Abstract
A group of Northern Ireland women aged 40–75 years of age with low-trauma forearm fracture were studied to determine the incidence of such fractures and the prevalence of osteoporosis in this fracture population. A total of 1,147 subjects were identified in 1997 and 1998 throughout Northern Ireland following low-trauma forearm fractures, as well as 699 residents in the Eastern Health and Social Services Board (EHSSB), enabling calculation of the annual incidence rate of new low-trauma forearm fractures at 2.69/1,000 population aged 40–75. A total of 375 participants consented to have bone mineral density (BMD) measurements undertaken at the femoral neck, spine, and forearm using a Lunar Expert bone densitometer. Osteoporosis at the femur was present in 14% of women, at the spine in 29%, and at the forearm in 32%. A total of 45% were osteoporotic at one or more measured sites, but only 18% were on treatment for osteoporosis. Additional significant risk factors identified included an early menopause in 24.5% and current or previous corticosteroid use in 13%. Only 1.6% received information on treatment of osteoporosis at the time of fracture. Increased awareness is needed in both primary and secondary care including fracture services to improve treatment of women with low-trauma fracture.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Distal forearm fracture is a common event in women, with a lifetime risk of 14% [1]. Such fractures may be particularly important as a marker of underlying osteopenia or osteoporosis, with increases of 2 to 3 times of the expected rate of subsequent vertebral or hip fracture in comparison to the general population [2, 3, 4, 5]. Women with distal forearm fracture have reduced bone mineral density at the hip [6], the lumbar spine [7], and the heel [8]. Low-trauma fragility forearm fracture is a recommended indication for bone density measurement [9, 10] and treatment for osteoporosis where appropriate, but often these not undertaken [11, 12, 13]. While there is no apparent excess mortality following Colles fracture [14], it interferes significantly with self-care activities, with approximately 40% of patients requiring hospital admission [15]. Up to 30% may develop longer term complications including algodystrophy, osteoarthritis, and neuropathy [16], and nearly half report only fair or poor outcomes at 6 months [17].
In view of the rising numbers [18] of women presenting with hip fracture in Northern Ireland and the high 6-month female mortality of 16% [19] and the cost [15], it was considered important to establish the prevalence of osteoporosis in women with low-trauma distal forearm fracture and the current provision of treatment for osteoporosis in this population. Appropriate targeted treatment may be an important measure if future reduction of osteoporotic fracture is to be achieved. We have studied a group of Northern Ireland women with low-trauma forearm fracture to determine the incidence of such fractures and the prevalence of osteoporosis in this population.
Methods
Women aged 40–75 years presenting with distal forearm fracture in 1997/1998 in 7 hospitals covering over 90% of the population in Northern Ireland were identified. Ethical approval was obtained for the study from the Ethical Committee of the Queen’s University of Belfast. Fracture patients were identified from accident and emergency records, fracture clinic attendance, and radiology records. Patients were deemed to have a low-trauma fracture if the injury occurred from a fall from standing height or less. Following written informed consent, information on risk factors for osteoporosis was obtained by a trained osteoporosis nurse. The information was gathered on a standard proforma included demographic details, previous steroid therapy, age of menopause, hormone replacement therapy, alcohol intake, dietary calcium intake, smoking history, falls in preceding 6 months, fractures, patient education following attendance at a fracture clinic, and medication.
The population by postal code was obtained for the Eastern Health and Social Services Board (EHSSB) region of Northern Ireland from the Central Services Government register for 1997 and 1998. This enabled the incidence figures for low-trauma fracture to be calculated by age bands per 1,000 population allowing the annual incidence rate of low-trauma fractures / 1,000 population / year to be derived. The EHSSB population was chosen as it incorporated the more densely populated greater Belfast area in which forearm fracture ascertainment was highest.
Bone mineral density measurement
Bone mineral density (BMD) measurement of the lumbar spine (L2–L4), neck of femur (femoral neck region), and nondominant forearm (radius total region) were measured in g/cm2 by dual-energy X-ray absorptiometry using a Lunar Expert Bone Densitometer. The T-score reference population for each region was the UK female reference population supplied by the manufacturer. Subjects were categorized using the World Health Organization recommendations, at each region of interest, as normal if bone mineral density was above −1 standard deviation (SD) of the young adult mean, as osteopenia if between −1and −2.5 SD, and as osteoporotic if below −2.5 SD [20].
Results were analyzed using the Statistical Package for Social Sciences (SPSS).
Results
A total of 1,147 patients aged 40–75 years with low-trauma forearm fracture were identified in 1997 and 1998 throughout Northern Ireland. Of these, 699 residents living in the EHSSB post codes were identified, and their incidence of low-trauma female forearm fractures / 1,000 population / year calculated for the total population and by age band, as shown in Table 1. The overall annual incidence of new low-trauma forearm fracture was 2.69/1,000 population aged 40–75.
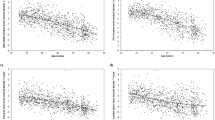
A total of 375 subjects attended for BMD measurement (Table 2). Of these 54 (14%) had osteoporosis at the hip, 107 (29%) at the spine, and 120 (32%) at the forearm with 5 (1%) subjects osteoporotic only at the hip, 34 (9%) osteoporotic only at the spine, and 43 (11%) osteoporotic only at the forearm (Table 3). Osteoporosis was present at both hip and spine measurement site in 39 (10%) subjects, hip and forearm in 40 (11%) subjects, and spine and forearm 64 (17%) subjects. Osteoporosis at all three measured sites was recorded in 30 (8%) subjects. A comparison of the prevalence of osteoporosis in those above and below the age of 60 years is outlined in Table 3.
Overall a total of 168 (45%) were osteoporotic at one or more measured sites, of whom 30 (18%) were on treatment for osteoporosis. Of these, 9 subjects (5%) were receiving bisphosphonate therapy, 10 (6%) calcium supplementation, 2 (1%) oral vitamin D supplements, and 11 (7%) hormonal treatment. Comparison of subjects over and under the age of 60 years revealed no differences in the proportion with osteoporosis receiving treatment.
The risk factor data for the study groups revealed that 20% were current smokers (Table 4). Additional significant risk factors identified included an early menopause (i.e., at less than 45 years) in 25%, a previous hysterectomy in 26% at a mean age of 43.8 years, and one or both ovaries removed in 13%. The mean spine BMD in the 259 patients on whom no documented gynecological surgery had been performed was 1.01 g/cm2 , in the 47 patients who had had a hysterectomy alone was 0.989 g/cm2, and in the 47 patients who had undergone both hysterectomy and oophorectomy was 0.958 g/cm2, which was significantly reduced in comparison to those on whom no surgery was performed (p=0.025). Current or previous corticosteroid use was recorded in 13%. Seventeen percent had fallen within the previous 6 months. At the time of their attendance at the fracture clinic, only 3% had received advice about osteoporosis, 2% on fall prevention, and only 1.6% received information on treatment of osteoporosis.
Discussion
We have found that the standardized incidence by age band of low-trauma fractures in females was highest in the age range 65–69 years. In men, 52% of forearm fractures have been attributed to severe trauma and 21% in women [21], and, therefore the incidence of forearm fracture attributed to low trauma will not be as great as the overall total incidence. This is reflected in the yearly incidence of low-trauma forearm fracture recorded in this study of 4.41/1,000 population aged 65–74 in comparison to the 6.2/1,000 population of all forearm fractures reported in Oxford, UK [22] and the 6.7/1,000 in Rochester, USA [21].
We have shown that osteoporosis is present in a high proportion of patients presenting with low-trauma forearm fracture. The presence of osteoporosis in one of the three measured sites in 45% of patients confirms the high prevalence in forearm fracture patients. The prevalence of osteoporosis was lowest at the hip at 14%, with 29% osteoporotic at the spine and 32% at the forearm. Nonconcordance of BMD measurements between sites has been previously highlighted [23] with differing coefficients of variation of measurement of 1.48% at the lumbar spine, 0.99% for total hip, and 1.82% for the ultradistal forearm [24]. The proportion (29%) with osteoporosis at the spine is lower, however, than the 47% reported from Spain [6], but the 33% with osteoporosis at the hip or spine is similar to the 36% observed in Glasgow [25] and the 39% with the osteoporosis at the heel in Nottingham [8].
If the National Institute for Clinical Excellence [26] proposal in the United Kingdom to advocate treatment in women younger than 65 years of age only if the T-score is less than −3.2 is adopted, 2 of the patients would have had such a score at the hip and 22 in the spine, resulting overall in only 24 out of 246 (10%) being recommended for pharmacological treatment.
Identification of modifiable high-risk factors for osteoporosis allows a more targeted approach to management and prevention of further bone loss. A previous fragility fracture is a high-risk factor for further fracture, and therefore first attendance at a fracture clinic should be an opportunity to assess further fracture risk and to enable interventions to be introduced for secondary fracture prevention.
In our study group of patients attending a fracture clinic we identified several potentially modifiable lifestyle factors including a high prevalence of smokers and history of corticosteroid therapy. While vitamin D levels were not measured in these patients, subclinical deficiency of vitamin D has been identified in 20–40% of elderly patients at home and in institutional care in Northern Ireland [27, 28]. Only 1% of patients with osteoporosis were receiving vitamin D supplementation, and 10% calcium supplementation. Attention to both vitamin D and calcium dietary intake would be important in secondary fracture prevention advice. In addition, 16.5% had reported a minor fall within the previous 6 months, suggesting the need for further assessment and intervention to minimize further risk by preventing a second fall.
The most significant finding, however, was the large number (24.5%) who reported an early menopause (i.e., under 45 years of age). Many of these had had a previous hysterectomy and in 12% one or both ovaries had been removed. These findings would suggest that on attendance at a fracture clinic an enquiry should be made regarding these gynecological procedures and more importantly would suggest that treatment for prevention of bone loss should be considered at the time of the original surgery.
In current clinical practice, only a small proportion (18%) of those with forearm fracture and osteoporosis are currently receiving active intervention and treatment for osteoporosis, and this is not provided more often in either younger or older patients. Similarly low uptake of treatment has been reported in other regions despite clinical guidelines [29]. Unfortunately, at the time of fracture only 3% had received advice on osteoporosis, only 2% had been advised regarding fall prevention, and in only 1.6% of patients was investigation or treatment discussed. These findings may reflect the busy working environment of the fracture clinics and support the concept of a liaison fracture clinic nurse as a worthwhile service development to introduce more effective secondary fracture prevention [30, 31].
There is a need to highlight the importance of low-trauma fracture itself as a trigger of treatment for bone protection, and this requires increased awareness of the importance of such treatment. Such patients are at increased relative risk of fracture independent of BMD. Enhanced availability of bone mineral density measurements will enable an even higher risk subgroup to be identified with lowered bone mineral density who are at increased risk of further fracture, particularly in the spine, forearm, and hip. Such patients may particularly benefit from therapeutic intervention. In our study of 40% of the women in Northern Ireland in this age group, current health care strategies are not identifying patients with low-trauma fracture who would benefit from such bone protection. In Northern Ireland with a female population of 338,300 between the age of 40 and 75 (Northern Ireland Statistics and Research Agency) we would envisage approximately 900 low-trauma forearm fractures occurring each year requiring targeted intervention and appropriate bone protection.
Increased awareness is needed in both primary and secondary care including fracture services to improve treatment of women with low-trauma fracture.
References
Lindsay R, Meunier PJ (1998) Osteoporosis: review of the evidence for prevention, diagnosis and treatment and cost effective analysis. Osteoporosis Int 8[Suppl 4]:53–56
Van Staa TP, Leufkens HGH, Cooper C (2002) Does a fracture at one site predict later fractures at other sites? Osteoporos Int 13:624–629
Cuddihy MT, Gabriel SE, Crowsson CS, O’Fallon WM, Melton LJ III (1999) Forearm fractures as predictors of subsequent osteoporotic fractures. Osteoporos Int 9:469–475
Malmin H, Ljunghall S, Persson I, Naesen T, Kruseme UB, Bergstrom R (1993) Fracture of the distal forearm as a forecaster of subsequent hip fracture: a population-based cohort study with 24 years of follow-up. Calcif Tissue Int 52:269–272
Lauritzen JB, Schwartz P, McNair P, Lund B, Transbol I (1993) Radial and humeral fractures as predictors of subsequent hip, radial or humeral fractures in women, and their seasonal variation. Osteoporos Int 3:133–137
Kanterewicz E, Yanez A, Perez-pons A, Codony I, Del Rioc Diez-Perez A (2002) Association between Colles’ fracture and low bone mass: age-based differences in post menopausal women. Osteoporos Int 13:824–828
Peel NFA, Barrington NA, Smith TWD, Eastell R (1994) Distal forearm fracture as risk factor for vertebral osteoporosis. BMJ 308:1543–1544
Masud T, Jordan D, Hosking DJ (2001) Distal forearm fracture history in an older community-dwelling population: the Nottingham Community Osteoporosis (NOCOS) Study. Age Ageing 30:255–258
Barlow DH (1994) Report of the Advisory Group on Osteoporosis. Department of Health, London
Anonymous (1999) Clinical guidelines for prevention and treatment of osteoporosis. Royal College of Physicians, London
Freedman KB, Kaplan FS, Bilker WB, Strom BL, Lowe RA (2000) Treatment of osteoporosis: are physicians missing an opportunity? J Bone Joint Surg Am 82A:1063–1070
Hajesar EE, Hawker G, Bogoch ER (2000) Investigation of treatment for osteoporosis in patients with fragility fractures. Can Med Assoc J 163:819–822
Torgerson DJ, Dolan P (1998) Prescribing by general practitioners after an osteoporotic fracture. Ann Rheum Dis 57:378–379
Cooper C, Atkinson EJ, Jacobson SJ, O’Fallon WM, Melton LJ III (1993) Population based study of survival after osteoporotic fractures. Am J Epidemiol 137:1001–1005
Dolan P, Torgerson DJ (1998) The cost of treating osteoporotic fractures in the United Kingdom female population. Osteoporos Int 8:611–617
Looney WP, Dobyns JH, Linscheid RL (1980) Complications of Colles’ fractures. J Bone Joint Surg 62A:613–619
Kaukonen JP, Karaharju EO, Pomas M, Lathje P, Jakobsson A (1988) Functional recovery after fractures of the distal forearm: analysis of radiographic and other factors affecting the outcome. Ann Chir Gynaecol 77:27–31
Beringer TRO, Wilson RA, Swain D, Patterson CC, Beverland D (2000) Proximal femoral fracture in Northern Ireland between 1985–1997: trends and future projections. Ulster Med J 69:112–117
Wilson RA, McAnespie M, Dolan A, Smyth JR, Elliott JRM, Steele IC, Marsh DR, Heyburn G, Beringer TRO (1999) A comparison of male and female mortality at 6-months following a femoral neck fracture. Age Ageing 28[Suppl 2]:81
Kanis JA, Melton LJ III, Christensen C, Johnson CC, Khaltuer N (1994) The diagnosis of osteoporosis. J Bone Miner Res 8:1137–1141
Melton LJ III, Amadio PC, Crawson CS, O’Fallon WM (1998) Long-term trends in the incidence of distal forearm fractures. Osteoporos Int 8:341–348
Winner SJ, Morgan CA, Evans JG (1989) Perimenopausal risk of falling and incidence of distal forearm fracture. BMJ 298:1486–1488
Feyerabend AJ, Lear JL (1993) Regional variations in bone mineral density as measured with dual energy photon absorptiometry and dual energy x-ray absorptiometry. Radiology 186:467–469
Sahota D, Pearson D, Cante SW, San P, Hosking DJ (2000) Site specific variation in the classification of osteoporosis and the diagnostic reclassification using the lowest individual lumbar vertebra T-score compared with L1-L4 mean in early post menopausal women. Osteoporos Int 11:852–857
Gallacher SJ, Walker B, McCreath S, Watson WS (2000) An audit of bone densitometry screening following wrist fracture. Osteoporos Int 11[Suppl 1]:521
National Institute of Clinical Excellence (2004) Appraisal consultation document: technologies for the prevention and treatment of osteoporosis and prevention of osteoporotic fractures in women. http://www.nice.org.uk/. Cited 17 July 2003
Beringer TRO (1985) A clinical study of metabolic bone disease in the elderly in relation to proximal femoral fracture. MD Thesis, Queen’s University of Belfast
Vir SC, Love AHG (1978) Vitamin D status of elderly at home and institutionalized in hospital. Int J Vit Nutr Res 45:123–30
O’Riordan S, Mortimer K, Sturgess I, Batty G (2001) Audit of investigation and treatment of osteoporosis after Colles Fracture. Age Ageing 30[Suppl 2]:25
McLellan AR, Fraser M (2001) The osteoporosis-orthopaedic liaison nurse: a service model for effective delivery of strategies for the secondary prevention of osteoporotic fractures. Osteoporos Int 12[Suppl 2]:547
McLellan AR, Gallacher SJ, Fraser M, McQuillian C (2003) The fracture liaison service: success of a program for the evaluation and management of patients with osteoporotic fracture. Osteoporos Int 14:1028–1034
Acknowledgements
We wish to thank all the women who participated in the study and acknowledge the help of the Department of Radiology at Musgrave Park Hospital with respect to DXA scanning expertise and also Mr Ken Moffett for data analysis. Proctor and Gamble Pharmaceuticals supported the study with a unrestricted research grant.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Beringer, T.R.O., Finch, M., McA. Taggart, H. et al. A study of bone mineral density in women with forearm fracture in Northern Ireland. Osteoporos Int 16, 430–434 (2005). https://doi.org/10.1007/s00198-004-1684-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-004-1684-4