Abstract
Generalized osteopenia and spinal deformity occur concomitantly in adolescent idiopathic scoliosis (AIS) during the peripubertal period. No large-scale study has been performed to reveal the link between scoliotic deformity and bone-mineral status in AIS. In a cross-sectional study, the extent of scoliotic-curve severity in relation to bone-mineral status was examined for 619 AIS girls and compared with those of 300 healthy non-AIS counterparts aged 11–16 years. Curve severity was categorized into a moderate (10–39°) and a severe group (≥40°) based on Cobb angle. Anthropometric parameters, bone mineral-density (BMD) and bone mineral-content (BMC) of lumbar spine, proximal femur and distal tibia were determined by dual-energy X-ray absorptiometry and peripheral QCT. Differences in anthropometric parameters and bone mass among control and the AIS-moderate and AIS-severe groups were tested by one-way ANOVA. Association between Cobb angle and bone mass was determined by univariate and multivariate analyses. Mean Cobb angle of the moderate and severe groups were 25±6.3° and 50.2±11.3°, respectively. Arm span and leg length among the moderate and severe AIS subjects were almost all longer than for the controls from age 13 years. Age-adjusted arm span and leg length were significantly correlated with curve severity ( p <0.015). Starting from age 13 years, most axial and peripheral BMD and BMC of the moderate or severe AIS group was significantly lower than for the controls ( p <0.029). Age-adjusted Cobb angle was inversely correlated with BMD and BMC of the distal tibia and lumbar spine among AIS subjects ( p ≤0.042). The proportion of osteopenic AIS girls in the severe group was significantly higher than that in the moderate group ( p ≤0.033). Multivariate analysis indicated that Cobb angle was inversely and independently associated with axial and peripheral BMD and BMC ( p ≤0.042). To conclude, curve severity was an inverse and independent associated factor on bone mineral mass of AIS during peripuberty. The study implied that prevention of osteopenia could be as important as controlling spinal progression in the management of AIS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Manifestation of generalized osteopenia during the peripubertal period in patients with adolescent idiopathic scoliosis (AIS) is well documented [1–7]. Approximately 25% of AIS patients followed up at our scoliosis clinic were osteopenic, with BMD z -scores less than −1 SD [4,5]. Osteopenia and spinal deformity occur concomitantly in AIS during the peripubertal period [4,5]. In our scoliosis clinic, rapid progression of spinal deformity may occur in a proportion of AIS patients at 10–14 years of age. During rapid peripubertal growth, an increasing body weight may exert a biomechanical force on the deformed osteopenic spine, thereby increasing the risk of curve progression [8–10]. However, there has been no large-scale study to reveal the relationship between spinal deformity and bone mineral status in AIS. The aim of the present study was to examine the extent of spinal curve severity in relation to bone mineral status in AIS girls during the peripubertal period.
Materials and methods
Subjects
Newly diagnosed AIS girls aged between 11–16 years and attending our scoliosis clinic were invited to participate in the study. Diagnosis of AIS was confirmed by clinical and X-ray examination with the Cobb’s angle equal to or greater than 10°. Patients receiving any forms of prior treatment for scoliosis including bracing were excluded from the study. Healthy girls of similar age range were recruited randomly from three local schools to serve as controls. All normal controls were also physically examined to rule out any form of scoliosis before entering into the study. Subjects with history of congenital deformities, neuromuscular diseases, endocrine diseases, skeletal dysplasia, connective tissue abnormalities or mental retardation were also excluded from the study. Informed consent was obtained from parents. Clearance of ethical approval was obtained from the Clinical Research Ethics Committee before subject enrollment.
Evaluation of scoliotic curvature
Scoliotic curvature was evaluated by measuring Cobb’s angle at the coronal plane of the whole spine on the standard radiographic film. For patients with double curves, Cobb’s angle of the greatest curve was used for reference [11]. Curve severity of AIS was classified into two groups: moderate group (Cobb angle 10–39°) and severe group (Cobb angle ≥40°) according to the conventional practice of classification of curve severity at our scoliosis clinic.
Anthropometric parameters
Anthropometric parameters including weight, height, arm span and leg length were measured using standard techniques based on our previous studies [12–13]. Body mass index (BMI) was calculated by dividing weight (kg) by height squared (m2). For AIS patients, corrected height was derived with Bjure’s formula (log y =0.011 x −0.177; where y is the loss of trunk height (cm) due to the deformed spine, and x is the greatest Cobb angle of the primary curve) [14].
Evaluation of bone mineral status
Dual-energy X-ray absorptiometry
Femoral neck BMC (FNBMC) and BMD (FNBMD) of the non-dominant proximal femur, and lumbar spinal BMC (LSBMC) and BMD (LSBMD) in anteroposterior position were measured by dual-energy X-ray absorptiometry (DXA) (XR-36, Norland, Fort Atkinson, WI, USA). The rotated scoliotic spine of AIS patients may present difficulties in measuring the spinal BMD reliably. To minimize this problem, the spine was pre-scanned once; a reference line was drawn to join the highest points of the iliac crests, which usually passes between the third and fourth lumbar spinal processes. On that reference line a rectangle was erected to include L2–L4, and this was defined as the scan area [5,7]. Furthermore, our previous study has shown that the projected spinal bone area varies with the degree of rotational deformity of the scoliotic spine, and this will result in underestimation of the lumbar spinal BMD [6]. Hence, we also presented results of lumbar spinal BMC (LSBMC) adjusted for projected spinal bone area and body size in the present study. To measure the femoral neck in anterior-posterior position, a foot support was used to maintain a 20° inward rotation of the legs to compensate for femoral neck anteversion. It has been reported that femoral neck BMD was lower at the hip at the convex side of the major primary curve when compared with that of the hip at the concave side of the major primary curve, due to a shift of the body’s center of gravity towards the opposite side of curve convexity [15]. Hence, we also compared convex and concave FNBMD of the bilateral hip in a sample of AIS patients and compared them with those of controls to see if BMD on both sides of the hip were any different from those of the controls. Quality assurance was performed daily by using the standard phantom provided by the manufacturer. In the present study, the in vivo precision errors in measuring BMC and BMD at the lumbar spine and proximal femur of the subjects were 1.1–3.7% for our study population. Technical details of DXA measurement for AIS and non-AIS girls have been described in our previous studies [3,5].
Peripheral quantitative computed tomography (pQCT)
Volumetric BMD (vBMD) of the non-dominant distal tibiae was measured by pQCT (Densiscan 2000, Scanco Medical, Switzerland). During CT scanning, the lower leg of the subjects was positioned in a selected radiolucent cast suitable for the subject. After displaying an anteroposterior projectional scout view, a reference line was set vertical to the long axis of the lower leg and placed on the middle point of the endplate of the distal tibia. A four-slice program with slice thickness of 1 mm each and the interval between the slices of 1.5 mm was used for distal tibia as described in our previous study [5]. Measurement values were averaged from the four slices for data evaluation. The average vBMD of the trabecular bone in a core volume (central 50% of the total bone area) of the distal tibia (TtBMD) and integral vBMD of both the cortical and trabecular bone within the total bone volume of the distal tibia (TiBMD) were evaluated. In addition, the cross-sectional area of the scanned distal tibia (TiCSA) was also obtained from the average of the four-slice program, whereas the integral trabecular and cortical BMC of the distal tibia (TiBMC) was determined by multiplying TiBMD and TiCSA. The coefficients of variation (CV) of repeated measurements at the distal tibia (TtBMD, TiBMD and TiCSA) were 0.99%, 0.82% and 1.41%, respectively, for our study population. Technical details on using pQCT for vBMD measurement are found elsewhere [16–18].
Statistics
The spread of the data was tested for normality. Data were summarized either in mean±SD or median and interquartile range (IQR). One-way analysis of variance (ANOVA) test followed by post hoc Bonferroni multiple comparison were employed to test any significant difference among the three groups, i.e., the control group, moderate and severe AIS groups. Age-adjusted BMD and BMC in association with curve severity were determined by using Pearson correlation analysis. Age-adjusted BMD z -scores of AIS were determined from the mean BMD of the age-matched control girls. BMD z -score ≤−1 SD was classified as osteopenia, while BMD z -score >−1 SD was classified as normal BMD status [4,5]. Chi-square test was used to compare the percentage of AIS subjects with normal BMD status and osteopenia based on BMD z -score between the moderate and severe AIS groups. Linear multiple regression analysis was used to determine the proportional effects of Cobb’s angle, anthropometric parameters and age on the variation of BMD. Level of significance was set at p <0.05. SPSS version 11 (SPSS, Chicago, IL, USA) was used for statistical analysis.
Results
The study included 619 AIS girls with curve severity ≥10° and 300 healthy non-AIS girls, at age 11–16 years. All the subjects fulfilled the selection criteria. A majority of the curve types of the studied patients were thoracic (67.1%); about 23% were thoracolumbar and 9.9% were lumbar. Table 1 shows the age distribution of the control group, moderate and severe AIS groups. Cobb’s angles (mean±SD) of the moderate group ( n =532) and severe ( n =87) group were 25±6.3° and 50.2±11.3°, respectively. A majority of the newly recruited AIS belong to the moderate group of curve severity, which might be related to the universal scoliosis screening program for school children in Hong Kong.
Table 2 compares anthropometric parameters among the three groups by age. Body weight was significantly different among the three groups at ≤12 years old ( p =0.017), with body weight of the moderate group significantly lower than that of the controls ( p <0.05). There were also significant differences in BMI among the three groups at ≤12 years, 13 years and ≥15 years ( p ≤0.008), with BMI of the moderate group significantly lower than that of the controls at ≥12 years and ≥15 years ( p <0.05); whereas, at age 13 years, BMI of the severe group was significantly lower than that of the control group ( p <0.05). At age 13 years, corrected height, arm span and leg length were significantly different among the three groups ( p ≤0.026), with the three body segmental lengths of the moderate group significantly longer than those of the controls ( p <0.05). At age 14 years, corrected height and arm span were significantly different among the three groups ( p ≤0.009), with corrected height ( p <0.05) and arm span ( p <0.01) of the moderate group longer than those of the controls; whereas, arm span of the severe group was also longer than that of the controls ( p <0.01). At age ≥15 years, corrected height and arm span were significantly different among the three groups ( p ≤0.001), with the three body segmental lengths of both the moderate and severe groups significantly longer than those of the controls ( p <0.05). No significant differences in weight, BMI and body segmental lengths were found between the moderate and severe groups at different ages, which may be attributable to the small number of newly recruited AIS subjects who presented with severe scoliosis. Fig. 1 depicts the percentage differences in corrected height and arm span of the moderate and severe groups with reference to the control group. The differentials of corrected height and arm span in the severe groups were markedly higher than those of the moderate groups, although the differences did not reach significant levels. That might be due to the sample size in the severe AIS group. It seems that the older the age, the more discrepancies in body segmental lengths between AIS and non-AIS girls increased. Age-adjusted arm span and leg length were significantly correlated with curve severity ( r =0.099, p =0.015 and r =0.126, p =0.002, respectively). However, curve severity was not correlated with weight, BMI or corrected height ( p >0.05) (Table 3).
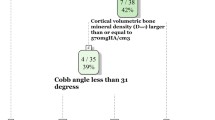
Table 4 summarizes the comparisons of BMD and BMC among the control group, moderate and severe AIS groups by age. Volumetric BMD and BMC of the distal tibia were all significantly different among the control, moderate and severe groups at all ages ( p ≤0.006) apart from TiBMD at age ≤12 years. From age 13 years onwards, almost all the distal tibial volumetric BMD and BMC of both the moderate and severe groups were significantly lower than those of the controls ( p <0.05). With regard to areal BMD and BMC, there were significant differences in LSBMD among the three groups at all ages ( p ≤0.046). LSBMD levels of the moderate and severe groups were almost all significantly lower than those of the controls at all ages ( p <0.05). LSBMC was significantly different among the control, moderate and severe groups at age ≥15 years ( p <0.006), with LSBMC of the moderate group significantly lower than that of the control group ( p <0.01). FNBMD and FNBMC were significantly different among the three groups at age 13 years and ≥15 years ( p ≤0.029). At age ≥15 years, FNBMD and FNBMC of the moderate and severe groups were almost all lower than those of the controls ( p <0.01). Table 3 shows the correlation between curve severity and adjusted BMD and BMC. There was inverse correlation between adjusted volumetric BMD and BMC of the distal tibia ( r =−0.083 to −0.115, p ≤0.042). There was also inverse correlation between adjusted LSBMC and curve severity ( r =0.106, p =0.009). It seems that the higher the Cobb’s angle, the lower the volumetric and areal BMD and BMC in the AIS girls. Further analysis was attempted to reveal if there was any significant difference in the proportion of osteopenic AIS girls between the moderate and severe AIS groups. BMD z -score of TTBMD, TiBMD, LSBMD and FNBMD of AIS subjects in the moderate and severe groups were compared by chi-square test. There was a significantly higher percentage of osteopenic AIS girls in the severe group than in the moderate group with respect to volumetric BMD (TtBMD, p =0.033; TiBMD, p =0.002) (Table 5).
Table 6 summarizes results of linear multivariate analysis including Cobb’s angle, age, weight, leg length and respective scanned bone area (bone size) as independent variables to explain the variations of axial and peripheral BMD and BMC. Leg length was selected to be included in multivariate analysis, because it was more significant than arm span or corrected height to associate with BMD. In each of the six regression models in Table 6, Cobb’s angle gave a significant but negative unstandardized coefficient (B), indicating that spinal deformity in AIS patients was independently and inversely associated with the variation of BMD after controlling for potential confounders ( p ≤0.042). Age and weight in the regression models were independently and positively associated with BMD and BMC at the six skeletal sites ( p <0.001). Leg length was negatively and significantly associated with BMD and BMC ( p <0.001), except for the femoral neck region, implying that the longer the long bone, the lower the BMD. The R-squares in these BMD models were sufficiently large, ranging from 28–77%. In summary, multivariate analysis revealed that after controlling for potential confounding factors, spinal deformity in AIS was inversely associated with axial and peripheral BMD and BMC.
Since the projected spinal bone area varies with the degree of rotational deformity of the deformed spine, this may result in underestimation of the lumbar spinal BMD [4]. Hence, further analysis was attempted to examine whether LSBMC levels of the moderate and severe patients were any different from those for the controls of similar age. Bone-area-adjusted LSBMC (natural log transformed due to unequal variance) was compared among the controls, moderate and severe AIS subjects by using univariate analysis of covariance (ANCOVA). Results showed that the adjusted LSBMC of the moderate and severe AIS subjects was still significantly lower than that of the controls of similar age (Table 7). The results were in line with those of LSBMD. In fact, after adjusting for the covariates of age, weight, leg length and bone area, curve severity still inversely and independently predicted the LSBMC (Table 6).
On the other hand, femoral BMD was found to be lower at the hip of the convex side of the major primary curve when compared with that of the hip at the concave side of the major primary curve in AIS subjects [15]. Hence, the effect of scoliotic curve convexity on FNBMD at bilateral hips of AIS subjects was further examined by analyzing bilateral FNBMD data from 318 patients aged 11–16 years in the present study. FNBMD at the non-dominant femur of AIS subjects had been found to be significantly different from that of controls at age 13 years and 15 years (Table 8). Results from further analysis found that within these 318 patients, convex FNBMD was significantly lower than concave FNBMD (0.743±0.006 g/cm2 vs 0.748±0.006 g/cm2, p =0.013). Furthermore, by one-way ANOVA, there were significant differences in convex and concave FNBMD among the controls, AIS moderate and severe groups at 15 years of age (Table 8). Post hoc Bonferroni multiple comparison showed that convex FNBMD of moderate and severe AIS subjects at age 15 years was significantly lower than that of controls, and that concave FNBMD of the moderate group ( p <0.05) was also significantly lower than that of controls ( p =0.01). Whereas concave FNBMD of the severe group was markedly lower than that of controls ( p =0.097), such a marginal insignificance might be due to the small sample size in the severe group ( n =7) (Table 8). On the other hand, at age 13 years, the magnitude of convex and concave FNBMD among the moderate and severe groups was markedly lower than that of the controls, although the difference was not statistically significant.
Table 9 depicts regression equations to predict the variation of axial and peripheral BMD and BMC of AIS subjects aged 11–16 years. These equations were derived from the multiple regression models in Table 6.
Discussion
This large-scale cross-sectional study revealed for the first time that there was a significant inverse relationship between age-adjusted spinal deformity and bone mineral status in AIS girls in the peripubertal period. Further analysis by using multivariate models confirmed that Cobb’s angle was still independently and inversely associated with the variation of axial and peripheral BMD and BMC after adjusting for known covariates, namely, age, body size and bone size. Hence, a longitudinal follow-up study will be necessary to confirm the relationship between curve severity and bone mineral status as found in the present cross-sectional study.
Axial and peripheral BMD and BMC of the moderate and severe AIS groups from age 13 years onwards were found to be virtually all significantly lower than those of the controls. The results agreed with our latest study of a group of AIS girls with mild to moderate curve severity (mean Cobb’s angle at 26.3±7.9°, 95% confidence interval [CI]: 10.5–42.1°) [7]. Similarly, age-adjusted Cobb’s angle of the moderate to severe AIS groups was significantly correlated with arm span and leg length in AIS girls, which was also consistent with results from our recent study in AIS girls with mild to moderate curve severity (mean Cobb’s angle at 26.3±7.9°) [11]. The prevalence of osteopenia in the AIS moderate group (25.3–29.9%) based on axial and peripheral BMD sites was found to be similar to our earlier report (21–29%) [5]. However, in the present study, up to 47% of AIS girls in the severe group were found to be osteopenic, which was drastically higher than those in the moderate group.
Although the rotated scoliotic spine may lead to underestimation of BMD measured at the lumbar spine, by analyzing LSBMC of AIS girls, the results showed that, similar to LSBMD, LSBMC of AIS patients in the current study was also significantly lower than that of the controls of similar age after adjusting for body size and bone size. On the other hand, by comparing convex FNBMD and concave FNBMD to those of the controls, although convex FNBMD was significantly lower than concave FNBMD in AIS patients, both convex and concave FNBMD of AIS patients were significantly lower than those of the controls at 15 years of age. In addition, both convex and concave FNBMD of AIS subjects were markedly lower than those of controls at age 13 years. Hence, FNBMD at either side of the hip of AIS patients in the present study was lower than that of the controls of similar age.
In 1995, a universal screening program for scoliosis was introduced to primary and secondary school students in Hong Kong. The prevalence rate of AIS has increased from 2.7% in 1998 to 4% in 2003 [19–20]. Children found to have abnormal spinal curvature are referred to hospital orthopaedic clinics for specialist management. Our scoliosis clinic is the largest tertiary referral center for scoliosis in Hong Kong; more than 1,000 new cases of AIS are seen each year. A majority of the new patients present with moderate scoliosis, with Cobb’s angle of the spine of between 20–39°. The small number of newly diagnosed AIS girls presenting with severe curve severity when enrolled in our study could be attributable to the ongoing health screen program in Hong Kong. About 10% of these moderate cases may progress to spinal deformity. The current clinical management of AIS patients is aimed at preventing or slowing spinal progression. No definitive treatment can be offered for minor curves. For major or rapidly progressive curves, extensive surgical correction with instrumentation and permanent fusion is required.
Although osteopenia is rare in healthy adolescents, significantly lower BMD measured at various skeletal sites of AIS girls as compared with that of age-matched healthy controls is well documented [3–5]. In our earlier longitudinal study on BMD changes involving a group of 64 AIS girls aged 11–16 years, with a mean follow-up period 3.8 years, we found that AIS girls with low BMD at baseline had persistently lower BMD throughout the follow-up period, until plateauing off [4]. Nutrition, in particular calcium intake, plays an important role in the maintenance of bone integrity and, thereby, optimizing bone health from childhood to adulthood [21–24]. In our recent reports, calcium intake of peripubertal AIS girls in Hong Kong was less than 400 mg/day, which is insufficient to meet the requirement for optimal bone mineralization. We also found that the lower the calcium intake the lower the BMD of AIS girls [7,25]. Therefore, a low calcium intake may jeopardize the integrity of BMD and hence bone strength of AIS girls [7,35].
There are important research and clinical implications based on the findings of the present study. Firstly, the progression of spinal deformity and poor bone mineral status seem to occur at the same time during peripuberty. The immediate clinical concern is that scoliosis-related osteopenia weakens the spinal architecture and may contribute to the progression of spinal deformity during growth. However, spinal progression is a multifactorial disorder and could be related to mechanical and structural properties of the spine [8–10]. The progression of spinal deformity is believed to be a mechanical modulation of the growth of the vertebrae [8–10]. The rate of scoliotic deformity progresses more rapidly during peripubertal bone growth. Biomechanical forces exerted onto the growing spine may modulate spinal growth in accordance with the Hueter-Volkmann law [26–27], which states that bone growth depends on the amount of compression on the growth plate —it is retarded by increased compression and accelerated by reduced compression [28–31]. The effects of mechanical forces, in particular asymmetric mechanical loading on the concave side of the immature scoliotic vertebrae, have been shown to induce greater compression load, retarding growth of vertebral bodies. This is in contrast to the convex side, which experiences more distraction load [8]. Consequently, the unbalanced forces might lead to angular progression of the scoliotic spine during rapid peripubertal growth.
Hence, improving bone mass could be one factor, among others, to improve bone strength. Further investigation is needed to establish whether an improved bone mass status, and thus bone strength, of the scoliotic spine retards the rate of spinal progression. Secondly, the prevalence of low bone mass in AIS patients is higher than that in the normal adolescent population [5]. This osteopenia will persist and eventually lead to substantially reduced peak adult bone mass [32–33], thereby increasing risk of osteoporotic fractures later in life [34]. Hence, promotion of bone mass could be of paramount importance in this group of patients for them to attain a higher peak bone mass and thus reduce risk of osteoporosis later in life. Thirdly, in AIS patients requiring surgical procedures, a strong preoperative bone mass is important for surgeons, because bone mass correlates well with bone strength, allowing implants and fixation for spinal fusion to be more accurately fixed. Fourthly, early treatment of low bone mass may modify the progression of scoliosis and minimize long-term problems associated with adult osteoporosis. These clinical implications are significant and, in our, opinion are worthy of further investigation.
Conclusions
This study showed for the first time study that curve severity was significantly and inversely associated with bone-mineral status of AIS patients during the peripubertal period. The proportion of osteopenic AIS girls in the severe group was significantly higher than that in the moderate group. Treatment of AIS-related osteopenia has not yet been instituted anywhere in the world. This could be due to the fact that the pathophysiology is still not fully understood. Appropriate treatment needs to be evidence-based. Results from the present large-scale study increase spinal surgeons’ awareness of the possible short-term and long-term complications of AIS-associated osteopenia. In AIS patients during the peripubertal period, preventing generalized osteopenia may be as important as controlling spinal progression.
References
Cook SD, Harding AF, Morgan EL, Nicholson RJ, Thomas KA, Whitecloud TS, Ratner ES (1987) Trabecular bone mineral density in idiopathic scoliosis J Pediatr Orthop 7:168–174
Snyder BD, Zaltz I, Breitenbach MA, Kido TH, Myers ER, Emans JB (1995) Does bracing affect bone density in adolescent scoliosis? Spine 20:1554–1560
Cheng JC, Guo X (1997) Osteopenia in adolescent idiopathic scoliosis. A primary problem or secondary to the spinal deformity? Spine 22:1716–1721
Cheng JC, Guo X, Sher AH (1999) Persistent osteopenia in adolescent idiopathic scoliosis. A longitudinal follow-up study. Spine 24:1218–1222
Cheng JC, Qin L, Cheung CS, Sher AH, Lee KM, Ng SW, Guo X (2000) Generalized low areal and volumetric bone mineral density in adolescent idiopathic scoliosis. J Bone Miner Res 15:1587–1595
Cheng JCY, Sher AHL, Guo X, Hung VWY, Cheung AY (2001) The effect of vertebral rotation of the lumbar spine on dual energy X-ray absorptiometry measurements: observational study. Hong Kong Med J 7:241–245
Lee WTK, Cheung CSK, Tse YK, Guo X, Qin L, Ho SC, Lau J, Cheng JCY (2005) Generalized low bone mass of girls with adolescent idiopathic scoliosis is related to inadequate calcium intake and weight-bearing physical activity in peripubertal period. Osteoporos Int 16(9):1024–1035
Stokes IA, Spence H, Aronsson DD, Kilmer N (1996) Mechanical modulation of vertebral body growth. Implications for scoliosis progression. Spine 21:1162–1167
Stokes IA (1997) Analysis of symmetry of vertebral body loading consequent to lateral spinal curvature. Spine 22:2495–2503
Villemure I, Aubin CE, Dansereau J, Labelle H (2004) Biomechanical simulations of the spine deformation process in adolescent idiopathic scoliosis from different pathogenesis hypotheses. Eur Spine J 13:83–90
Cheung CSK, Lee WTK, Tse YK, Tang SP, Lee KM, Guo X, Qin L, Cheng JCK (2003) Abnormal peri-pubertal anthropometric measurements and growth pattern in adolescent idiopathic scoliosis—a study of 598 patients. Spine 28:2152–2157
Cheng JCY, Leung SSF, Chiu BSK, Tse PW, Lee CW, Chan AK, Xia G, Leung AK, Xu YY (1998) Can we predict body height from segmental bone length measurements? A study of 3,647 children. J Pediatr Orthop 18:387–393
Cheng JCY, Leung SSF, Lau J (1996) Anthropometric measurements and body proportions among Chinese children. Clin Orthop 323:22–30
Bjure J, Grimby G, Nachemson A (1968) Correction of body height in predicting spirometric values in scoliotic patients. Scand J Clin Lab Invest 21:191–192
Hans D, Biot B, Schott AM, Meunier PJ (1996) No diffuse osteoporosis in lumbar scoliosis but lower femoral bone density on the convexity. Bone 18:15–17
Rüegsegger P, Koller B, Muller R (1996) A microtomographic system for the nondestructive evaluation of bone architecture. Calcif Tissue Int 58:24–29
Rüegsegger P (1996) Bone density measurement. In: Bröll H, Dambacher MA (eds) Osteoporosis: A guide to diagnosis and treatment. Rheumatology. Karger, Basel, 18:103–116
Qin L, Au SK, Chan KM, Lau MC, Woo J, Dambacher MA, Leung PC (2000) Peripheral volumetric bone mineral density in pre- and postmenopausal Chinese women in Hong Kong. Calcif Tissue Int 67:29–36
Hong Kong Department of Health (1997) Public health and epidemiology bulletin. Hong Kong, 6(2):1997
Department of Health, Hong Kong, SAR (2003–2004) Annual report. Government Printer, Hong Kong
NIH Consensus Development Panel on Osteoporosis Prevention, Diagnosis, and Therapy (2000) Consensus Development Conference. NIH 17(1):1–45 [http://consensus.nih.gov/cons/111/111_intro_htm]
Lee WTK (1993) Requirements of calcium: Are there ethnic differences? Asia Pac J Clin Nutr 2:183–190
Lee WTK, Leung SSF, Wang SH, XU YC, Zeng WP, Lau J, Oppenheimer SJ, Cheng J (1994) Double-blind controlled calcium supplementation and bone mineral accretion in children accustomed to low calcium diet. Am J Clin Nutr 60:744–752
Lee WTK, Leung SSF, Leung DMY, Tsang HSY, Lau J, Cheng JCY (1995) A randomised double-blind controlled calcium supplementation trial, and bone and height acquisition in children. Br J Nutr 74:125–139
Lee WTK, Cheng JCY, Cheung CSK, Guo X, Ho S, Lau J (2003) Inadequate calcium intake is a significant determinant on generalised osteopenia in Hong Kong Chinese adolescents with idiopathic scoliosis. Wei Sheng Yan Jiu 32:568–572
Hueter C (1862) Anatomische Studien an den Extremitaetengelenken Neugeborener und Erwachsener. Virchows Arch Pathol Anat Physiol Klin Med 25:572–599
Volkmann R (1882) Verletzungen und Krankenheiten der Bewegungsorgane. In: von Pitha, Billroth (eds) Handbuch der allgemeinen und speciellen Chirurgie Bd II Teil II. Ferdinand Enke, Stuttgart
Arkin AM, Katz JF (1956) The effects of pressure on epiphyseal growth. The mechanism of plasticity of growing bone. J Bone Joint Surg Am 38:1056–1076
Gooding CA, Neuhauser EBD (1965) Growth and development of the vertebral body in the presence and absence of normal stress. AJR Am J Roentgenol 93:388–394
Hert J, Liskova M (1964) Regulation of the longitudinal growth of the long bone by mechanical influence. Acta Univ Carol Med 20 [Suppl]:32–34
Roaf R (1960) Vertebral growth and its mechanical control. J Bone Joint Surg Br 42:40–59
Velis KP, Healey JH, Schneider R (1989) Peak skeletal mass assessment in young adults with idiopathic scoliosis. Spine 14:706–711
Vanderpool DW, James JI, Wynne-Davies R (1969) Scoliosis in the elderly. J Bone Joint Surg Am 51:446–455
Healey JH, Lane JM (1985) Structural scoliosis in osteoporotic women. Clin Orthop 195:216–223
Cheung CSK, Lee WTK, Tse YK, Lee KM, Guo X, Qin L, Cheng JCY (2005) Generalized osteopenia in adolescent idiopathic scoliosis —association with abnormal pubertal growth, bone turnover and calcium intake? Spine (in press)
Acknowledgements
We would like to express our gratitude for the support from patients, healthy volunteers and their parents. Without their support, this study would not have been possible. We also thank Mr. Jacky W.W. Chau, Miss Vivian W.Y. Hung, Miss Christine Lee, and Miss Catherine Li for assistance in field work, and Dr. Simon K.M. Lee for going through the final manuscript. The study was supported by an Earmark Research Grant from the Research Grant Council (CUHK No. 4336/99), Hong Kong SAR, and a grant from the Health Service Research Committee / Health Care and Promotional Fund (HSRF No. 921024), Hong Kong SAR
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee, W.T.K., Cheung, C.S.K., Tse, Y.K. et al. Association of osteopenia with curve severity in adolescent idiopathic scoliosis: a study of 919 girls. Osteoporos Int 16, 1924–1932 (2005). https://doi.org/10.1007/s00198-005-1964-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-005-1964-7