first tertile after adjustment for age. Only those in the highest tertile of KI had more than one thoracic anterior deformity (data not shown).
a, b Proportion of subjects with a central, crush, anterior wedge, or any MXA deformity type within each kyphosis tertile group. The proportion of deformities across the tertile groups for each fracture type, or any fracture type, were compared using the χ2 test; ***P < 0.001, **P < 0.005, *P < 0.01
The diagnostic utility of the KI as a predictor of thoracic anterior deformities was further evaluated using ROC analysis and the calculation of appropriate summary statistics (Fig. 4a, Table 3). Using a KI cut-off of 15.5 (tertile 3), the probability of deformity was 28%. The probability of deformity for individuals below the cut-off fell to 8%. Using a more conservative KI cut-off of 12.8 (tertiles 2 and 3), the probability of anterior wedge deformity above the KI cut-off of 15.5 was 18% and below the cut-off was 5%.
a ROC demonstrating the value of the KI in predicting anterior vertebral deformities between T4 and T12; the arrows indicate the sensitivity and specificity of KIs of 15.5 and 12.8. b ROC demonstrating the value of the KI in predicting any type of vertebral deformity between L4 and T12; the arrows indicate the sensitivity and specificity of KIs of 15.5 and 12.8
Thoracic and lumbar deformities
The percentage of deformities in both the lumbar and thoracic spine within each KI tertile are shown in Fig. 3. As KI tertile increased so did the proportion of anterior and central deformities. ROC analysis was used to determine the sensitivity of the KI as a predictor of any spinal lumbar or thoracic deformity (Fig. 4b, Table 3). At a KI of 15.5 or greater (tertile 3), the sensitivity for the detection of any spinal deformity was 42% and the specificity was 70%. The probability of deformity above the KI cut-off was 42% and below the cut-off was 30%. Using a more conservative KI cut-off of 12.8 (tertiles 2 and 3), the sensitivity was 77% and the specificity was 28%. The probability of any deformity above the KI cut-off 12.8 was 36% and below this cut-off was 30%.
Incident vertebral deformities
MXA data was available in 349 subjects four years after the first measurement. Of these 349 subjects, 6.6% (n = 23) sustained one or more new MXA-defined vertebral deformities in previously un-deformed vertebrae of the thoracic or lumbar spine. The deformities consisted of nine crush, one central and 22 anterior deformities. There was no association between the KI and the occurrence of a new MXA-defined vertebral deformity (KI tertile 1: 6 (5.5%); KI tertile 2: 9 (8.2%); KI tertile 3: 8 (6.5%); χ2 = 0.57, P = 0.77).
Discussion
In this study, the proportion of subjects with one or more vertebral deformities, as determined by MXA, was 34%. This should be compared with radiographic morphometric studies using a 3-SD decision threshold criterion in which a vertebral deformity prevalence of 46% in 80- to 90-year-olds and 21% in a somewhat younger age group was reported [21, 22]. The distribution of vertebral deformities along the spine was similar to that reported by both Eastell et al. [21] and Melton et al. [22], verifying that our analysis of vertebral deformities using MXA produced similar results to studies that used roentograms. A previous report from our centre demonstrated that MXA produced similar results to those produced by radiographic morphometry when evaluated with respect to spinal heights measured ex vivo [23]. The distribution of deformities across the spine in our study compares closely with the distribution of vertebral deformities across the spine previously reported by Melton et al. [24], who demonstrated that deformities were most common in the mid-thoracic and thoraco-lumbar junction, similar to our own study. Furthermore, similar to what was observed in this study, Melton et al. [24] reported equal prevalence of anterior and crush fractures with central fractures about half as prevalent perhaps related to the hierarchical algorithm of selecting for crush, then anterior, then central deformity as used in this study.
The results obtained from this study show that increasing kyphosis is primarily related to an increased risk of thoracic anterior deformities, but not other sorts of spinal deformities, although in the whole spine data there was a weak association with central collapse. Thus, clinical kyphosis detection with or without the use of the KI has the potential to detect some individuals who may not otherwise be considered for treatment. When analysed using odds ratio, the performance characteristics of the KI showed that an individual with a KI above 15.4 had nine-times the risk of having a thoracic anterior deformity compared with those having a KI below 12.8. However, using ROC analysis in absolute terms the risk only rose from 14% to 28% if positive and fell to 8% if negative, values that are not particularly useful in clinical diagnostic practice.
When compared against patients with any spinal deformity, the performance characteristics of the KI were also poor because the post-test probability for a positive test only rose to 42% from 34% and only fell to 30% for a negative test. Moreover, the KI was of no predictive value for determining the risk of future vertebral fracture, determined as a 20% reduction in vertebral height using MXA. While it is true that these calculations are limited to the population of elderly postmenopausal women studied, this population was selected because of the relatively high prevalence of vertebral deformity. In other populations with lower prevalence of fracture, the performance characteristics of the KI are likely to be lower. Therefore, the assessment of the KI, either by measurement or by clinical assessment, is of only limited value in determining a patient’s risk of having a vertebral deformity and is of no value in determining that individual’s risk of future vertebral fracture. Spine deformities can only be reliably diagnosed using X-ray technology or vertebral fracture assessment using DXA [17].
References
Riggs BL, Melton LJ 3rd (1986) Involutional osteoporosis. N Engl J Med 314:1676–1686
Hall SE, Criddle RA, Comito TL, Prince RL (1999) A case-control study of quality of life and funcational impairment in women with long-standing vertebral osteoporotic fracture. Osteoporosis Int 9:508–515
Kado DM, Browner WS, Palermo L, Nevitt MC, Genant HK, Cummings SR (1999) Vertebral fractures and mortality in older women: a prospective study. Study of Osteoporotic Fractures Research Group. Arch Intern Med 159:1215–1220
Cooper C, Atkinson EJ, Jacobsen SJ, O’Fallon WM, Melton LJ 3rd (1993) Population-based study of survival after osteoporotic fractures. Am J Epidemiol 137:1001–1005
Center JR, Nguyen TV, Schneider D, Sambrook PN, Eisman JA (1999) Mortality after all major types of osteoporotic fracture in men and women: an observational study. Lancet 353:878–882
Doherty DA, Sanders KM, Kotowicz MA, Prince RL (2001) Lifetime and five-year age-specific risks of first and subsequent osteoporotic fractures in postmenopausal women. Osteoporos Int 12:16–23
Sornay-Rendu E, Munoz F, Garnero P, Duboeuf F, Delmas PD (2005) Identification of osteopenic women at high risk of fracture: the OFELY study. J Bone Miner Res 20:1813–1819
Kaptoge S, Armbrecht G, Felsenberg D, Lunt M, Weber K, Boonen S, Jajic I, Stepan JJ, Banzer D, Reisinger W, Janott J, Kragl G, Scheidt-Nave C, Felsch B, Matthis C, Raspe HH, Lyritis G, Poor G, Nuti R, Miazgowski T, Hoszowski K, Armas JB, Vaz AL, Benevolenskaya LI, Masaryk P, Cannata JB, Johnell O, Reid DM, Bhalla A, Woolf AD, Todd CJ, Cooper C, Eastell R, Kanis JA, O’Neill TW, Silman AJ, Reeve J (2006) Whom to treat? The contribution of vertebral X-rays to risk-based algorithms for fracture prediction. Results from the European Prospective Osteoporosis Study. Osteoporos Int 17:1369–1381
Holmberg AH, Johnell O, Nilsson PM, Nilsson J, Berglund G, Akesson K (2006) Risk factors for fragility fracture in middle age. A prospective population-based study of 33,000 men and women. Osteoporos Int 17:1065–1077
Huang MH, Barrett-Connor E, Greendale GA, Kado DM (2006) Hyperkyphotic posture and risk of future osteoporotic fractures: the Rancho Bernardo study. J Bone Miner Res 21:419–423
Ferrar L, Jiang G, Barrington NA, Eastell R (2000) Identification of vertebral deformities in women: comparison of radiological assessment and quantitative morphometry using morphometric radiography and morphometric X-ray absorptiometry. J Bone Miner Res 15:575–585
Rea JA, Chen MB, Li J, Blake GM, Steiger P, Genant HK, Fogelman I (2000) Morphometric X-ray absorptiometry and morphometric radiography of the spine: a comparison of prevalent vertebral deformity identification. J Bone Miner Res 15:564–574
Ross PD (1997) Clinical consequences of vertebral fractures. Am J Med 103:30S–42S; discussion 42S–43S
Edmond SL, Kiel DP, Samelson EJ, Kelly-Hayes M, Felson DT (2005) Vertebral deformity, back symptoms, and functional limitations among older women: the Framingham Study. Osteoporos Int 16:1086–1095
Crans GG, Genant HK, Krege JH (2005) Prognostic utility of a semiquantitative spinal deformity index. Bone 37:175–179
Milne JS, Lauder IJ (1976) The relationship of kyphosis to the shape of vertebral bodies. Ann Hum Biol 3:173–179
Lundon KM, Li AM, Bibershtein S (1998) Interrater and intrarater reliability in the measurement of kyphosis in postmenopausal women with osteoporosis. Spine 23:1978–1985
Bruce DG, Devine A, Prince RL (2002) Recreational physical activity levels in healthy older women: the importance of fear of falling. J Am Geriatr Soc 50:84–89
Ettinger B, Black DM, Palermo L, Nevitt MC, Melnikoff S, Cummings SR (1994) Kyphosis in older women and its relation to back pain, disability and osteopenia: the study of osteoporotic fractures. Osteoporos Int 4:55–60
McCloskey EV, Spector TD, Eyres KS, Fern ED, O’Rourke N, Vasikaran S, Kanis JA (1993) The assessment of vertebral deformity: a method for use in population studies and clinical trials. Osteoporos Int 3:138–147
Eastell R, Cedel SL, Wahner HW, Riggs BL, Melton LJ 3rd (1991) Classification of vertebral fractures. J Bone Miner Res 6:207–215
Melton LJ, Kan SH, Frye MA, Wahner HW, O’Fallon WM, Riggs BL (1989) Epidemiology of vertebral fractures in women. Am J Epidemiol 129:1000–1011
Edmondston SJ, Price RI, Valente B, Singer P (1999) Measurement of vertebral body heights: ex vivo comparisons between morphometric X-ray absorptiometry, morphometric radiography and direct measurements. Osteoporos Int 10:7–13
Melton LJ, Lane AW, Cooper C, Eastell R, O’Fallon WM, Riggs BL (1993) Prevalence and incidence of vertebral deformities. Osteoporosis Int 3:113–119
Acknowledgments
Prof. K. Singer suggested the use of the flexible rule to measure kyphosis. This study was supported by research grants from the Healthway Health Promotion Foundation of Western Australia, the Australasian Menopause Society and the National Health and Medical Research Council of Australia (project grant 254627).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Prince, R.L., Devine, A. & Dick, I.M. The clinical utility of measured kyphosis as a predictor of the presence of vertebral deformities. Osteoporos Int 18, 621–627 (2007). https://doi.org/10.1007/s00198-006-0289-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-006-0289-5