Abstract
Distal radius fracture is an early indicator of osteoporosis, yet little is known about men with this fracture and osteoporosis prevalence. The purpose of this cross-sectional, controlled study was to evaluate bone mineral density (BMD) in men, from working age to the elderly, with distal radius fracture. Recruitment was as follows: men who fractured during 1999–2000 were evaluated retrospectively in 2003 and men who fractured during 2003–2007 were followed prospectively for one year post-fracture. A total of 233 patients, response rate 40 %, were enrolled and compared with 643 controls. Fractures from all degrees of trauma were included. BMD was measured at femoral neck, total hip, and lumbar spine. Mean age at fracture was 52 years (21–88 years). Men aged 40–64 years had 5.4–6.7 % lower BMD at all sites compared to controls (p = 0.001) and in >65 years BMD was lower by 10.7–13.8 % (p < 0.001), while not significant at <40 years (1.4–2.8 %; p = 0.228–0.487). Osteoporosis was more prevalent at all ages (20–39 years: 8.5 vs 1.5 %; 40–64 years: 16.8 vs 5.1 %; >65 years: 23.3 vs 8.3 %) BMD did not differ with trauma level. Already from age 40, men with a distal radius fracture had lower BMD, the difference becoming more pronounced with increasing age. Also, the prevalence of osteoporosis was higher, surprisingly even in the youngest age group.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The distal radius is one of the most frequent fracture sites for both men and women [1] and it represents one of the earliest indicators of osteoporosis and risk of future fragility fractures [2, 3]. For both men and women, a previous distal radius fracture is associated with an increased risk of a subsequent hip fracture, the risk being more pronounced in men and particularly in men at relatively younger ages [3].
A distal radius fracture is the result of a fall to the out-stretched hand, often in an individual with compromised bone strength [4]. In contrast to women, the incidence remains relatively low in men until the age of 70–80 after which there is a moderate increase [5, 6]. The difference in prevalence is partly explained by differences in bone size and cortical thickness [7] which provides a mechanical advantage to the male appendicular bone. In Scandinavia, incidence rates for both men and women are higher than in the rest of Europe [8] for reasons not fully understood but possible explanations include a higher degree of osteoporosis and vitamin D deficiency. Moreover, with falls in general being the universally strongest risk factor of non-vertebral fractures in the older adult, outdoor falls from icy weather conditions are common cause of distal radius fractures at these latitudes [9, 10].
Distal radius fractures in women are extensively studied, whereas information still is limited in men. In a first study from 2002, it was shown that men with distal radius fracture have a lower bone mineral density (BMD) than their peers and a higher risk of osteoporosis [11] and additional studies have been comparatively few and small in size [11–14].
A distal radius fracture is regarded as a fracture of the middle aged or old, and because of this, most studies are performed in patients aged 50 and above. However, distal radius fractures also occur in younger men; what if reduced bone mass is present already at this early age?
Our primary hypothesis was that men who sustain a distal radius fracture have lower BMD compared to the background population regardless of age or degree of trauma. To investigate this, we performed a cross-sectional, controlled study with 233 men with distal radius fracture and 643 controls. An additional question was what proportion would have BMD classified as osteoporotic, osteopenic, and normal?
Methods
Subjects and Design
This study of adult men with distal radius fracture was conducted at the Department of Orthopedics, Skåne University Hospital, Malmö, the third largest city in Sweden. Men, resident in the catchment area, aged 20 or above presenting with a distal radius fracture resulting from any trauma were eligible for the study. Patients who did not speak or understand Swedish and those with multiple fractures were excluded since the protocol included self-reported outcome instruments. No other exclusion criteria, such as co-morbidities or medications, were applied.
In the first, retrospective, part of the study, we identified all men who had consulted the orthopedic or radiology departments after sustaining a distal radius fracture during 1999–2000, by reviewing patient case files and radiology reports. During fall 2003, these men were invited by mail to participate in the study and were examined at one visit at the Osteoporosis Research Unit between December 2003 and June 2004, time from fracture to examination mean 4.1 years, range 3.2–5.3.
In the second, prospective, part of the study, conducted between March 2003 and March 2007, we invited all men with acute distal radius fractures to participate in the study. The reason for extending the study with a prospective arm was to allow for functional follow-up at one year and reach beyond a cross-sectional descriptive study. The fracture patients were identified through the admission records of the Emergency Department or at the one-week routine control at the out-patient clinic. An initial questionnaire was distributed during the first week; the examination was performed 6–8 weeks later (mean 8 weeks, range 4–19 weeks) and the participants were followed up at 6 and again at 12 months.
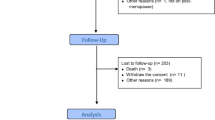
We identified a total of 738 men who suffered a distal radius fracture (288 in the retrospective arm, 450 in the prospective arm). 151 patients were excluded: 42 had an existing fracture in the prospective part of the study; 26 had multiple fractures; 46 were deceased prior to investigation; 18 patients were non-resident in Malmö and 19 did not speak Swedish. Of the remaining patients, 233 agreed to participate in the study (n = 100 in the retrospective arm, n = 133 in the prospective arm), giving a response rate of 40 %. Non-participants: a total of 354 fracture patients declined participation in the study; 279 were unwilling or did not respond to invitation, 60 reported severe illnesses, and 15 had a known active substance abuse. The mean age of the non-participants was 53.6 ± 20.2 years (range 20–93). There were no significant difference in age between participants and non-participants (p = 0.77).
The control group consists of 643 men aged 24–81 years from a pre-existing database who had been examined at the clinic during 2003–2013 as part of the European Male Aging Study [12] and as controls in an infertility study and is representative of a cross-section of the adult male population in the catchment area.
At the time of investigation, all participants and controls underwent a baseline examination including BMD measurement, blood sampling, and completed a health-related questionnaire.
All parts of the study were approved by the Lund University ethical review board and performed in compliance with the Helsinki Declaration. Participants were informed of the purpose of the study and gave their signed informed consent before being enrolled.
Measurements
The participants completed a comprehensive questionnaire on health status, medication, previous fractures, family history, educational level, and lifestyle factors such as diet, tobacco, alcohol consumption, and physical activity. Factors associated with secondary osteoporosis were classified as the use of oral steroids longer than 3 months, use of anticonvulsants or warfarin, alcohol consumption more than 21 units a week, malabsorption due to longtime gastric ulcer or inflammatory bowel disease, celiac disease, inflammatory arthritis, or long-term immobilization. The data collected from the controls, contained some but not sufficient information to allow for similar analysis.
Anthropometric characteristics were assessed at the time of the BMD measurement. A stadiometer was used for height measurements to the closest 0.5 cm and a standard scale for weight to the nearest 0.5 kg. BMI was calculated according to the formula, weight in kilograms divided with the squared height in meters and expressed in kg/m2.
Degree of trauma was recorded by questionnaire. The fracture cases were divided into either low- or high-trauma category. Low-energy trauma was defined as a fall from standing height or less. High trauma was defined as fall from any height or traffic accident.
BMD (g/cm2) at the femoral neck (FN), total hip (TH), and lumbar spine, L2–L4 (LS) was measured in 207 fracture patients and 545 controls. BMD was assessed using dual-energy X-ray absorptiometry (DXA); Lunar Prodigy (GE Healthcare Lunar, Madison, WI, USA), software versions 2.15–7.70 were used for all fracture patients and the majority of controls (88.6 %; 570 of 643); for the final 73 controls, instrument failure obliged us to use the Lunar iDEXA (GE Healthcare Lunar, Madison, WI, USA). These participants composed a significant part of the younger controls and we chose to include but performed a cross-calibration to compensate for the small variation. The BMD data used in the statistical analyses have been adjusted to the Prodigy. To do this, a cross-calibration was performed using 34 healthy individuals (13 men; 21 women) who underwent DXA scans by both devices. Using a Bland and Altman plot the mean difference in BMD was calculated (0.0006 g/cm2 at FN; 0.0002 g/cm2 at TH; −0.0088 g/cm2 at LS) and subsequently added to the original value. We found no inherent bias and a very good correspondence between measurements made by the two devices. DXA measurements were performed by the same research technicians throughout the study period and stability and accuracy were monitored using a manufacturer-supplied phantom three times per week. The precision coefficients (CV %) for DXA have been reported previously as 0.9 % FN, 0.5 % TH, and 0.7 % L2–L4 [13]. T-score calculations were derived from the DXA manufacturer-supplied reference population, i.e., males aged 20–39 of USA/European origin [14]. We applied the operational WHO definition for osteoporosis (T-score ≤ −2.5 SD), osteopenia (T-score > −2.5 SD and <−1.0 SD), and normal bone density (T-score ≥ −1). In 2013, the International Osteoporosis Foundation (IOF) stated that female reference data should also be used to calculate T-scores for men since fracture occurs at the same absolute BMD in men and women. We present T-scores derived from both the male and the female reference data since T-scores based on male reference data are widely implemented clinically, male-specific reference databases are used by the major densitometer manufacturers to calculate T-scores for men, and it allows for comparison with published studies. T-scores based on female reference data were calculated using the following formula:
Z-scores, adjusted for age and weight, were also obtained from the machine.
Statistics
In men, age-related decrease in BMD is considered to become evident around 60–70 years, with low BMD rare in otherwise healthy men below age 40 [15]; therefore in the analyses, the cases and controls were divided into three age groups: 20–39, 40–64, and 65 years and above. Categorical variables are expressed as number and percentage, and continuous variables as mean with standard deviation (SD) and/or range. Quantitative data were tested for normality, Kolmogorov–Smirnov test, and were found to be normally distributed. We used independent unpaired t-test for continuous variables and Chi-square test for comparisons between categorical variables. Regression analysis of absolute BMD values was performed and data adjusted for age and BMI. Odds ratios (OR) and 95 % confidence intervals (95 % CI) for osteoporosis were estimated in conditional logistic regression analyses adjusted for BMI and age. Acknowledging that the controls were not collected specifically for this study or age-matched, we performed an additional sensitivity analysis to confirm our results. Using computerized age matching, cases were matched to controls ±2 years. This resulted in exclusion of eleven cases (the four youngest and the seven oldest) such that the age range narrowed to 22–84 years (mean 58 ± 13).
Age matching was performed using SPSS v20 (IBM Corp., NY, USA) and SAS 9.4 (SAS Institute Inc., Cary, NC, USA); all statistical analyses were performed using SPSS. We considered a two-tailed p-value <0.05 statistically significant.
Results
Demographic and Clinical Data
The controls were slightly younger than the fracture cases at the time of examination while height, weight, BMI, and smoking status was similar in both groups. There was a higher prevalence of cardiovascular disease in the fracture group compared to controls and a tendency toward more co-morbidity (Table 1). Factors potentially associated with secondary osteoporosis were found in 21 % of the fracture patients.
The mean age when distal radius fracture occurred was 52.2 years (20.6–88.3). Fracture distribution according to age group was 27 % (20–39 years), 44 % (40–64 years), and 29 % in those ≥65 years. There were 122 men with low-energy trauma and 91 with high-trauma fractures (13 bicycle and 9 car accidents); in 20 cases the trauma level was unknown. The mean age was higher in the low-trauma cases (55 years vs 49; p = 0.17) (Table 2, Supplementary Table 1). In the youngest age group, among those with known trauma level, the distribution was similar; 47 % (n = 27) low, 43 % (n = 25) high. Only from the age of 65, the proportion of low-trauma distal radius fractures was higher, 68.3 versus 25.4 %.
Bone Mineral Density
First, we evaluated BMD in the retrospective and prospective arms of the fracture cohort. We found no significant difference between the groups (FN: 0.933 vs 0.927; p = 0.834, TH: 0.994 vs 0.973; p = 0.283, LS: 1.153 vs 1.164; p = 0.655). In the age-stratified BMD analyses, similar results were obtained within the retrospective and prospective arms, therefore they were merged to create a single-fracture group in subsequent analyses. Secondly, we evaluated the fracture group by comparing the low- and high-trauma groups. We found no significant difference in BMD, T-scores, or Z-scores at any site between the two groups (Table 2). After subdividing into age groups, the result remained the same. Those with unknown trauma level did not differ regarding age, BMI, or BMD compared to the group with known (low/high) trauma level.
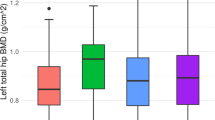
The DXA measurements for the entire fracture group were then compared to the control group. Overall, men with distal radius fracture had significantly lower BMD (6.7–7.3 %) at all sites compared to controls (Table 3) and adjustment for age and BMI did not alter this result. The difference in BMD between patients and controls increased with age. As shown in Table 3, fracture patients age 40–65 years had a 5.4–6.7 % lower BMD compared to equivalently aged controls (p < 0.001) while in the 65 and above group, this was doubled to 10.7–13.8 %. Adjustment for age and BMI of absolute BMD values did not substantially alter this finding, neither did inclusion of smoking in the model. In men below 40 years, the 2.8 % lower FN-BMD in radius fracture cases was not significant although after adjustment the similarity was attenuated. To evaluate a potential interaction between age and BMD, we performed a logistic regression analysis and found that age was somewhat more important for BMD in the cases compared to the controls. Pearson correlations coefficient was 0.351 for the controls compared to 0.547 in the cases (p = 0.004), indicating a stronger negative association between BMD and age in men with distal radius fracture.
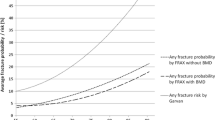
Men aged 40–64 years with distal radius fracture had Z-score’s between −0.41 and −0.67 SD and values in those over 65 years ranged between −0.49 and −0.60 SD which in both age groups was significantly lower than among equivalently aged controls (40–64 years: −0.010 to −0.13; ≥65 years: 0.23 to −0.83). The proportion of individuals with Z-score < −1 was almost twice as high in the fracture group as a whole (FN: 24.2 vs 15.2 %, TH: 24.8 vs 12.9 %, LS: 36.5 vs 22.7 %). The difference in Z-score was most pronounced in men aged 40 and above but diminished in the youngest age group (Fig. 1).
Making comparison to a young, sex matched reference population, using the T-score, we found an even more pronounced trend. In the entire group of distal radius fracture patients, and in each of the age groups, the proportion of men with a diagnosis of osteoporosis (T-score ≤ −2.5) at any skeletal site was 3–5 times higher than in the controls (Fig. 2), with the largest proportional difference in the youngest men (20–39 years, 8.5 vs 1.5 %, p = 0.023). This increased risk of osteoporosis among men with fracture was evident even after adjustment for BMI and age (OR = 3.5, 95 % CI (2.034–6.185); p < 0.001). When specifically evaluating femoral neck BMD, we find more than three times as many individuals with a T-score < −2.5 in the fracture group (Table 4). The same tendency was observed at each individual skeletal site; in the oldest men, osteoporosis was more common in the cases both at the hip (FN 18.6 vs 5.8 %) and spine (13.3 vs 5.0 %) and generally more prevalent in the hip compared to the spine.
No statistical difference was observed in the youngest age group, although there was a tendency for a higher prevalence of osteoporosis in the fracture group (FN 4.3 vs 1.5 %, p = 0.28; LS 4.3 vs 1.5 %, p = 0.28). Osteopenia was also more frequent at all skeletal sites among distal radius fracture patients (Table 4).
As expected, T-scores derived from female reference data were higher, resulting in a lower proportion diagnosed as osteopenic and osteoporotic in both fracture and control groups.
Repeating the analyses in the age-matched dataset, we found that the results obtained were essentially unchanged.
Discussion
Although osteoporosis most commonly affects women, men do sustain fragility fractures and compared to women the consequent mortality is considerably higher [16]. Majority of women with distal radius fracture have sub-normal BMD while the association in men is less well understood since the trauma mechanism may differ. Yet, surprisingly, few studies have specifically investigated BMD in men with distal radius fracture [11, 17, 18] and most have an emphasis on the elderly.
Our study of adult men goes beyond just supporting previous findings that BMD is lower in cases of radius fracture. We show that men with distal radius fracture already from the age of 40 have significantly reduced bone mass compared to the population average. Furthermore, even below age 40 men with this fracture type already exhibit a tendency toward low BMD. Our results revealed that three times more men with distal radius fracture had osteoporosis compared to the background population. Although using the IOF recommendation of T-scores derived from female reference data resulted in fewer men having a diagnosis of osteoporosis, the fact remains that men with radius fracture have a demonstrably lower bone mass indicating that men who have suffered a distal radius fracture are a population at risk requiring further clinical investigation.
A smaller study of 67 British men found forty-two percent of the fracture group (mean age 61) to be osteoporotic compared with ten percent in healthy age-matched controls, with fifty percent reporting risk factors associated with secondary osteoporosis [11]. In the equivalently aged men in our cohort, the comparative proportion with osteoporosis was much less and only one-fifth reported secondary factors. Our finding is more in agreement with a cross-sectional study of older men from the Glasgow Fracture Liaison Service study who also report a twenty-three percent with osteoporosis at all sites [19]. In comparison, a Norwegian cross-sectional study of distal radius fractures in patients above age fifty reported incidence of osteoporosis at any site in men as 33 % [20] and thus slightly higher than we report, although a smaller case–control study (n = 85 and n = 54) only found a significant prevalence of osteoporosis at the lumbar spine (23 vs 10 %) [21]. All of the above-mentioned studies base their results on T-scores calculated using male reference data.
We also show that younger men with distal radius fracture have low bone mass; almost 1 in 10 aged 20–39 had bone mass reduced to such an extent that it complies with an osteoporosis diagnosis. Previous studies have all excluded men below the age of forty under the assumption that men this young have a very low risk of osteoporosis and because most fractures result from higher trauma [11, 22]. We found that almost half of the men aged 20–39 suffered a low-trauma fracture compared to approximately 1/10 in earlier studies [22]. This was unexpected but unlikely to be explained by recall bias within the time frame and there was no difference in BMD with degree of trauma.
Younger men have not previously been considered a risk group suggesting that the association between low bone density and fracture needs to be further studied in men below the age of forty to understand the underlying pathophysiology. Skeletal structure may play a role, a study of elderly men by pQCT indicated bone width as an predictor of fragility fractures independent of BMD [23]; however, this was not available in the present study. The cause of fragility fracture is multifactorial, the occurrence of a fall being the strongest risk factor, but further studies are required to understand the propensity to falls also in the younger population and the relationship to BMD and fractures. Apparent from our study, there is need for clinical investigation of BMD and risk of future fractures in men with distal radius fracture; despite a possible higher level of trauma, it cannot be precluded that compromised bone strength, is contributing to these fractures in men, as indicated by a higher prevalence of osteoporosis also in those below 65.
This finding is of importance in terms of understanding patterns of osteoporotic fracture risk in men. Compared to women, only a small proportion of men at risk of osteoporosis are evaluated and receive treatment [24, 25]. By raising awareness of the higher prevalence of osteoporosis in men with distal radius fracture, we might reduce the risk of future major fractures such as hip fracture, which in men causes higher mortality than in women [9].
A major strength of this work is that we have performed the largest comparative BMD study in male patients with distal radius fracture against a background population. We have covered the full spectrum of ages and are also the first to have specifically investigated the often overlooked group of younger men below the age of forty. We included all radius fractures regardless of trauma level, based on our hypothesis that men whose distal radius fracture resulted from moderate- or high-energy trauma may have impaired bone strength [11]. Limitations are acknowledged, among these the 40–50 % response rate; although there was no difference in age distribution between responders and non-responders there is always a risk of selection bias in cohort studies. Our participation rate is, however, similar to that of equivalent studies. This also pertains to the controls, who may attend both because they are healthier or less healthy depending on reason for agreeing to participate, but inherent to most studies. We recognize as a limitation that important confounding factors for fracture, namely history of falls and family history of osteoporosis could not be included in the analyses, as a consequence of the fact that the controls were not specifically collected for this present study.
The long inclusion period is unlikely to affect the results since a homogeneous environment and personnel were maintained throughout. While a fracture occasion can lead to a lifestyle change altering osteoporosis risk, we consider this unlikely since only two variables (BMI and oral steroid use) differed between the retro- and prospective arms of the study while BMD was similar for both. The prevalence of distal radius fracture was not available in the control group, but we believe that this only strengthens our results, since excluding controls, with previous distal radius fractures, would most likely enhance the statistical difference in BMD bearing in mind the earlier findings.
The results from this study suggest, despite the described limitations, that men aged 40 and over who suffer a distal radius fracture have lower BMD and are at increased risk of skeletal fragility. Even in the younger men, a trend toward a higher risk of osteoporosis was apparent. Presentation of a distal radius fracture regardless of trauma level indicates that screening for osteoporosis and risk of future fractures should be considered.
References
Cummings SR, Kelsey JL, Nevitt MC, O’Dowd KJ (1985) Epidemiology of osteoporosis and osteoporotic fractures. Epidemiol Rev 7:178–208
Cuddihy MT, Gabriel SE, Crowson CS, O’Fallon WM, Melton LJ 3rd (1999) Forearm fractures as predictors of subsequent osteoporotic fractures. Osteoporos Int 9:469–475
Mallmin H, Ljunghall S, Persson I, Naessén T, Krusemo UB et al (1993) Fracture of the distal forearm as a forecaster of subsequent hip fracture: a population-based cohort study with 24 years of follow-up. Calcif Tissue Int 52:269–272
Nellans KW, Kowalski E, Chung KC (2012) The Epidemiology of distal radius fractures. Hand Clin 28:113–125
Mallmin H, Ljunghall S (1992) Incidence of Colles’ fracture in Uppsala. A prospective study of a quarter-million population. Acta Orthop Scand 63:213–215
Wilcke MKT, Hammarberg H, Adolphson PY (2013) Epidemiology and changed surgical treatment methods for fractures of the distal radius: a registry analysis of 42,583 patients in Stockholm County, Sweden, 2004–2010. Acta Orthop 84:292–296
Haentjens P, Johnell O, Kanis JA, Bouillon R, Cooper C et al (2004) Evidence from data searches and life-table analyses for gender-related differences in absolute risk of hip fracture after Colles’ or spine fracture: Colles’ fracture as an early and sensitive marker of skeletal fragility in white men. J Bone Miner Res 19:1933–1944
Ismail AA, Pye SR, Cockerill WC, Lunt M, Silman AJ et al (2002) Incidence of limb fracture across Europe: results from the European Prospective Osteoporosis Study (EPOS). Osteoporos Int 13:565–571
Cummings SR, Melton LJ (2002) Epidemiology and outcomes of osteoporotic fractures. Lancet 359:1761–1767
Järvinen TLN, Sievänen H, Khan KM, Heinonen A, Kannus P (2008) Shifting the focus in fracture prevention from osteoporosis to falls. BMJ 336:124–126
Tuck SP, Raj N, Summers GD (2002) Is distal forearm fracture in men due to osteoporosis? Osteoporos Int 13:630–636
Lee DM, Pye SR, Tajar A, O’Neill TW, Finn JD et al (2013) Cohort profile: the European Male ageing study. Int J Epidemiol 42:391–401
Callréus M, McGuigan F, Akesson K (2014) Country-specific young adult dual-energy X-ray absorptiometry reference data are warranted for T-score calculations in women: data from the peak-25 cohort. J Clin Densitom 17:129–135
Looker AC, Orwoll ES, Johnston CC, Lindsay RL, Wahner HW et al (1997) Prevalence of low femoral bone density in older U.S. adults from NHANES III. J Bone Miner Res 12:1761–1768
Khosla S, Amin S, Orwoll E (2008) Osteoporosis in men. Endocr Rev 29:441–464
Abrahamsen B, van Staa T, Ariely R, Olson M, Cooper C (2009) Excess mortality following hip fracture: a systematic epidemiological review. Osteoporos Int 20:1633–1650
Øyen J, Rohde G, Hochberg M, Johnsen V, Haugeberg G (2011) Low bone mineral density is a significant risk factor for low-energy distal radius fractures in middle-aged and elderly men: a case-control study. BMC Musculoskelet Disord 12:67
Risto O, Hammar E, Hammar K, Fredrikson M, Hammar M et al (2012) Elderly men with a history of distal radius fracture have significantly lower calcaneal bone density and free androgen index than age-matched controls. Aging Male 15:59–62
Sharma S, Fraser M, Lovell F, Reece A, McLellan AR (2008) Characteristics of males over 50 years who present with a fracture: epidemiology and underlying risk factors. J Bone Joint Surg Br 90:72–77
Øyen J, Gjesdal CG, Brudvik C, Hove LM, Apalset EM et al (2010) Low-energy distal radius fractures in middle-aged and elderly men and women–the burden of osteoporosis and fracture risk: a study of 1794 consecutive patients. Osteoporos Int 21:1257–1267
Oyen J, Brudvik C, Gjesdal CG, Tell GS, Lie SA et al (2011) Osteoporosis as a risk factor for distal radial fractures: a case-control study. J Bone Joint Surg Am 93:348–356
Lindau TR, Aspenberg P, Arner M, Redlundh-Johnell I, Hagberg L (1999) Fractures of the distal forearm in young adults. An epidemiologic description of 341 patients. Acta Orthop Scand 70:124–128
Szulc P, Munoz F, Duboeuf F, Marchand F, Delmas PD (2006) Low width of tubular bones is associated with increased risk of fragility fracture in elderly men—the MINOS study. Bone 38:595–602
Kiebzak GM, Beinart GA, Perser K, Ambrose CG, Siff SJ et al (2002) Undertreatment of osteoporosis in men with hip fracture. Arch Intern Med 162:2217–2222
Harper CM, Fitzpatrick SK, Zurakowski D, Rozental TD (2014) Distal radial fractures in older men: a missed opportunity? J Bone Joint Surg Am 96:1820–1827
Acknowledgments
This work was supported by grants from the Swedish Research Council (K2012-52X-14691-10-3), FAS (2007-2125), Greta and Johan Kock Foundation, A. Påhlsson Foundation, A. Osterlund Foundation, the H Järnhardt foundation, King Gustav V and Queen Victoria Foundation, The Swedish Rheumatism Association, Skåne University Hospital Research Fund, Research and Development Council of Region Skåne, Sweden; Commission of the European Communities Fifth Framework Programme ‘Quality of Life and Management of Living Resources’ Grant QLK6-CT-2001-00258.
Author’s Contribution
Lisa Egund and Fiona McGuigan were responsible for the statistical analysis and interpretation of data and Lisa Egund prepared the first draft of this paper. Karin Önnby designed the study and with Aleksander Giwercman was responsible for the acquisition of data. Kristina Akesson designed the study and is guarantor. All authors revised the paper critically for intellectual content and approved the final version. All authors agree to be accountable for the work and to ensure that any questions relating to the accuracy and integrity of the paper are investigated and properly resolved.
Funding
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Lisa Egund, Fiona McGuigan, Karin Önnby, Aleksander Giwercman, and Kristina Akesson declare that they have no conflict of interest.
Human and animal rights statements
All procedures performed in this study involving human participants were in concordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Egund, L., McGuigan, F., Önnby, K. et al. High Prevalence of Osteoporosis in Men with Distal Radius Fracture: A Cross-Sectional Study of 233 Men. Calcif Tissue Int 99, 250–258 (2016). https://doi.org/10.1007/s00223-016-0142-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-016-0142-6