Abstract
Introduction and hypothesis
We examined obstetric and maternal-newborn factors and UI history for stress urinary incontinence (UI) and urge UI during pregnancy and the first year postpartum.
Methods
This prospective cohort study included 1447 pregnant women who underwent prenatal examinations and completed an Incontinence Questionnaire-Urinary Incontinence Short Form before pregnancy, during early, mid- and late pregnancy, and at five visits during the first year postpartum. Data were analyzed using univariate/multivariate generalized estimating equation (GEE) logistic regression analyses.
Results
The prevalence rates of stress UI during late pregnancy (42.5%) and urge UI at 3–5 days postpartum (10.4%) were the highest throughout pregnancy and the first year postpartum. After adjusting for covariates, gestational age increased the risks of stress UI (p < 0.001) and urge UI (p = 0.003); stress UI during pre-pregnancy, number of previous vaginal deliveries and concurrent high body mass index (BMI) increased stress UI (all p < 0.05); urge UI during pre-pregnancy and full-time work increased urge UI (both p < 0.05) during pregnancy. During the postpartum period, vaginal delivery increased stress UI (p < 0.001) and urge UI (p = 0.041); stress UI during pre-pregnancy and pregnancy, women aged ≥ 30 years and vacuum extraction/forceps delivery increased stress UI (all p < 0.05). Urge UI during early, mid- and late pregnancy increased stress UI (all p < 0.05).
Conclusions
Gestational age increased stress and urge UI, while previous vaginal deliveries and high BMI increased stress UI; full-time work increased urge UI during pregnancy. Vaginal delivery increased both UIs, and vacuum/forceps delivery and maternal age increased stress UI during postpartum.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Urinary incontinence (UI) is associated with reduced quality of life during pregnancy [1] and the postpartum period [2]. This involuntary leakage of urine is a common and troublesome symptom with reported rates of 6.8–69.0% during pregnancy and puerperium in Western and Eastern countries [1, 3,4,5]. Of the UI types (stress, urge, mixed and other) [6], stress and urge UIs are the most common during pregnancy [3, 7] and postpartum [4]. Prevalence rates of stress UI and urge UI are 9.1–37.8% and 4.9–14.3% during pregnancy, respectively [3, 7]. During the first year postpartum, prevalence rates of stress UI and urge UI are 18.6–41.0% and 4.9%–12.4%, respectively [3, 4]. Stress UI after childbirth has had a notable impact on the daily activities and emotions of women [8]. Women with urge UI may have higher anxiety [9].
Several studies that have investigated factors related to UI during the pre- and postnatal periods have not specified the UI type [5, 10,11,12,13]. The associated factors for UI in pregnancy include maternal age [11, 14], parity [11], gestational age [11, 12], constipation, previous urinary tract infection [12], body mass index (BMI), pre-pregnancy BMI [14] and occasional leakage before pregnancy [7]. Factors related to UI during the postpartum period include maternal age and parity, mode of delivery [10], antenatal UI and neonatal parameters [5].
The factors associated with certain UI types, such as stress UI or urge UI, may vary; therefore, they require clarification so that effective treatment strategies for UI can be determined. A recent study reported that parity was associated with stress UI during pregnancy [15]. Factors associated with the postpartum prevalence of stress UI include vaginal delivery [3, 4, 15] and antenatal stress UI [3]. Factors associated with urge UI postpartum include vaginal delivery [4], antenatal urge UI and increasing maternal BMI during the first trimester [3]. In contrast, studies found that vaginal delivery was not associated with urge UI postpartum [3, 15]. Factors associated with stress and urge urinary incontinence (UI) during the prenatal and postnatal periods remain uncertain.
To date, few studies have specifically examined the factors associated with the prevalence of stress UI and urge UI during pregnancy and postpartum. Additionally, pre-pregnancy and prenatal UI data have seldom been incorporated in long-term follow-up investigations. Therefore, we examined data on obstetric maternal-newborn factors and UI history that were related to the prevalence of stress UI and urge UI during pregnancy and the first year postpartum.
Methods
Study sample and procedure
We conducted a prospective cohort study of women’s health during pregnancy and the postpartum period. The study was approved by the Research Ethics Committee of the medical center. In this study, convenience sampling was used to recruit pregnant women from among those receiving prenatal examinations at a medical center in Taiwan. The inclusion criteria were women at ≤ 16 weeks of gestation at the time of recruitment who could read the questionnaires, planned to receive prenatal examinations and give birth at the study hospital and were willing to complete the questionnaire from pregnancy to postpartum. The exclusion criteria were a risk of miscarriage or fetal abnormality at the time of recruitment. The women read and signed a consent form before participating in the study; participants were informed that they were free to withdraw at any time. Data from 2009 to 2018 were used in this study. Women were recruited during early pregnancy and completed questionnaires regarding personal data (e.g., age and employment) and UI during the month before becoming pregnant (pre-pregnancy) and during the current month. The participants were followed up during the mid and late stages of pregnancy, 3–5 days, 1, 3, 6 and 12 months after childbirth in the waiting room before prenatal examinations and at 3–5 days and 1, 3, 6 and 12 months after childbirth in the maternity units or by mail. Data on birth and newborn parameters were obtained from the medical records.
UIs were assessed using the Taiwanese version of International Consultation on Incontinence Questionnaire-Urinary Incontinence Short Form (ICIQ-UI SF) [16, 17], which is regarded as reliable and valid for evaluating UI among Taiwanese women [17]. Cronbach’s alpha coefficient estimates for the Taiwanese version of ICIQ-UI SF at all time points included in this study ranged from 0.78 to 0.85.
ICIQ-UI SF comprises three scored questions and one non-scored question and is easy to complete [16]. The three scored questions of the ICIQ-UI SF include: “How often do you leak urine? How much urine do you usually leak?Overall, how much does leaking urine interfere with your everyday life?” The total scores for the three questions were recorded, with a minimum score of 0 and a maximum score of 21. Cut-off scores are set as 0 (no incontinence) and ≥ 1 (UI).
The International Urogynecological Association (IUGA) and the International Continence Society (ICS) defined that stress UI is the complaint of urine leakage associated with coughing, sneezing or physical exertion, whereas urge UI is the complaint of urine leakage associated with a sudden compelling desire to void that is difficult to delay [18, 19].
UI type was determined based on one non-scored question of the ICIQ-UI SF (“When does urine leak?”). The optional responses indicating stress UI included, “leaks when you cough or sneeze” and “leaks when you are physically active/exercising.” The three remaining responses, “leaks before you can get to the toilet,” “leaks when you are asleep” and “leaks when you have finished urinating and are dressed,” indicated urge UI. A combination of these responses indicating urge UI and stress UI was classified as mixed UI, and the responses “leaks for no obvious reason” and “leaks all the time” were regarded as other UI type [6].
Statistical analyses
Descriptive statistics were used to report the participants’ characteristics and UI types. These characteristics (obstetric and maternal–newborn parameters) included time-dependent and fixed variables. The time-dependent variables included age, concurrent BMI, changes in BMI from pre-pregnancy to each time point, employment type, gestational age and current medical condition/history. The fixed variables were parity, number of previous deliveries, delivery method, instrument use, body weight and head circumference of the newborn. Obstetric and maternal-newborn parameters and UI history were independent variables. Outcome variables were UI rates including prevalence of stress UI and urge UI during early, mid- and late pregnancy and at 3–5 days and 1, 3, 6 and 12 months postpartum. Associations between independent variables and the prevalence of stress UI and urge UI during pregnancy (early to late pregnancy) and the postpartum period (3–5 days to 12 months postpartum) were analyzed using univariate/multivariate generalized estimating equation (GEE) binary logistic analysis; the odds ratio (OR) and its 95% confidence interval (CI) were also reported. Correlation coefficient analyses were used to examine multicollinearity among the independent variables. The subjects with incomplete data on the UI questionnaire were excluded. Multivariate regression analysis included variables with p < 0.10 from univariate regression analysis. The two-tailed significance threshold was set at p < 0.05; statistical analyses were performed using SPSS version 20 (IBM Corp., Somers, NY).
Results
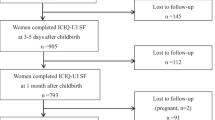
In total, 1447, 1366, 1241, 1169, 1045, 992, 885, 797 and 735 women completed valid questionnaires during early pregnancy, pre-pregnancy, mid- and late pregnancy and at 3–5 days, 1, 3, 6 and 12 months postpartum, respectively (Supplementary Fig. 1). The reasons for failure to attend follow-up evaluations at each stage included personal privacy, frequent visits (early pregnancy), abortion (early and mid-pregnancy), preterm delivery (late pregnancy), feeling uncomfortable, prenatal examination or delivery at other clinics (early, mid- and late pregnancy), being tired after childbirth (3–5 days after birth), anxious with sick baby, busy with baby care (3–5 days, 1 month and 3 months postpartum), being pregnant again, loss of contact (6 and 12 months postpartum) and unknown. There were no significant differences in age and parity during early pregnancy (p = 0.884, p = 0.276, respectively) and at 3–5 days postpartum (p = 0.187, p = 0.495, respectively) between the participants and non-participants.
The characteristics of the participants during pregnancy and postpartum are shown in Table 1 and Supplementary Table 1. The prevalence rates of stress UI and urge UI at the nine time points are shown in Fig. 1. The rate of stress UI during late pregnancy (42.5%) was the highest, and the rate of urge UI at 3–5 days postpartum (10.4%) was the highest across pregnancy and the first year postpartum. The prevalence rates of mixed UI and other UI at each time point are shown in Supplementary Fig. 2. The UI prevalence rates at the nine time points were 22.0%, 32.3%, 53.9%, 60.4%, 33.4%, 31.9%, 32.7%, 31.0% and 35.6%, respectively. Significant variables from univariate analysis for stress UI and urge UI prevalence during pregnancy and the first year postpartum were treated as covariates in multivariate regression analysis.
Stress UI and urge UI during pregnancy
After adjusting for covariates, multivariate GEE logistic regression analysis indicated that risk factors for stress UI during pregnancy were concurrent high BMI (OR: 1.03, 95% CI: 1.00–1.06), gestational age (OR: 1.04, 95% CI: 1.03–1.05), number of previous vaginal deliveries (OR: 2.03, 95% CI: 1.51–2.73) and stress UI during pre-pregnancy (OR: 12.42, 95% CI: 9.10–16.96) (Table 2).
Risk factors for urge UI during pregnancy were full-time work (OR: 1.55, 95% CI: 1.02–2.36), gestational age (OR: 1.03, 95% CI: 1.01–1.04) and urge UI during pre-pregnancy (OR: 28.29, 95% CI: 17.54–45.63) after adjusting for covariates (Table 3).
Stress UI and urge UI during the first year postpartum
After adjusting for covariates, risk factors for stress UI during the postpartum period were maternal ages of 30–34 years (OR: 2.06, 95% CI: 1.21–3.50) and ≥ 35 years (OR: 2.46, 95% CI: 1.44–4.20), vaginal delivery (OR: 2.31, 95% CI: 1.69–3.15), vacuum extraction or forceps delivery (OR: 1.76, 95% CI: 1.22–2.52), stress UI during pre-pregnancy (OR: 2.19, 95% CI: 1.56–3.07) and stress UI during early, mid- and late pregnancy (OR: 1.98, 95% CI: 1.45–2.72; OR: 1.96, 95% CI: 1.37–2.81; OR: 2.10, 95% CI: 1.50–2.94, respectively) (Table 4).
Risk factors for urge UI during the postpartum period were vaginal delivery (OR: 1.68, 95% CI: 1.02–2.76) and urge UI during early, mid- and late pregnancy (OR: 3.74, 95% CI: 1.34–10.45; OR: 3.85, 95% CI: 1.71–8.66; OR: 2.32, 95% CI: 1.02–5.28, respectively) after adjusting for covariates (Table 5).
Discussion
This longitudinal follow-up study presents a clear profile of stress UI and urge UI during pre-pregnancy, three stages of pregnancy and the first year postpartum. Our findings verified obstetric and maternal-newborn factors associated with the prevalence rate of stress UI and urge UI during the pre- and postnatal periods. In addition, the effects of experiencing a history of UI on stress UI and urge UI during pregnancy and postpartum were identified.
This study found that the number of previous vaginal deliveries increased the prevalence of stress UI in the following pregnancies, but it did not increase the prevalence of urge UI. One cross-sectional study reporting that previous instrumental vaginal delivery was associated with UI during pregnancy did not specify the UI type [20]. In addition, parity was associated with stress UI [15] or any UI [11] during pregnancy. In our study, univariate but not multivariate regression models showed that higher parity was associated with stress UI during pregnancy. This finding may be due to the fact that the number of previous vaginal deliveries had a stronger influence on stress UI than parity. Additionally, parity was not associated with stress and urge UI during the first year postpartum, which was concordant with the results of a prior study of women followed up at 6 weeks postpartum [15].
Previous studies have reported that childbirth is a notable pathophysiological factor that contributes to the development of UI in women [21]; furthermore, vaginal delivery can cause pelvic floor trauma and pudendal nerve injury [22]. These injuries may result in the development of UI [23]. In this study, vaginal delivery increased the prevalence of stress UI during the postpartum period. This finding is concordant with those of previous studies, reporting that vaginal delivery was associated with a higher postpartum prevalence of stress UI [3, 4] as well as an increased risk of long-term stress UI [24]. In contrast, vaginal delivery was not associated with stress UI at 6 months postpartum [25].
Our findings verified that vaginal delivery was associated with urge UI after childbirth. Consistently, previous studies found an association of vaginal delivery with a higher prevalence of urge UI during the postpartum period [4] and with a slightly increased risk of urge UI compared to cesarean delivery [24]. However, other studies reported no association between vaginal delivery and the prevalence of urge UI at 6 weeks [15] and 12 months postpartum [3].
Furthermore, we found that delivery by vacuum extraction or forceps increased the risk of stress UI during the first year postpartum. A previous study reported that forceps delivery increased the long-term risk of stress UI compared with other vaginal deliveries for women aged < 50 years [26]. However, there was no long-term risk of stress due to the mode of delivery in women aged ≥ 50 years [26].
Our study showed that the prevalence rate of stress UI during pregnancy ranged from 23.8% to 42.5%, which was higher than those of urge UI (4.1%–6.9%), mixed UI (1.2%–6.3%) and other UI (1.3%–4.6%). Similarly, the prevalence rate of stress UI during the first year postpartum was 16.3%–23.8%, which was higher than those of urge UI (6.7%–10.4%), mixed UI (1.8%–4.1%) and other UI (1.9%–4.1%). These findings indicate that the prevalence of stress UI is the most common among the UI types during pregnancy and postpartum, which is in agreement with the reports by previous studies [3, 4, 7].
The prevalence rates of both stress UI and urge UI increased throughout the three stages of pregnancy. The highest rates were recorded during late pregnancy, which was supported by the findings of a regression analysis showing that gestational age increased the risk of stress UI and urge UI during pregnancy. This finding is consistent with the results of previous cross-sectional studies that reported that the third trimester had a higher risk for any UI than the first trimester and that gestational age increased the risk of any UI [11, 12]. In addition, the prevalence of stress UI declined during the period from late pregnancy to 3–5 days postpartum. This finding may be related to the decrease in maternal BMI after childbirth, which was supported by the regression analysis result showing that BMI increased the risk of stress UI during pregnancy, but not during the postpartum period.
Moreover, concurrent high BMI correlated with the increased prevalence of stress UI during pregnancy, and not urge UI. BMI was previously reported to be a risk factor for the prevalence of UI during pregnancy [14]. However, during the first postpartum year, concurrent high BMI was not a risk factor for the prevalence of stress and urge UI. In contrast to our findings, previous studies that did not specify the UI type reported that a high BMI increased the rates of UI at 3 months [27] and 6 months postpartum [28]. The inconsistency in the findings between our study and the previous studies may reflect the differences in the BMI of the included women, UI type or study design.
The increases in BMI of women from pre-pregnancy to each time point during pregnancy or the postpartum period were not associated with stress and urge UI in this study. One study that did not indicate the UI type showed that weight gain during pregnancy was not associated with an increased prevalence of UI during pregnancy or the postpartum period [29]. However, another study reported that an increase in maternal BMI during the first trimester was associated with urge UI at 12 months after delivery [3].
Stress UI experienced prior to pregnancy was associated with an increased prevalence of stress UI during pregnancy and the postpartum period. Urge UI prior to pregnancy was also associated with an increased prevalence of urge UI during pregnancy, which is consistent with the findings of a prior study reporting that women with pre-pregnancy UI had an increased probability of developing UI during pregnancy [14]. The presence of stress and urge UI during early, mid- and late pregnancy increased the prevalence of stress and urge UI during the postpartum period, respectively. Previous studies reported that antenatal UI was associated with postpartum UI [3], and the occurrence of stress UI at term was only associated with stress UI at 6 months postpartum [25]. However, no association was reported between women reporting UI at late pregnancy and stress UI or urge UI at 6 weeks postpartum [15].
Our study showed an increased prevalence of stress UI in women aged ≥ 30 years during the postpartum period. An earlier cross-sectional study reported that women > 25 years following the first delivery were at an increased risk of UI [30]. However, in the current study, newborn parameters (e.g., birthweight and head circumference) were not risk factors for any of the examined postpartum UI types, contrary to the findings of previous studies [5]. This discrepancy may be due to the differences in the body sizes of the included newborns or the study design. In contrast, full-time work increased the prevalence of urge UI during pregnancy in the present study. However, no data have been reported regarding the association between UI and employment during the prenatal or postnatal periods. This finding requires further investigation in future studies involving larger study populations.
Our finding suggests that health providers should prioritize UI type detection during clinical assessment and devote more time to women with risk factors. In addition, health providers should provide information regarding lifestyle modifications (e.g., smoking cessation) to manage both stress and urge UI, exercise (e.g., pelvic floor muscle exercises) and weight reduction for overweight women to manage stress UI and avoidance of excessive fluids and regular urinating intervals to manage urge UI [31]. Our study verified that both UI types during pregnancy have a strong impact on the UI types postpartum. This suggests that the provision of information regarding UI prevention or intervention, such as pelvic floor muscle exercises, to pregnant women is important, and women should be encouraged to perform these exercises.
Women who are pregnant or intend to become pregnant frequently research the advantages and disadvantages of vaginal and cesarean deliveries [32]. Our findings will improve the understanding of health providers regarding the associations between the mode of delivery and the various types of UI. In addition, we encourage healthcare professionals to remain alert when assessing postpartum UI, particularly in women who have undergone vaginal delivery or vacuum extraction/forceps delivery.
The main strengths of the study included its prospective cohort design with multiple time points and performance of repeated-measures statistical analyses, which both increased the accuracy of data and statistical power and eliminated all issues concerning individual differences. The limitations of this study relate to the self-reporting of UI by participants. However, both stress and urge UI types were evaluated using validated instruments that have been confirmed by urodynamic measures [6]. The generalizability of our study findings may be limited as all participants were selected from a single medical center. Other potential factors, such as episiotomy and perineal laceration, were not presented because of the high degree of multicollinearity. Retrospective recall of pre-pregnancy UI by women may be influenced by a memory bias during data collection. The dropout rate may also represent a limitation, as this study was based on multiple measures over a long-term follow-up period.
Conclusions
Distributions of self-reported stress UI and urge UI across pregnancy and the first year postpartum were precisely demonstrated in this long-term follow-up study. Factors associated with stress and urge UI during pre- and postnatal periods were equivalent or varied. During pregnancy, the gestational age was associated with increased prevalence of both stress and urge UI, while the number of previous vaginal deliveries, stress UI during pre-pregnancy and high concurrent BMI scores were associated with increases in stress UI, full-time work increased urge UI. During the first year postpartum, vaginal delivery increased both stress and urge UI. Moreover, stress UI during pre-pregnancy, early, mid- and pregnancy, an age of 30 years or older and vacuum extraction/forceps delivery were associated with stress UI, but not urge UI. These findings provide valuable insight regarding factors associated with UI type during pregnancy and after childbirth. In addition, UI awareness should be promoted to assess the UI type early, particularly for women with risk factors, and initiate effective strategies for stress UI and urge UI during the pre-pregnancy, prenatal and postnatal periods.
References
Rogers RG, Ninivaggio C, Gallagher K, Borders AN, Qualls C, Leeman LM. Pelvic floor symptoms and quality of life changes during first pregnancy: a prospective cohort study. Int Urogynecol J. 2017;28(11):1701–7.
Trivino-Juarez JM, Romero-Ayuso D, Nieto-Pereda B, Forjaz MJ, Criado-Alvarez JJ, Arruti-Sevilla B, Aviles-Gamez B, Oliver-Barrecheguren C, Mellizo-Diaz S, Soto-Lucia C, Pla-Mestre R. Health related quality of life of women at the sixth week and sixth month postpartum by mode of birth. Women Birth. 2017;30(1):29–39.
Chan SS, Cheung RY, Yiu KW, Lee LL, Chung TK. Prevalence of urinary and fecal incontinence in Chinese women during and after their first pregnancy. Int Urogynecol J. 2013;24(9):1473–9.
Chang SR, Chen KH, Lin HH, Lin MI, Chang TC, Lin WA. Association of mode of delivery with urinary incontinence and changes in urinary incontinence over the first year postpartum. Obstet Gynecol. 2014;123(3):568–77.
Wesnes SL, Hannestad Y, Rortveit G. Delivery parameters, neonatal parameters and incidence of urinary incontinence six months postpartum: a cohort study. Acta Obstet Gynecol Scand. 2017;96(10):1214–22.
Rotar M, Trsinar B, Kisner K, Barbic M, Sedlar A, Gruden J, Vodusek DB. Correlations between the ICIQ-UI short form and urodynamic diagnosis. Neurourol Urodyn. 2009;28(6):501–5.
Brown SJ, Donath S, MacArthur C, McDonald EA, Krastev AH. Urinary incontinence in nulliparous women before and during pregnancy: prevalence, incidence, and associated risk factors. Int Urogynecol J. 2010;21(2):193–202.
Mason L, Glenn S, Walton I, Appleton C. The experience of stress incontinence after childbirth. Birth. 1999;26(3):164–71.
Perry S, McGrother CW, Turner K. An investigation of the relationship between anxiety and depression and urge incontinence in women: development of a psychological model. Br J Health Psychol. 2006;11(Pt 3):463–82.
Ng K, Cheung RYK, Lee LL, Chung TKH, Chan SSC. An observational follow-up study on pelvic floor disorders to 3-5 years after delivery. Int Urogynecol J. 2017;28(9):1393–9.
Kok G, Seven M, Guvenc G, Akyuz A. Urinary incontinence in pregnant women: prevalence, associated factors, and its effects on health-related quality of life. J Wound Ostomy Continence Nurs. 2016;43(5):511–6.
Dinç A. Prevalence of urinary incontinence during pregnancy and associated risk factors. Lower Urinary Tract Symptoms. 2018;10(3):303–7.
Siahkal SF, Iravani M, Mohaghegh Z, Sharifipour F, Zahedian M. Maternal, obstetrical and neonatal risk factors' impact on female urinary incontinence: a systematic review. Int Urogynecol J. 2020;31(11):2205–24.
Daly D, Clarke M, Begley C. Urinary incontinence in nulliparous women before and during pregnancy: prevalence, incidence, type, and risk factors. Int Urogynecol J. 2018;29(3):353–62.
Slavin V, Creedy DK, Gamble J. Benchmarking outcomes in maternity care: Peripartum incontinence - a framework for standardised reporting. Midwifery. 2020;83:102628.
Avery K, Donovan J, Peters TJ, Shaw C, Gotoh M, Abrams P. ICIQ: a brief and robust measure for evaluating the symptoms and impact of urinary incontinence. Neurourol Urodyn. 2004;23(4):322–30.
Chang SR, Chen KH, Chang TC, Lin HH. A Taiwanese version of the international consultation on incontinence questionnaire—urinary incontinence short form for pregnant women: instrument validation. J Clin Nurs. 2011;20(5-6):714–22.
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, Monga A, Petri E, Rizk DE, Sand PK, Schaer GN. An international urogynecological association (IUGA)/international continence society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn. 2010;29(1):4–20.
Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, van Kerrebroeck P, Victor A, Wein A. The standardisation of terminology of lower urinary tract function: report from the standardisation sub-committee of the International Continence Society. Neurourol Urodyn. 2002;21(2):167–78.
Okunola TO, Olubiyi OA, Omoya S, Rosiji B, Ajenifuja KO. Prevalence and risk factors for urinary incontinence in pregnancy in Ikere-Ekiti. Nigeria Neurourol Urodyn. 2018;37(8):2710–6.
Beck RP, McCormick S, Nordstrom L. Intraurethral-intravesical cough-pressure spike differences in 267 patients surgically cured of genuine stress incontinence of urine. Obstet Gynecol. 1988;72(3 Pt 1):302–6.
Chapple CR, Manassero F. Pathophysiology of stress incontinence. In: Raz S, Rodríguez LV, editors. Female urology. Elsevier Saunders; 2008. p. 301–9.
Groutz A. Pregnancy, childbirth, and pelvic floor injury. In: Raz S, Rodríguez LV, editors. Female urology. Elsevier Saunders; 2008. p. 533–41.
Tahtinen RM, Cartwright R, Tsui JF, Aaltonen RL, Aoki Y, Cardenas JL, El Dib R, Joronen KM, Al Juaid S, Kalantan S, Kochana M, Kopec M, Lopes LC, Mirza E, Oksjoki SM, Pesonen JS, Valpas A, Wang L, Zhang Y, Heels-Ansdell D, Guyatt GH, Tikkinen KAO. Long-term impact of mode of delivery on stress urinary incontinence and urgency urinary incontinence: a systematic review and meta-analysis. Eur Urol. 2016;70(1):148–58.
Arrue M, Ibanez L, Paredes J, Murgiondo A, Belar M, Sarasqueta C, Diez-Itza I. Stress urinary incontinence six months after first vaginal delivery. Eur J Obstet Gynecol Reprod Biol. 2010;150(2):210–4.
Tahtinen RM, Cartwright R, Vernooij RWM, Rortveit G, Hunskaar S, Guyatt GH, Tikkinen KAO. Long-term risks of stress and urgency urinary incontinence after different vaginal delivery modes. Am J Obstet Gynecol. 2019;220(2):181.e181–8.
Glazener CM, Herbison GP, MacArthur C, Lancashire R, McGee MA, Grant AM, Wilson PD. New postnatal urinary incontinence: obstetric and other risk factors in primiparae. BJOG. 2006;113(2):208–17.
Ruiz de Vinaspre Hernandez R, Rubio Aranda E, Tomas Aznar C. Urinary incontinence and weight changes during pregnancy and post partum: a pending challenge. Midwifery. 2013;29(12):e123–9.
Wesnes SL, Hunskaar S, Bo K, Rortveit G. Urinary incontinence and weight change during pregnancy and postpartum: a cohort study. Am J Epidemiol. 2010;172(9):1034–44.
Rortveit G, Hunskaar S. Urinary incontinence and age at the first and last delivery: the Norwegian HUNT/EPINCONT study. Am J Obstet Gynecol. 2006;195(2):433–8.
Lukacz ES, Santiago-Lastra Y, Albo ME, Brubaker L. Urinary incontinence in women: a review. JAMA. 2017;318(16):1592–604.
Faisal I, Matinnia N, Hejar AR, Khodakarami Z. Why do primigravidae request caesarean section in a normal pregnancy? A qualitative study in Iran. Midwifery. 2014;30(2):227–33.
Acknowledgements
This study was supported by a grant from the Ministry of Science and Technology of Taiwan. The authors thank MS. Yi-Wen Wang for data collection.
Author information
Authors and Affiliations
Contributions
SR Chang: Project development, data collection and management, manuscript writing.
WA Lin: Data management and analysis.
TC Chang: Data collection and manuscript preparation.
HH Lin: Data collection and manuscript preparation.
CN Lee: Data collection and manuscript preparation.
MI Lin: Manuscript preparation.
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 258 kb)
Rights and permissions
About this article
Cite this article
Chang, SR., Lin, WA., Chang, TC. et al. Risk factors for stress and urge urinary incontinence during pregnancy and the first year postpartum: a prospective longitudinal study. Int Urogynecol J 32, 2455–2464 (2021). https://doi.org/10.1007/s00192-021-04788-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-021-04788-w