Abstract
Introduction
The primary objective of this study is to determine the prevalence of overactive bladder (OAB) and detrusor overactivity (DO) in female patients who were referred for urodynamic study (UDS) because of lower urinary tract symptoms (LUTS). The secondary objective is to determine the subjective and objective differences between female OAB patients with and without DO.
Materials and methods
All female patients who underwent UDS for LUTS between June 2016 and September 2019 were retrospectively reviewed. Personal history, medical history, physical examination, and validated questionnaires were collected. One-hour pad test and multichannel urodynamic study was performed. All statistical analyses were conducted by SAS 9.4. P-value < 0.05 was considered statistically significant.
Results
A total of 4184 female patients underwent UDS because of LUTS between June 2016 and September 2019; 1524 patients were analyzed for OAB or DO. The occurrence of OAB was 36.4%. The overall incidence of DO in OAB patients was 15.5%; 9.5% of all patients had DO findings on UDS, and 4.6% were incidental findings. There were significant differences among mean age, parity, ICIQ-UI SF, OABSS, POPDI-6, and all UDS parameters (except for maximal urethral pressure and pressure transmission ratio) between patients with and without DO. In patients with DO, there were no significant differences among age, parity, and BMI with or without OAB symptoms. However, there were significant differences among mean OABSS, ICIQ-UI SF, UDI-6, POPDI-6, IIQ-7, and pad test.
Conclusions
Patients with DO are associated with older age, increased parity, greater urine leakage, and worse storage and micturition functions on UDS. Combinations of subjective and objective measurements are better predictive models for OAB patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Overactive bladder (OAB) is defined by the International Continence Society (ICS) as a syndrome with “urinary urgency, usually accompanied by frequency and nocturia, with or without urinary incontinence, in the absence of urinary tract infection (UTI) or other obvious pathology” [1]. It is diagnosed clinically, based on the patient’s symptoms and history.
Urodynamic study (UDS) assesses patient’s lower urinary tract function while replicating the patient’s symptoms [2]. Detrusor overactivity (DO), defined as the occurrence of detrusor contraction during filling cystometry, is a demonstratable UDS finding correlating to OAB symptoms [1]. However, the etiology of OAB and DO is not well defined. Studies have shown more than half of the patients with OAB do not have DO detected on UDS [3]. There are controversies about whether OAB and DO are part of a spectrum of the same disease or if they are of an entirely different etiology [4]. The diagnosis of OAB is not dependent on presence of DO, and the presence of DO is not predictive of OAB.
There is an ongoing debate about whether treatment should be based on patient’s symptoms and clinical findings (such as voiding diary, residual urine, pelvic floor exam, etc.) or UDS findings. Most guidelines recommend patients to undergo UDS only if initial symptoms do not improve after conservative therapy because of the invasiveness of UDS and poor correlation with clinical symptoms [5]. However, a recent prospective study showed that not only the women who received consistent treatment with their UDS findings were more likely to find improvement of their bladder symptoms, but also the clinicians changed treatment management in patients with OAB complaints [6]. In addition, many patients have both storage and voiding problems, which may be multifactorial or related to each other [7]. OAB symptoms are not useful for predicting the presence of concurrent voiding dysfunction that may alter management; thus, UDS is necessary for diagnosis [8]. Serati et al. found 59.9% of patients clinically diagnosed with mixed urinary incontinence had pure urodynamic stress incontinence (USI), 25.9% of stress urinary incontinence (SUI) patients had DO, and 14.2% of SUI patients in fact had pure urgency urinary incontinence. Patient’s subjective symptoms are often unreliable, and objective measures such as UDS are needed for better assessment [9].
The primary objective of this study is to determine the prevalence of OAB and DO in female patients who were referred to our single tertiary teaching center gynecology department for UDS due to lower urinary tract symptoms (LUTS). The secondary objective is to determine the subjective and objective differences between OAB patients with and without urodynamically proven DO.
Materials and methods
Participants
All gynecologic female patients who underwent UDS in a single tertiary medical center for LUTS between June 2016 and September 2019 were retrospectively reviewed. Patients who complained of OAB symptoms and/or had the diagnosis of DO in the UDS were recruited. Those with incomplete data were excluded. This study was approved by the Chang Gung Memorial Foundation Institutional Review Board (IRB no. 201901269B0).
Procedures
Initial assessment comprised personal history, medical history, and physical examination. UDS was arranged for all patients who complained of LUTS.
One-hour pad test and multichannel urodynamic study with a filling rate of 70 ml/min at room temperature was performed according to ICS Standard Good Urodynamic Practices (ICS-GUP2016) [2]. The UDS device used was Solar Gold MMS (Medical Measurement B.V., Enschede, The Netherlands). The results of the study were reviewed by one of the four urogynecology specialists in our center. Detrusor overactivity is defined as involuntary detrusor contractions during filling cystometry [1].
All women were asked to complete the following validated questionnaires in Traditional Chinese on the day of the UDS: Overactive Bladder System Score (OABSS) [10], International Consultation on Incontinence Questionnaire for Urinary Incontinence-Short Form (ICIQ-UI SF) [11], Urogenital Distress Inventory Short Form (UDI-6) [12], Pelvic Organ Prolapse Distress Inventory-6 (POPDI-6) [13], Incontinence Impact Questionnaire-7 (IIQ-7) [12], Pelvic Organ Prolapse/Urinary Incontinence Sexual Function Questionnaire-12 (PISQ-12) [14], and Colorectal-Anal Distress Inventory-8 (CRADI-8) [13]. If the patient was illiterate, the questionnaires were read to them by family members or medical staff personnel.
Statistical analysis
Descriptive statistics were presented as mean with standard deviation. Independent t-test was performed to compare the two groups. A subsequent regression analysis was carried out, and three logistic regression models were generated from different perspectives. ROC (receiver-operating characteristic) analysis was used to assess the prediction performance among the generated models. All statistical analyses were conducted by SAS 9.4. P < 0.05 was considered statistically significant.
Results
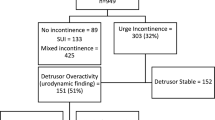
From June 2016 to September 2019, 4184 patients underwent UDS for LUTS (Fig. 1). After exclusion of patients with incomplete records and who did not complain of OAB symptoms or had DO diagnosis, 1524 patients were analyzed.
Primary outcomes
There were 1125 patients who complained of OAB without associated DO; 207 patients had OAB with DO, and 192 patients had incidental DO on UDS (Fig. 1). The overall incidence of DO in patients with OAB was 15.5%. In all patients with LUTS, the occurrence of OAB was 36.4%; 9.5% of all LUTS patients had DO findings on UDS, and the incidental finding of DO was 4.6%.
Secondary outcome
Of the 1524 patients, 399 had DO diagnosed on the UDS. Comparison between patients with and without DO is depicted in Table 1. There are significant differences between the mean age (66.4 vs 55.9 years old, P < 0.001) and parity number (3.31 vs 2.57, P < 0.001). There are no significant differences in BMI between the two groups.
Subjectively, there are significant differences in ICIQ-UI SF, OABSS, and POPDI-6 overall score. Except for maximal urethral pressure and pressure transmission ratio, all other urodynamic parameters have significant differences between the two groups.
Multiple logistic regression analysis was performed by a stepwise variable selection algorithm. Variables which were significant in univariate analyses was considered in the modeling process. Table 2 shows the three logistic regression models for DO of patients with OAB. The first model (Model I) consists of noninvasive parameters, including personal and medical history, pad test, and uroflow study. The second model (Model II) consists of only objective parameters including pad test and UDS. The third model (Model III) consists of all subjective and objective parameters. The area under the ROC curve (AUROC) indicates the predictive accuracy of the model (Fig. 2). Model III is significantly better than the other 2 models (AUROC 1 = 0.8203, 2 = 0.7954, 3 = 0.8640, p < 0.0001) in prediction performance.
A subsequent analysis of all patients with DO (with and without symptoms) is shown in Table 3. Patients with and without OAB symptoms did not differ significantly with age, parity, and BMI. There are significant differences among the mean OABSS, ICIQ-UI SF, UDI-6, POPDI-6, IIQ-7, and pad test.
In the studied patient population, 13.5% had advanced pelvic organ prolapse (POP) and another 6.7% underwent pelvic reconstructive surgery; 63.2% of the patients had both OAB and SUI symptoms. Only 4.1% had both DO and USI on UDS; 45.3% patients had OAB symptoms with USI on UDS, and 17.5% had SUI symptoms and DO on UDS.
Discussion
The etiology of OAB is unclear. Many consider DO an underlying pathophysiology of OAB while others have proposed that the cause of OAB may be multifactorial with different phenotypes [15]. Our results showed the total incidence of DO in all LUTS patients was 9.5%; 15.5% of OAB patients had urodynamically proven DO during filling cystometry. This is less compared to previous reporting, where nearly half of OAB patients have DO [6].
The detection rate of DO differs with different methods of UDS. Ambulatory UDS and lower physiological filling rate have a greater DO detection rate than conventional UDS [15]. When the filling capacity was stopped at 500 ml during UDS, 16% of patients with DO would be missed [16]. In our study, we used a filling rate of 70 ml/min on a conventional UDS, which is greater than the physiological diuresis and may account for the lower DO detection rate. Higher filling rates cause mechanical trauma to the receptors, nerve endings, muscle cells, and cell junctions, thereby impairing detrusor contractility [17]. Second, our study did not differentiate patients with only urgency symptoms from those with urgency urinary incontinence. With urgency urinary incontinence being on the more severe end of the spectrum, it can be expected to have a higher associated rate of DO. Patient’s understanding of “urgency” sensation may differ, and the presence of such symptoms may be overestimated, resulting in lower overall DO rate. It is reasonable to expect that patients treated at a tertiary medical center would reflect the severe end of the population. However, the national health care system in Taiwan does not require referral, and receiving treatment at a tertiary medical center is as affordable and accessible as that at a community hospital. This may in turn dilute the prevalence of DO in OAB patients and in fact reflect the true prevalence in the general population in Taiwan.
The prevalence of OAB was found greater in patients with POP [18]. Interestingly, OAB actually occurred more often in women with a less advanced stage of prolapse [19]. Most patients who come to our center because of POP have advanced stage and are seeking surgical treatment since such surgeries are not readily available in community hospitals. In this study, 20.2% of the patients had either advanced POP or had already undergone pelvic reconstructive surgery. This may provide insight into why our patients with DO/DOI scored lower on POPDI-6. However, further studies are needed to investigate the causative relationship between POP and OAB.
Historically, OAB was believed to be a motor disorder where patient-reported sensation or urinary urgency is the result of concomitant involuntary detrusor contraction [20]. Guralnick et al. found that patients with DO were older, had smaller maximal voided volumes, and had abnormal sensation [21]. Our findings were similar. Patients with DO were older with increased parity. Motor functions of DO patients were significant for lower peak flow rate, decreased voiding volume, and increased residual urine. Yet, modulation of unmyelinated afferent C fibers with capsaicin and lidocaine has been shown to reduce DO in induced OAB of animal models [22]. This suggests that afferent signals (sensory component) also contribute to the etiology of OAB [20]. We have found that OAB patients with DO have significant small first desire to void volume and maximal cystometric capacity compared with those without DO.
When comparing DO patients with and without OAB symptoms, there were only significant differences in pad test and total profile area of urethral profile pressure objectively. However, the subjective questionnaires showed significant difference between the two groups. This raises the question of why patients with similar characteristics have such different perceptions. The infamous saying of “the bladder is an unreliable witness” simply means that LUTS do not correlate with the underlying pathophysiology [23]. Various scoring systems based on history and noninvasive examination assessments developed for the prediction of DO are limited as a screening tool and cannot replace UDS [24]. Comprehensive assessment of history, physical examination, and bedside tests has been shown to be less helpful in diagnosing DO [25]. In the three logistic regression models generated in this study for prediction of DO, Model III (consisting of noninvasive and objective parameters) has the greatest area under the ROC curve and is the best predictor model. Subjective symptoms alone are a poor mirror of the cause of the patient’s condition, and objective findings are not consistent with the patient’s symptoms. By combining both the subjective and objective parameters, our study shows that we can then truly reflect the patient’s condition.
The necessity of having DO diagnosis prior to initiation of treatment is an ongoing debate. There are controversies regarding whether the diagnosis of DO aids in treatment guidance and predicts response to therapy. In a 12-week evaluation of tolterodine ER for the treatment of OAB, patients showed greater improvement in mean voided volume and mean voiding frequency with tolterodine use compared to placebo. However, the effect was not dependent on the presence of DO. There was a lack of clear relationship between DO and response to therapy, and the use of UDS assessment prior to treatment with antimuscarinic therapy has been questioned [26]. On the other hand, Patel et al. found that the presence or absence of DO and the volume at which the patient experiences OAB symptoms are predictive of treatment success and can be helpful in management [27]. In OAB patients, filling cystometry can evaluate compliance, sensation, and detrusor activity [5]. These patients experience earlier sensations, which can be used to characterize symptom severity and as an objective evaluation marker following intervention [28]. It has been recently suggested that there are several subtypes of OAB with different pathophysiologies. Urgency sensation may arise from different etiologies, and DO associated OAB is just one of many [29]. Utilization of UDS can aid in differentiation of etiologies, risk stratification, patient education, and expectant management.
Forty-three to 83% of patients discontinue antimuscarinic therapy for OAB within 1 month period [30]. Perhaps instead of being concerned about the invasiveness of UDS, we should also consider the fact that OAB patients have a high discontinuation rate due to intolerable side effects of OAB medication. In a longitudinal, prospective study, Verghese et. al found that clinicians’ treatment decisions are affected by UDS diagnosis. The authors also found that patients who were treated concordant with their UDS findings were more likely to report an improvement in bladder symptoms [6]. The aid of UDS for targeted treatment with expected better outcomes is of paramount importance. Performing UDS may provide both clinicians and patients a better understanding of their condition, aid in treatment decisions, and provide higher patient satisfaction and compliance rates.
Limitation of study
Our study has a few pitfalls. First, the enrolled population was all of Asian descent, and the results may not apply to the general female population worldwide. Second, as commonly seen in the Asian communities, patients suffering from LUTS often refer to these symptoms of the aging process and may not seek medical attention. Hence, the prevalence and severity of the symptoms cannot reflect the general community. Third, we used a non-physiological medium filling rate for the filling cystometry. The detection rate of DO in a conventional UDS has been known to be inferior and DO is not always demonstrated.
Strength of the study
Our study included a large sample size. All patients were subjected to an uniform and standardized UDS and validated questionnaire survey.
Conclusion
In the present study, we found female patients with DO are associated with older age, increased parity, greater urine leakage, and worse storage and micturition functions on UDS. The combinations of subjective and objective measurements are better predictive models for OAB patients than either one alone. Patient’s self-reported symptoms are often unreliable, and incorporation of UDS findings for treatment planning may increase patient’s compliance with treatment of OAB and satisfaction. Further prospective study utilizing findings of UDS for patient treatment and management is warranted.
References
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, Monga A, Petri E, Rizk DE, Sand PK, Schaer GN, International Urogynecological A, International Continence S. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn. 2010;29(1):4–20. https://doi.org/10.1002/nau.20798.
Rosier P, Schaefer W, Lose G, Goldman HB, Guralnick M, Eustice S, Dickinson T, Hashim H. International Continence Society Good Urodynamic Practices and Terms 2016: Urodynamics, uroflowmetry, cystometry, and pressure-flow study. Neurourol Urodyn. 2017;36(5):1243–60. https://doi.org/10.1002/nau.23124.
Hashim H, Abrams P. Is the Bladder a Reliable Witness for Predicting Detrusor Overactivity? J Urol. 2006;175(1):191–4. https://doi.org/10.1016/s0022-5347(05)00067-4.
Haylen BT, Chetty N, Logan V, Schulz S, Verity L, Law M, Zhou J. Is sensory urgency part of the same spectrum of bladder dysfunction as detrusor overactivity? Int Urogynecol J Pelvic Floor Dysfunct. 2007;18(2):123–8. https://doi.org/10.1007/s00192-006-0165-z.
Brown ET, Krlin RM, Winters JC. Urodynamics: examining the current role of UDS testing. What is the role of urodynamic testing in light of recent AUA urodynamics and overactive bladder guidelines and the VALUE study? Curr Urol Rep. 2013;14(5):403–8. https://doi.org/10.1007/s11934-013-0361-6.
Verghese TS, Middleton LJ, Daniels JP, Deeks JJ, Latthe PM. The impact of urodynamics on treatment and outcomes in women with an overactive bladder: a longitudinal prospective follow-up study. Int Urogynecol J. 2018;29(4):513–9. https://doi.org/10.1007/s00192-017-3414-4.
Robinson D, Staskin D, Laterza RM, Koelbl H. Defining female voiding dysfunction: ICI-RS 2011. Neurourol Urodyn. 2012;31(3):313–6. https://doi.org/10.1002/nau.22213.
Cho KJ, Kim HS, Koh JS, Kim JC. Evaluation of female overactive bladder using urodynamics: relationship with female voiding dysfunction. Int Braz J Urol. 2015;41(4):722–8. https://doi.org/10.1590/s1677-5538.Ibju.2014.0195.
Serati M, Topazio L, Bogani G, Costantini E, Pietropaolo A, Palleschi G, Carbone A, Soligo M, Del Popolo G, Li Marzi V, Salvatore S, Finazzi Agrò E. Urodynamics useless before surgery for female stress urinary incontinence: Are you sure? Results from a multicenter single nation database. Neurourol Urodyn. 2016;35(7):809–12. https://doi.org/10.1002/nau.22804.
Hung MJ, Chou CL, Yen TW, Chuang YC, Meng E, Huang ST, Kuo HC. Development and validation of the Chinese Overactive Bladder Symptom Score for assessing overactive bladder syndrome in a RESORT study. J Formos Med Assoc. 2013;112(5):276–82. https://doi.org/10.1016/j.jfma.2011.09.020.
Avery K, Donovan J, Peters TJ, Shaw C, Gotoh M, Abrams P. ICIQ: a brief and robust measure for evaluating the symptoms and impact of urinary incontinence. Neurourol Urodyn. 2004;23(4):322–30. https://doi.org/10.1002/nau.20041.
Shumaker SA, Wyman JF, Uebersax JS, McClish D, Fantl JA. Health-related quality of life measures for women with urinary incontinence: the Incontinence Impact Questionnaire and the Urogenital Distress Inventory. Continence Program in Women (CPW) Research Group. Qual Life Res. 1994;3(5):291–306. https://doi.org/10.1007/BF00451721.
Barber MD, Walters MD, Bump RC. Short forms of two condition-specific quality-of-life questionnaires for women with pelvic floor disorders (PFDI-20 and PFIQ-7). Am J Obstet Gynecol. 2005;193(1):103–13. https://doi.org/10.1016/j.ajog.2004.12.025.
Su TH, Lau HH. Validation of a Chinese version of the short form of the pelvic organ prolapse/urinary incontinence sexual questionnaire. J Sex Med. 2010;7(12):3940–5. https://doi.org/10.1111/j.1743-6109.2010.01891.x.
Chen SL, Ng SC, Huang YH, Chen GD. Are patients with bladder oversensitivity different from those with urodynamically proven detrusor overactivity in female overactive bladder syndrome? J Chin Med Assoc. 2017;80(10):644–50. https://doi.org/10.1016/j.jcma.2017.03.009.
Baumeister P, Kozomara M, Seifert B, Mehnert U, Kessler TM. Detrusor overactivity is missed by stopping urodynamic investigation at a bladder volume of 500 mL. BJU Int. 2019;124(5):870–5. https://doi.org/10.1111/bju.14868.
Klevmark B. Volume threshold for micturition. Influence of filling rate on sensory and motor bladder function. Scand J Urol Nephrol Suppl. 2002;210:6–10. https://doi.org/10.1080/003655902320765890.
de Boer TA, Salvatore S, Cardozo L, Chapple C, Kelleher C, van Kerrebroeck P, Kirby MG, Koelbl H, Espuna-Pons M, Milsom I, Tubaro A, Wagg A, Vierhout ME. Pelvic organ prolapse and overactive bladder. Neurourol Urodyn. 2010;29(1):30–9. https://doi.org/10.1002/nau.20858.
Burrows LJ, Meyn LA, Walters MD, Weber AM. Pelvic symptoms in women with pelvic organ prolapse. Obstet Gynecol. 2004;104(5 Pt 1):982–8. https://doi.org/10.1097/01.AOG.0000142708.61298.be.
Rovner ES, Goudelocke CM. Urodynamics in the evaluation of overactive bladder. Curr Urol Rep. 2010;11(5):343–7. https://doi.org/10.1007/s11934-010-0130-8.
Guralnick ML, Grimsby G, Liss M, Szabo A, O'Connor RC. Objective differences between overactive bladder patients with and without urodynamically proven detrusor overactivity. Int Urogynecol J. 2010;21(3):325–9. https://doi.org/10.1007/s00192-009-1030-7.
Juszczak K, Ziomber A, Wyczolkowski M, Thor PJ. Urodynamic effects of the bladder C-fiber afferent activity modulation in chronic model of overactive bladder in rats. J Physiol Pharmacol. 2009;60(4):85–91.
Blaivas JG. The Bladder is an Unreliable Witness. Neurol Urodynam. 1996;15:443–5.
Giarenis I, Musonda P, Mastoroudes H, Robinson D, Cardozo L. Can we predict detrusor overactivity in women with lower urinary tract symptoms? The King's Detrusor Overactivity Score (KiDOS). Eur J Obstet Gynecol Reprod Biol. 2016;205:127–32. https://doi.org/10.1016/j.ejogrb.2016.07.495.
Holroyd-Leduc JM, Tannenbaum C, Thorpe KE, Straus SE. What Type of Urinary Incontinence Does This Woman Have? JAMA. 2008;299(12):1446–56.
Malone-Lee JG, Al-Buheissi S. Does urodynamic verification of overactive bladder determine treatment success? Results from a randomized placebo-controlled study. BJU Int. 2009;103(7):931–7. https://doi.org/10.1111/j.1464-410X.2009.08361.x.
Patel B, Choe J, Lee U, Lucioni A, Washington B, Govier F, Kobashi K. Volume at urodynamic detrusor overactivity predicts success with InterStim. J Urol. 2013;189(4S):e929.
Lee SR, Kim HJ, Kim A, Kim JH. Overactive bladder is not only overactive but also hypersensitive. Urology. 2010;75(5):1053–9. https://doi.org/10.1016/j.urology.2009.10.045.
Peyronnet B, Mironska E, Chapple C, Cardozo L, Oelke M, Dmochowski R, Amarenco G, Gamé X, Kirby R, Van Der Aa F, Cornu JN. A Comprehensive Review of Overactive Bladder Pathophysiology: On the Way to Tailored Treatment. Eur Urol. 2019;75(6):988–1000. https://doi.org/10.1016/j.eururo.2019.02.038.
Kim TH, Lee KS. Persistence and compliance with medication management in the treatment of overactive bladder. Investig Clin Urol. 2016;57(2):84–93. https://doi.org/10.4111/icu.2016.57.2.84.
Acknowledgement
The authors would like to thank the Clinical Trial Center in Chang Gung Memorial Hospital, which is supported by the Ministry of Health and Welfare of Taiwan, for statistical assistance (grant MOHW109-TDU-B-212-114005).
Author information
Authors and Affiliations
Contributions
TX Huang: Project development, Data collection, Manuscript writing and editing
TS Lo: Project development, Manuscript editing
HJ Tseng: Data analysis
YH Lin: Manuscript editing
CC Liang: Manuscript editing
WC Hsieh Manuscript editing
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Huang, TX., Lo, TS., Tseng, HJ. et al. Correlation between overactive bladder and detrusor overactivity: a retrospective study. Int Urogynecol J 34, 867–875 (2023). https://doi.org/10.1007/s00192-022-05274-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-022-05274-7