Abstract
This case-control epidemiologic study examines the relationship between hormone replacement therapy (HRT) and risk for fractures of four sites among women 45 years of age and older. From October 1996 to May 2001, incident patients with distal forearm (n=744), foot (n=618), proximal humerus (n=331), and pelvis (n=109) fractures were recruited from five Kaiser Permanente Medical Centers in northern California. Controls (n=1617) were selected at random from the same five medical centers over the same time period within strata defined by 5-year age group, gender, and white versus nonwhite or unknown recorded race/ethnicity. Trained interviewers collected information using a standardized questionnaire. Compared with postmenopausal women who never used HRT, postmenopausal women currently using HRT for at least 3 months had a decreased risk of fracture at the distal forearm (adjusted OR=0.55, 95% CI: 0.43, 0.72), proximal humerus (adjusted OR=0.51, 95% CI: 0.36, 0.74), and pelvis (adjusted OR=0.51, 95% CI: 0.27, 0.95), but not the foot (adjusted OR=1.05, 95% CI: 0.81, 1.35). Past use of HRT for more than 7 years also appeared to be associated with a reduced risk of fracture at the distal forearm and proximal humerus. The longer a woman went without HRT after her last menstrual period, the greater her risk of fracture in the distal forearm, proximal humerus, and pelvis. The findings of this study support long-term, current use of HRT for the prevention of osteoporotic fractures, but other risks and benefits also need to be considered.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Many observational studies have found reductions in the risk for hip, vertebral, and distal forearm fractures with the use of hormone replacement therapy (HRT) [1]. The few randomized controlled trials evaluating the role of HRT on fracture risk have found reductions in vertebral, distal forearm, hip, and all nonvertebral fractures [1, 2, 3]. A meta-analysis of randomized controlled trials found a 27% reduction in risk of all nonvertebral fractures and a 40% reduction in hip and wrist fractures associated with the assignment of HRT [4]. However, one randomized controlled trial did not find reductions in the incidence of fractures (a secondary endpoint in that trial) with HRT use [5].
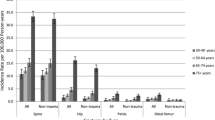
Although HRT has been associated with a reduction in risk for distal forearm fractures in previous observational studies [6, 7, 8, 9], documentation of HRT-associated effects on fracture risk in the foot, proximal humerus, and pelvis is limited even though the incidence rate for these four fractures is about 8/1000 per year in men and women 35 years of age and older [10]. One study reported a 30% fracture risk reduction at the proximal humerus with HRT use [7]. Another study on the same cohort did not find an association between HRT and foot fracture [11]. The impact of HRT on pelvis fractures remains unknown.
The objective of this analysis is to determine whether HRT use is associated with a reduction in the risk for fractures of the foot, distal forearm, proximal humerus, and pelvis. HRT is generally believed to affect cancellous bone to a greater extent than cortical bone because of the higher surface-to-volume ratio [12]. Because the pelvis, proximal humerus, and foot have both types of bone, and the distal forearm has primarily cancellous bone [13], it was hypothesized that HRT would be beneficial to all four fracture sites but would have the largest effect on the distal forearm. We hypothesized that HRT would have the least effect on foot fractures because they are less strongly associated with low bone mineral density [11]. The case-control study from which these data were derived was not designed specifically to assess the effect of HRT on fractures, but sought to identify a variety of possible risk factors for fractures in persons aged 45 years and older at five fracture sites.
Patients and methods
Five northern California Kaiser Permanente Medical Centers (Hayward, Oakland, San Francisco, Santa Clara, and South San Francisco) participated in this case-control study. The Institutional Review Boards of Kaiser Permanente and Stanford University approved this project and its informed consent procedures. Cases and controls for this analysis were identified from November 1996 through May 2001.
On a weekly basis, patients with fractures of the distal forearm, foot, proximal humerus, pelvis, or shaft of the tibia/fibula and aged 45 years and older were identified through computerized radiology reports and hospital inpatient and outpatient reports at each of the five Kaiser Permanente facilities. A trained record abstractor obtained information on the fracture site from radiology reports and medical records. To be included as a case, the fracture had to be confirmed by X-ray, bone scan, or MRI. Fractures classified as possible or suspicious were not accepted, unless there was X-ray evidence of fracture healing within 3 weeks. Classification of fractures followed the International Statistical Classification of Diseases and Related Health Problems, 10th revision [14]. Fractures of the distal forearm included those in the distal third of the radius, ulna, or both, while fractures of the proximal humerus included those at the level of or proximal to the surgical neck of the humerus. Fractures of the foot include the bones of the foot (eg talus, navicular, cuboid, cuneiform, and metatarsal), but not the toes or ankle. Fractures of the pelvis included all pelvic bones (eg sacrum, ileum, pubis, acetabulum, and ischium) except the coccyx. Data on one additional fracture site was collected, shaft of the tibia/fibula, but the results are not presented here because of the relatively small number of cases (n=83). Women could only be a case at one site. For this analysis, the first-listed fracture on the medical record was taken as the fracture site for individuals with simultaneous fractures at more than one of these sites (n=31).
In order to include relatively large numbers of racial/ethnic minorities for other purposes of this study, all persons indicated as a minority or with an unknown race/ethnicity on computerized hospital inpatient files and medical records were invited to participate in the study for all five fracture sites. Because pelvis fractures were uncommon, all whites were invited to participate. At the other fracture sites, only a percentage of persons indicated as whites were sampled: 50% with proximal humerus and distal forearm fractures and 25% with foot fractures through April 30, 2000. Starting on May 1, 2000, in order to increase the sample size, 100% of whites with distal forearm fractures and 50% of the whites with foot and proximal humerus fractures were invited to participate. It should be noted that final classification of race/ethnicity was based on self-report from the questionnaire. Some 73% of eligible patients agreed to participate.
Controls
The 1614 controls were accrued over the same time period as cases. Every 3 months, 25% of Kaiser members from the five centers in the age group 45 years and older were randomly sampled, and stratified into nine 5-year age groups (45–49, 50–54, 55–59, 60–64, 65–69, 70–74, 75–79, 80–84, 85+). The selected Kaiser members were then randomly ordered, and the first 34 women in each 5-year age group were retained. Race/ethnicity, if available, was ascertained for the potential controls from Kaiser records. All minorities, all individuals of unknown race/ethnicity, and a random sample of 39% of white women were selected. Women previously selected as cases were not eligible to be controls. Some 66% of eligible controls agreed to participate.
Exclusions
Subjects who required the use of proxy respondents because they died or had cognitive impairment, defined as a score of ten or greater on the Blessed Orientation-Memory-Concentration Test [15] or based on the interviewer's judgment, were excluded from these analyses (n=146). Patients who fractured their bone in a motor vehicle accident (n=69) and cases or controls who said that they took HRT for the prevention or treatment of osteoporosis were excluded from these analyses (n=232). Potential cases with pathologic fractures caused by specific diseases, such as metastatic cancer or Paget's disease, and controls with these same diseases were excluded.
In order to study incident fractures, patients with a history of fracture since the age of 45 years at the same site as that for which they were selected were excluded from the analysis (n=139), and controls with a prior fracture since the age of 45 years at any of the four fractures sites were excluded from the common control group (n=109). The common control group refers to the one control group used for all case-control comparisons presented in this paper.
Questionnaire
Most information on potential risk factors was obtained from a standardized questionnaire administered by trained interviewers in English or Spanish. For cases, questions referred to the period before the fracture occurred, while for controls, questions referred to the period before the time of the interview. Back-translation was used to assure that the English and Spanish versions of the questionnaire were equivalent. For the first 3 years of the study, the interview was conducted primarily in person at the subject's home (or institution, for institutionalized subjects) or rarely in another place of convenience. To increase participation rates and the number of subjects interviewed, the interview was conducted primarily over the telephone after November 15, 2000. Overall, 52% of interviews were conducted in person. Whether a study subject was interviewed in person or over the telephone was assessed as an effect modifier for each HRT and fracture association in the multivariate analyses. No evidence of effect modification from this source was found.
Only HRT taken for at least 3 months continuously was included. HRT used for birth control was not counted. The HRT questions were from the Women's Health Initiative [3]. Women were asked about the duration and type of estrogen and progestogen used, and their age when they started and stopped using each HRT. When the questionnaire was conducted in person, interviewers showed the women pictures of estrogen and progestogen pills. The prevalence of use of HRT and odds ratios were similar in the two types of interviews.
The measures of HRT presented in this paper are ever use of HRT continuously for at least 3 months (yes/no); use of HRT in the last month and continuously for at least 3 months (yes/no); total years of HRT use; years since last use of HRT; and estimated total number of postmenopausal years without use of HRT. If a woman had never used HRT, the time since last use of HRT was taken to be her current age minus age at last menstrual period. Twenty-six women were excluded because of missing values of the age they last stopped using HRT. Total postmenopausal years without HRT use refers to the number of years that a woman went without HRT after her last menstrual period. This was estimated by calculating the number of years since the last menstrual period for each woman (current age minus age at last menstrual period), then subtracting the total years she was on HRT.
Women with missing or 'don't know/refused to answer' values of the HRT measures were assumed not to have used HRT. Missing values of age at last menstrual period were assigned an age of last menstrual period of 51.4, the mean age of menopause in a multiethnic community study population [16]. Women with a hysterectomy and at least one intact ovary were also assigned an age at last menstrual period of 51.4 or the date they began HRT use because their age at the last menstrual period reflects the date of their hysterectomy, not the date of menopause. Some women began HRT before their menstrual periods ended; these women were assigned an age at last menstrual period as the age they started using HRT. The percentage of women assigned an age at last menstrual period of 51.4 was 12% for both cases and controls. When the analyses were repeated excluding those where age at last menstrual period was unknown, the measures of association did not change by more than 10%.
The following questionnaire-derived variables were assessed as potential confounders in the multivariate analyses: body mass index (kg/m2); history of maternal hip fracture and dowager's hump; self-reported overall health compared with others of her age; use of thiazides and related diuretics, calcium supplements, and seizure medications for at least once a week for a total of 1 year or longer; average weekly alcohol intake in the past year; average weekly leisure-time physical activity level in the past year; smoking status (current smoker, past smoker, or never smoker); type of menopause (hysterectomy, bilateral oophorectomy, or natural); number of fractures incurred since the age of 45 years; and number of falls during the prior year. Missing values for the components of the summary variables were given values of 'no' for binary response variables, the modal value for ordinal variables, and mean subgroup values by age, gender, and race/ethnicity for body mass index. Among all cases and controls, missing values occurred for less than 1% of women for most variables.
Statistical analysis
Odds ratios, which approximate the relative risk, were used as the measure of association between potential risk factors and fractures. To examine the association between a variable and fracture controlling for the effects of other variables, we used logistic regression with SAS version 8 software to compute adjusted odds ratios. The adjusted odds ratios took into account the 5-year age group, race/ethnicity as indicated by inpatient medical files to account for how the cases and controls were sampled, the type of interview (in person versus over the telephone), and additional variables listed in the footnotes to Tables 2 and 3. Variables were included in the multivariable models if they changed the odds ratios by more than 10% at any of the fracture sites, or if a priori hypotheses supported their inclusion.
Self-reported race/ethnicity was categorized into four groups on the basis of similarity of odds ratios for fractures: (1) white, Native American and other, (2) black, (3) Chinese, Filipino, Japanese, Pacific Islander and other Asians, and (4) Hispanic. The small number of subjects (n=120) who reported themselves as being in more than one racial/ethnic category were placed into a single category according to their answers to questions on their degree of acculturation.
For all the analyses presented in this paper, a common control group was used. However, for comparison, five unique control groups were also created by excluding only controls with prior fractures at the fracture site to which they were being compared, and the results were similar to those found with the common control group.
Possible effect modification of the associations between HRT use and fracture by age, type of interview, smoking status, body mass index, physical activity and alcohol consumption was assessed by stratification and cross-product terms in logistic regression. Little evidence of effect modification was present and will not be discussed further.
Results
Of the women who used HRT, over 75% used Premarin in various doses, and less than 10% used Estrace, the next most common regimen. Some 67% of women taking progestogens used Provera, and 17% used medroxyprogesterone. Of women with a hysterectomy, 93% took estrogen alone, and 91% of women without a hysterectomy took estrogen and progestogen, and the odds ratios associated with HRT use were similar in the hysterectomized and nonhysterectomized groups. In addition, the effect of current and past HRT use was assessed separately among women using estrogen alone versus women using estrogen plus progestogen, and the HRT and fracture associations were similar in these two groups. As a result, all estrogen and estrogen plus progestogen regimens were combined in the analysis. In addition, the dose of HRT in Premarin users was assessed. Over 75% of Premarin use involved the 0.625 mg dose, and the findings for duration of HRT and dose of HRT both reduced the odds ratio estimates, so the results on dose are not presented.
Selected characteristics of each case group and the controls are presented in Table 1. On average, the foot fracture cases were the youngest and proximal humerus and pelvis fracture cases the oldest. Most women first used HRT near the time of menopause. The age at last menstrual period was lower for ever users of HRT than women who never took HRT (45.7 vs 47.5). In general, age at last menstrual period was not associated with any of the fractures (data not shown). Pelvis fracture cases had the lowest body mass index and lowest percentage with natural menopause. A higher percentage of foot fracture cases and lower percentages of distal forearm and proximal humerus fracture cases had ever used HRT than controls. Distal forearm, proximal humerus, and pelvis cases were less likely to be current HRT users than controls. Women who were currently using HRT tended to have used HRT for at least twice as long as past users and had fewer postmenopausal years without HRT than past users (data not shown).
Adjusted odds ratios for the relationship between HRT use and fractures of the foot, distal forearm, proximal humerus, and pelvis are presented in Table 2. Having ever used HRT for 3 or more months was associated with a decreased risk of 35% for distal forearm, 37% for proximal humerus, and 28% for pelvis fractures, but had no effect on foot fractures. When subjects were categorized into current users, past users, and never users, current use was associated with a reduced risk for distal forearm, proximal humerus, and pelvis fractures of 45%, 49%, and 49%, respectively, but had no effect on foot fractures. Past use (not considering length of use) was associated with at most a slightly reduced risk of fractures of the distal forearm and proximal humerus.
The greater the amount of time a woman did not take HRT in her postmenopausal years, the greater her risk for fractures in the distal forearm, proximal humerus, and pelvis (Table 2). For every 5 years a woman went without HRT after her last menstrual period, her odds increased by 18% for distal forearm, 24% for proximal humerus, and 12% for pelvis fractures. Although the number of postmenopausal years without HRT and duration of HRT measure highly correlated characteristics of HRT use, the number of postmenopausal years without HRT is presented because it approximates the amount of time that bone was exposed to only minimal estrogen. The risk for fractures of the distal forearm, proximal humerus, and pelvis increased with the amount of time since last use of HRT, even after controlling for total length of HRT use in addition to age, race/ethnicity, type of interview, body mass index, and type of menopause.
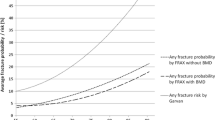
The relationship between risk for fracture and timing and duration of HRT use is presented in Table 3. Currently using HRT for a total of 7 years or more (the median duration of HRT use among HRT users in the control group) was associated with a reduced risk of distal forearm fracture of 58%, proximal humerus fracture of 56%, and pelvis fracture of 43%, while current use of HRT for a total of fewer than 7 years showed a slight reduction in risk for the distal forearm and proximal humerus, but a greater reduction for the pelvis. Although the confidence intervals are wider in past users, past use of HRT for a total of more than 7 years showed greater reductions in risk (except at the pelvis) than past use for a total of fewer than 7 years, which showed no reduced risk for fracture at any site. Figure 1 shows how the multivariate-adjusted odds ratios decrease with fewer postmenopausal years without HRT.
Adjusted odds ratios and 95% confidence intervals for foot, distal forearm, proximal humerus, and pelvis fractures by quartiles of postmenopausal years without hormone replacement therapy (HRT); the quartile with the largest duration, ≧22 years, serves as the reference group (quartiles are based on the distribution in the control group) [adjusted for 5-year age group, inpatient medical files race/ethnicity (white, nonwhite or unknown), type of interview (in person versus over the telephone), age in years, self-reported race/ethnicity, body mass index, and type of menopause (hysterectomy, bilateral oophorectomy, or natural)]
Discussion
Our findings and those of others [1, 6] suggest that current use of HRT is associated with protection against distal forearm, proximal humerus, and pelvis fractures. For the most part, long-term, current users showed the largest reduction in risk. In addition, the risk for fractures in the distal forearm, proximal humerus, and pelvis increased each year a woman was not using HRT after menopause. In our study, women who used HRT generally started at menopause, and current users took HRT for at least twice as long and had fewer postmenopausal years without HRT than past users. Beginning HRT near the time of menopause and continuing its use indefinitely appears to provide maximal protection against BMD loss and osteoporotic fractures [1].
It is well established that women experience a rapid loss of bone after menopause [17]. Among women taking estrogen, rates of bone resorption and formation have been found to return to premenopausal values [17] and are approximately one-third that of nonusers [18]. However, once women stop using HRT, bone loss returns to the initial, accelerated postmenopausal rate [18, 19], and the protective effect of HRT on fracture risk diminishes [1, 8]. Thus, both duration and timing of HRT seem to be important for fracture prevention.
HRT afforded no protection against foot fractures. Studies have documented improvements in the heel ultrasound stiffness index with HRT [20, 21], but the associations between the ultrasound stiffness index and foot fractures were not assessed in these studies. In the Study of Osteoporotic Fractures, each standard deviation decrease in calcaneal bone mineral density was only weakly associated with foot fractures (RR=1.12, 95% CI: 0.97, 1.29), and HRT was not associated with a reduction in risk for foot fractures [11].
The limitations of our study are, first, as with many case-control studies, inaccurate reporting of prior events such as HRT use could have occurred. A validation study at Kaiser Permanente of self-reported HRT use in the month before the fracture for cases and the month before interview for controls was conducted to determine the association between self-reported HRT use and HRT prescriptions being filled at Kaiser Permanente. Some 79% of cases and controls who said they used HRT in the last month had a prescription filled in that period, and almost 90% of these women had a prescription filled for HRT in the prior 90 days. These percentages are likely to be underestimates because a small number of women fill their prescriptions at other pharmacies.
It has been suggested that some of the beneficial effects of HRT seen in nonexperimental studies can be explained by selection bias [22] or uncontrolled confounding. That is, healthier women may be choosing to take HRT, and HRT use may be a marker of socioeconomic, clinical, or lifestyle factors that put women at a lower risk of fracture. We controlled as best we could for the possible confounding variables we measured, such as physical activity or the presence of certain diseases, but uncontrolled confounding cannot be ruled out. In a recent meta-analysis of randomized controlled trials, Torgerson and Bell-Syer [4] found a 40% reduction in 'wrist' fractures with HRT. This value is similar to our results for the association between current use of HRT and distal forearm fractures, suggesting that selection bias may not have played a large role in our study. Also, the lower response rate in the control group may be a limitation, especially if HRT use was related to nonresponse in the controls and not the cases. This does not appear to be the situation in our study, as the foot fracture cases had similar patterns of HRT use as controls, and our findings on current HRT use and distal forearm fractures were similar to the meta-analysis discussed above [4].
Women interviewed in person were shown pictures of HRT pills, while subjects interviewed over the telephone were not. This could bias our results because those subjects interviewed in person could give more accurate answers than those interviewed over the telephone. However, the odds ratios for the HRT measures did not vary by type of interview. Finally, age at menopause had to be imputed for 12% of cases and controls, but excluding these women did not change the associations between HRT and fracture.
On the other hand, patients were interviewed shortly after the fracture in order to collect more accurate and detailed information than if more time had elapsed. The subjects used in this study had equal access to health care because they were all enrolled in the same health plan. We also excluded women who used HRT for the prevention or treatment of osteoporosis so as to avoid underestimation of the benefits of HRT on fractures [23].
In summary, the hypothesis of this study was that HRT would be beneficial to all four fracture sites, but would have the largest effect on the distal forearm and the least effect on foot fractures. This observational study suggests that current HRT use in postmenopausal women reduces the risk for fractures of the distal forearm, proximal humerus, and pelvis to a similar extent, and does not reduce the risk for fractures of the foot. The risk for fractures in the distal forearm, proximal humerus, and pelvis increases with the time since last HRT use and with greater time that a woman has been without HRT after her final menstrual period. The findings of this study support the long-term, current use of HRT for the prevention of osteoporotic fractures, but other benefits and risks also need to be considered.
References
Cauley JA, Salamone LM (2001) Postmenopausal endogenous and exogenous hormones, degree of obesity, thiazide diuretics, and risk of osteoporosis. In: Marcus R, Feldman D, Kelsey JL (eds) Osteoporosis, 2nd edn, Vol 1. Academic Press, San Diego, pp 741–769
Mosekilde L, Beck-Nielsen H, Sorensen OH, Nielsen SP, Charles P, Vestergaard P, Hermann AP, Gram J, Hansen TB, Abrahamsen B, Ebbesen EN, Stilgren L, Jensen LB, Brot C, Hansen B, Tofteng CL, Eiken P, Kolthoff N (2000) Hormone replacement therapy reduces forearm fracture incidence in recent postmenopausal women—results of the Danish Osteoporosis Prevention Study. Maturitas 36:181–193
Writing Group for the Women's Health Initiative Investigators (2002) Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principle results from the Women's Health Initiative randomized controlled trial. JAMA 288:321–333
Torgerson DJ, Bell-Syer SEM (2001) Hormone replacement therapy and prevention of nonvertebral fractures: a meta-analysis of randomized trials. JAMA 285:2891–2897
Hully S, Furberg C, Barrett-Connor E, Cauley J, Grady D, Haskell W et al (2002) Noncardiovascular disease outcomes during 6.8 years of hormone therapy: the Heart and Estrogen/progestin Replacement Study follow-up (HERS II). JAMA 288:58–66
Cauley JA, Seeley DG, Ensrud K, Ettinger B, Black D, Cummings SR, Study of Osteoporotic Fractures Research Group (1995) Estrogen replacement therapy and fractures in older women. Ann Intern Med 122:9–16
Kelsey JL, Browner WS, Seeley DG, Nevitt MC, Cummings SR (1992) Risk factors for fractures of the distal forearm and proximal humerus. Am J Epidemiol 135:477–489
Weiss NS, Ure CL, Ballard JH, Williams AR, Daling JR (1980) Decreased risk of fractures of the hip and lower forearm with postmenopausal use of estrogen. N Engl J Med 303:1195–1198
Williams AR, Weiss NS, Ure CL, Ballard J, Daling JR (1982) Effect of weight, smoking, and estrogen use on the risk of hip and forearm fractures in postmenopausal women. Obstet Gynecol 60:695–699
Melton LJ III, Crowton CS, O'Fallon WM (1999) Fracture incidence in Olmsted County, Minnesota: comparison of urban with rural rates and changes in urban rates over time. Osteoporosis Int 9:29–37
Seeley, DG, Kelsey J, Jergas M, Nevitt MC (1996) Predictors of ankle and foot fractures in older women. J Bone Miner Res 11:1347–1355
Lindsay R, Cosman F (2001) Estrogens and osteoporosis. In: Marcus R, Feldman D, Kelsey JL (eds) Osteoporosis, 2nd edn, Vol 2. Academic Press, San Diego, pp 577–601
Riggs BL, Khosla S, Melton JL III (2001) The type I/type II model for involutional osteoporosis. In: Marcus R, Feldman D, Kelsey JL (eds) Osteoporosis, 2nd edn, Vol 2. Academic Press, San Diego, pp 49–58
WHO (1992) International Statistical Classification of Diseases and Health Related Problems, 10th revision, Vol 1. World Health Organization, Geneva
Katzman R, Brown T, Fuld P, Peck A, Schechter R, Schimmel H (1983) Validation of a short orientation-memory-concentration test of cognitive impairment. Am J Psychiatry 140:734–739
Gold EB, Bromberger J, Crawford S, Samuels S, Greendale GA, Harlow SD, Skurnick J (2001) Factors associated with age at natural menopause in a multi-ethnic sample of midlife women. Am J Epidemiol 153:865–874
Gallagher JC (1996) Estrogen: prevention and treatment of osteoporosis. In: Marcus R, Feldman D, Kelsey JL (eds) Osteoporosis. Academic Press, San Diego, pp 1191–1208
Quigley MET, Martin PL, Burnier AM, Brooks P (1987) Estrogen therapy arrests bone loss in elderly women. Am J Obstet Gynecol 156:1516–1523
Tremollieres FA, Pouilles JM, Ribot C (2001) Withdrawal of hormone replacement therapy is associated with significant vertebral bone loss in postmenopausal women. Osteoporosis Int 2001:385–390
Hadji P, Hars O, Schuler M, Block K, Wuster C, Emons G, Schulz K (2000) Assessment by quantitative ultrasonometry of the effects of hormone replacement therapy on bone mass. Am J Obstet Gynecol 182:529–534
Weiss M, Ben Shlomo A, Hagag P, Rapoport M, Ish-Shalom S (2000) Effect of estrogen therapy on speed of sound at multiple skeletal sites. Maturitas 35:237–243
Matthews KA, Kuller LH, Wing RR, Meilahn EN, Plantinga P (1996) Prior to use of estrogen replacement therapy, are users healthier than nonusers? Am J Epidemiol 143:971–978
Cummings SR, Nevitt MC, Browner WS, Stone K, Fox KM, Ensrud KE, Cauley J, Black D, Vogt TM (1995) Risk factors for hip fracture in white women. N Engl J Med 332:767–773
Acknowledgements
Supported by grants from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (RO1 AR42421 and T32 AR07588). We thank Beverly Peters and Luisa Hamilton for project management, Michael Sorel for computing and database management, and Carolyn Salazar for medical record abstraction.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Keegan, T.H.M., Gopalakrishnan, G., Sidney, S. et al. Hormone replacement therapy and risk for foot, distal forearm, proximal humerus, and pelvis fractures. Osteoporos Int 14, 469–475 (2003). https://doi.org/10.1007/s00198-003-1379-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-003-1379-2