Abstract
Objective
To determine the distribution of urinary incontinence (UI) symptoms and their relation to childbirth events.
Methods
This cross-sectional study used a structured self-administered questionnaire that included the Questionnaire for Female Urinary Incontinence Diagnosis and the Urogenital Distress Inventory Short Form. The study included 802 women sampled from four primary health care centers in Dammam, KSA. A chi-square test and adjusted logistic regression models were used to examine the relation between UI symptoms and obstetric events.
Results
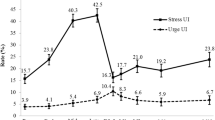
Of the participants, 56.6% (n = 454) had at least one UI symptom. Symptoms were most commonly associated with grand multiparity (80.47%), a history of abortion (72%), assisted vaginal delivery (70%), an age of ≤ 18 years at first birth (66.67%) and ≥ 35 years at last birth (75.48%), and a history of macrosomia (84.62%) and episiotomy (67.89%). Unlike the risk of urgency UI, the risk of stress UI was statistically significantly linked to obstetric events. Grand multiparity was associated with a higher risk of both stress UI (odds ratio [OR]: 3.75, confidence interval [95% CI]: 1.68–8.40) and urgency UI (OR: 2.87, 95% CI: 1.07–7.73).
Conclusion
UI symptoms are common among grand multiparas. Unlike urgency UI, stress UI is associated with previous obstetric events.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
During routine clinical visits, physicians infrequently screen for urinary incontinence (UI) [1], which is defined as “the complaint of any involuntary loss of urine” [2]. Although it is not considered a life-threatening condition, a small amount of urinary leakage might affect women’s quality of life and restrict their daily activities [3].
According to its mechanism, there are two main types of UI: urgency and stress UI [2]. Urgency UI is “the complaint of involuntary leakage accompanied by or immediately preceded by urgency” [2]. It is believed to be related to detrusor muscle overstimulation due to pathology, or irritation of the muscle, or neurological or psychological overstimulation, and it is not thought to be due to abnormality in the urethral sphincter [4]. On the other hand, stress UI is “the complaint of involuntary leakage on effort or exertion, or on sneezing or coughing” [2], and it might develop as a result of pelvic floor weakness, possibly caused by childbirth [2, 5]. Reported obstetric events that might cause UI are grand multiparity, assisted vaginal delivery, episiotomy, and macrosomia [6, 7]. UI has been defined in the literature on an additive scale of multiple symptoms when examined in relation to obstetric events. However, understanding the relationship between obstetric events and various individual UI symptoms might help to understand the mechanism of UI development in relation to childbirth.
The symptoms of UI vary according to the type. Those of urgency UI are mainly related to urinary leakage after a strong feeling of urgency to urinate that leads to rushing to the bathroom, whereas those of stress UI are mainly related to urinary leakage due to pelvic floor overload caused by actions such as coughing, heavy lifting, and jogging [2]. If the symptoms of urgency and stress UI overlap, it is called mixed UI [2, 8].
Globally, the rate of UI among women is reported to be from 25% to 45% [9]. In the Kingdom of Saudi Arabia (KSA), few studies have investigated UI in females despite its reported high incidence, ranging between 28% and 41% [6, 7, 10, 11]. In the KSA, women with UI have very limited access to advanced technologies in urogynecological medical care due to its scarcity, regardless of the high fertility rate among Saudi women. Thus, the aim of this study was to determine the distribution as well as the risk of developing UI symptoms in relation to obstetric events and health-related risk factors among women in Dammam, KSA.
Materials and methods
The study used a cross-sectional design that involved four primary health care centers (PHCs) in the city of Dammam. These PHCs are the largest in Dammam and were systematically chosen to represent the four proposed strata of the city Dammam, which is divided into two administrative areas, east and west, and further stratified for the purposes of this study into northeast, southeast, southwest, and northwest. The samples were collected equally from each center. The range of the average number of PHC visitors per day per center was 150 to 300 visitors. The participants’ data were collected over 1 month’s time on various working days and during various hours to ensure that this study captured a variety of attendees’ sociodemographic characteristics. The participants were selected arbitrarily from the waiting room before seeing their general practitioner, regardless of their original complaints, once it was determined that they met our study criteria. The data were collected by five researchers (RL Alghamdi, FA Almulhim, HM Alsadah, JM Almutawaa, and KA Alnakhli) who unified their data collection approach for consistency and performed a pilot study prior to this study. The study was approved by the ethics committee of Imam Abdulrahman bin Faisal University (IRB-UGS-2018-01-307), and all participants gave written informed consent before the study began.
The sample included Saudi women who visited one of the selected PHCs between July and August 2019. The following were excluded from the sample: women younger than 18 years of age, pregnant women, women who had given birth or had pelvic surgery in the previous 6 weeks, and women with urinary tract infections. Data were collected using face-to-face interviews to complete a structured questionnaire consisting of four parts: part 1 concerned the participants’ sociodemographic characteristics and health indicators; part 2 was related to the patients’ obstetric histories; part 3 was the Questionnaire for Female Urinary Incontinence Diagnosis (QUID) [8]; part 4 was the Urogenital Distress Inventory Short Form (UDI-6) [12].
The sociodemographic and health data included age (< 20 years, 20–29 years, 30–39 years, 40–49 years, or ≥ 50 years), marital status (never married, currently married, separated, or widowed), education level (elementary, intermediate, high school, or university or higher), income (continuous variable), smoking (yes/no), body mass index (BMI) (underweight [< 18.5 kg/m2], normal [18.5–24.9 kg/m2], overweight [25–29.9 kg/m2], or obese [> 30 kg/m2]), and presence of chronic disease (yes/no), including diabetes (both type I and type II), hypertension, sickle cell disease, heart disease, asthma, and dyslipidemia. The included obstetric events were parity (nulliparity, 1–4 births, or grand multiparity), abortion either induced or spontaneous (yes/no), mode of last delivery (not applicable [nulliparous], vaginal, or cesarean), age at last childbirth (not applicable [nulliparous], < 35 years, or ≥ 35 years), pregnancy complications including gestational diabetes, pregnancy-induced hypertension (yes/no), history of macrosomia (not applicable [nulliparous], yes/no), and history of episiotomy (not applicable [nulliparous], yes/no).
The UI symptoms were determined using the UDI-6, a short questionnaire that includes six items, each of which is aimed at evaluating the magnitude (not at all, slightly, moderately, or greatly) of the following symptoms: frequent urination, leakage related to a feeling of urgency, leakage related to physical activity, coughing, or sneezing, small amounts of urine leakage (drops), difficulty emptying the bladder, and pain or discomfort in the lower abdominal or genital area. During the analysis, each item was recorded as present (i.e., slightly, moderately or greatly) or absent (i.e., not at all).
The type of UI was determined using the QUID, which divides the UI types into stress incontinence, urgency incontinence, and mixed incontinence by assessing the urine leakage frequency (none of the time, rarely, once in a while, often, most of the time, or all of the time) during six daily life situations: (1) coughing or sneezing, (2) bending down or lifting something, (3) walking quickly, jogging, or exercising, (4) undressing in order to use the toilet, (5) feeling a strong and uncomfortable need to urinate before reaching the toilet, and (6) rushing to the bathroom because of a sudden, strong need to urinate. Stress incontinence was identified as present if the total score of items 1, 2, and 3 was ≥ 4. Urgency incontinence was identified as present if the total score of items 4, 5, and 6 was ≥ 6. Mixed incontinence was identified as present if both stress and urgency incontinence were present.
A chi-square test was used to compare the rate of obstetric events between women with and without UI symptoms. Unadjusted and adjusted logistic regression models (which were adjusted for age, marital status, education level, income, smoking, BMI, and chronic disease) were used to assess the risk of developing stress or urgency incontinence as well as various UI symptoms. The analyses were performed using Stata version 16 (StataCorp, College Station, TX, USA). A P value of 0.05 was considered statistically significant for all the analytic tests.
Results
The total number of included participants was n = 802 and the study response rate was 88.13%. Around 67% (n = 516) of the participants were in their 20s and 30s. In addition, around 70% (n = 564) were married. Regarding their education, 62.2% (n = 499) had a high school degree or lower, while 37.80% (n = 303) had a university degree or higher.
The rate of UI symptoms was 56.61% (n = 454); however, only 12.56% (n = 57) of women with UI symptoms sought medical advice, which did not completely resolve their symptoms. In total, 5.95% (n = 27) received prescribed medication; 5.51% (n = 25), attempted Kegel exercises; 0.88% (n = 4) had corrective surgeries. The symptoms of UI were significantly common among women who were > 50 years of age 75.36% (n = 52), obese 69.31% (n = 131), and having chronic diseases: 62.62% (n = 201), especially diabetes 79.17% (n = 57). Regarding diabetic women, 54.62% (n = 438) were overweight or obese, and 55.56% (n = 40) were grand multiparas, while 8.33% (n = 6) were nulliparas, and 44.44% (n = 32) were > 50 years of age. Table 1 further summarizes the health risk factors in relation to UI types.
The mean UDI-6 score of nulliparas was 6.73 ± 11.56, while the mean score of multiparas was 13.89 ± 0.65 (t: −6.36, df: 800, P < 0.001). Among multiparas, the mean UDI-6 score of those who had experienced obstetric events was 14.98 ± 14.36, whereas that of women who had not experienced obstetric events was 8.77 ± 15.51 (P < 0.001).
As shown in Table 2, obstetric events varied significantly between women with at least one symptom of urinary incontinence and women with no symptoms. Urinary incontinence symptoms were more common among women with grand multiparity (80.47%), a history of abortions (72%), assisted vaginal delivery (70%), an age of ≤ 18 years at first birth (66.67%) and ≥ 35 years at last birth (75.48%), and a history of macrosomia (84.62%) or episiotomy (67.89%).
As seen in Table 3, frequent leakage was the most common UI symptom among the study participants. In multiparous women with obstetric events, frequency was followed by leakage associated with physical activity (46.39%), whereas in nulliparous and multiparous women with no obstetric complications, it was followed by pelvic or genital pain (21.33% and 29.25%, respectively).
Compared to nulliparas, the risk of developing stress incontinence was greater in multiparas (odds ratio [OR]: 2.04; 95% confidence interval [CI]: 1.02, 4.06) and in grand multiparas (OR: 3.75; 95% CI: 1.68, 8.40). Furthermore, the risk of stress incontinence increased if women were < 18 years of age at first birth (OR: 2.27; 95% CI: 1.16, 4.49) and if women were > 35 years of age at last birth (OR: 3.19; 95% CI: 6.85, 1.49) compared to women who had never given birth In addition, compared to nulliparas, the risk of stress UI increased in multiparas with or without a history of episiotomy (OR: 2.13, 95% CI: 1.04–4.38 and OR: 2.39, 95% CI: 1.19–4.82, respectively). Similarly, in reference to nulliparas, the risk of stress UI increased in multiparas with or without a history of macrosomia (OR: 2.78, 95% CI: 1.13–4.40 and OR: 2.23, 95% CI: 1.07–6.96, respectively). On the other hand, urgency and mixed UI were not statistically significantly related to the obstetric profile after adjustment for the sociodemographic characteristics. For further information, see Table 4 in the supplementary material.
Regarding the various UI symptoms, which were measured using UDI-6, grand multiparity (compared to nulliparity) significantly increased the risk of having urgency-related leakage (OR: 5.12; 95% CI = 2.64–9.89), the risk of leakage due to physical activity (OR: 4.92; 95% CI = 2.25–8.19), and the risk of urgency (OR: 3.97; 95% CI: 2.07, 7.61). Additionally, in reference to nulliparity, having a history of macrosomia significantly increased the risk of having frequency (OR: 3.00; 95% CI: 1.46, 6.19), the risk of leakage with physical activity (OR: 3.10; 95% CI: 1.48, 6.47), the risk of leakage due to urgency (OR: 3.77; 95% CI: 1.80, 7.86), and the risk of discomfort in the pelvic or genital areas (OR: 2.59; 95% CI: 1.26, 5.32). For further information, see Table 5 in the supplementary material.
Regarding the risk of developing the various types of UI in relation to sociodemographic features, only the following relationships were found to be statistically significant. First, the risks of developing stress UI (OR: 2.92; 95% CI: 1.67, 5.09), urgency UI (OR: 4.17; 95% CI: 2.18, 7.98), and mixed UI (OR: 4.58; 95% CI: 2.28, 9.22) were higher in women > 50 years of age compared to younger women. Additionally, the risk of developing mixed UI (OR: 2.32; 95% CI: 1.08, 4.99) was higher in diabetic patients compared to nondiabetic ones. Finally, the risks of developing stress UI (OR: 2.07; 95% CI: 1.32, 3.25), urgency UI (OR: 1.52; 95% CI: 1.06, 2.20), and mixed UI (OR: 2.44; 95% CI: 1.32, 4.55) were higher in obese women (BMI ≥ 30 kg/m²) compared to non-obese women (Table 4).
Discussion
The first aim of this study was to determine the rate of UI symptoms. We found that UI symptoms were common in approximately half of the study participants. A few previous studies described the rate of UI among Saudi women, with reported rates ranging from 28% to 41.4% [6, 7, 10, 11]. However, a minority of the study participants who had UI symptoms sought medical care, which apparently failed to treat their symptoms. The possible mentioned reasons for not seeking medical advice included limited accessibility to advanced medical treatment of UI in the KSA (e.g., advanced pelvic physiotherapy modalities and pelvic floor surgeries for UI); a lack of understanding that UI is a medical problem and not a normal phenomenon of age or birth; and/or embarrassment about discussing symptoms with the treating physician [10].
Among our study participants, women with diabetes were mainly older (> 40 years), overweight (≥ 25 kg/m²), and had multiple births, which might contribute to their higher risk of developing urinary incontinence because the obesity and parity that accompany diabetes could put more pressure on the pelvic floor [13]. In addition, diabetes itself could cause peripheral nerve damage, which might precipitate the urgency symptoms that were experienced by our study participants [13]. Future research could perhaps focus on the relationship between diabetes and UI and consider these significant confounders (age, parity, and obesity) as well as differentiate between the two types of diabetes (type I and II) in their longitudinal designs to overcome possible avoidable biases.
In our study, we found that UI symptoms were common among women with the following characteristics: multiparity, at least one abortion, childbirth before ≥ 2 years ago, vaginal delivery (especially assisted), age of ≤ 18 years at first birth and ≥ 35 years at last birth, and a history of macrosomia or episiotomy. Previous studies found that UI symptoms were more common among multiparas and women who had given birth by vaginal delivery [14, 15]. The latter has been associated with a weakening of the pelvic floor muscle during delivery, especially vaginal delivery accompanied by episiotomy [15]. Regarding the number of deliveries, a dose-response effect has been reported in the literature, which means that the risk of UI increases with an increasing number of deliveries regardless of the mode of delivery—although the effect is stronger in vaginal delivery [16]. In addition, macrosomia might increase the strain on the pelvic floor during childbirth, as well as the risk of having an episiotomy, which might further damage the pelvic floor. However, it is still unclear whether performing an elective cesarean to deliver a large baby would minimize the risk of developing UI. Further research is required in this regard, especially because ultrasound imaging is not always accurate in reporting fetal weight [17, 18].
The second aim of this study was to examine the risk of UI types (stress, urgency, and mixed) in relation to obstetric events. We found that the risk of stress UI increased with the following obstetric events: grand multiparity, childbirth before ≥ 2 years ago, vaginal delivery (especially assisted), age at first birth ≤ 18 years, age at last birth ≥ 35 years, episiotomy, and macrosomia. This elevated risk of UI might be explained by the damages to the neuromuscular and facial structures in the pelvic area due to multiple births and during childbirth events [19].
In contrast, we found no association between obstetric events and a risk of developing urgency UI symptoms. The mechanism of urgency or an overactive bladder is still under investigation. The load of obstetric events on the pelvic floor might play only a minor role in this type of UI; the actual mechanism may be more complicated and might involve increased neuron function [20, 21].
Our third aim was to study the risk of developing each UI symptom in relation to obstetric events, as several women presented with various clinical pictures of UI. We found that, in comparison to nulliparous women, frequency, urgency, leakage related to urgency, and pelvic or genital area discomfort were associated with all examined obstetric events except abortion. Another study also found no association between abortion and UI [22]. Nevertheless, although the strain on the pelvic floor and the genital area induced by abortion is less than that induced by delivery, it might play a role in urinary leakage under further pelvic muscle strain, such as when performing various physical activities, as we found in our study. On the other hand, difficulty emptying the bladder was linked only with multigravidity and age at last birth. The exact mechanism of voiding dysfunction in women is not well understood [23]. One of the theories regarding long-lasting postpartum urine retention or difficulty voiding is the occurrence of damage to the pudendus nerve due to childbirth trauma [24].
This study has certain limitations. The inclusion in the questionnaire and investigation of the following symptoms could have added more value to the study: organ prolapse-related symptoms (such as a feeling of a bulge in the vagina, difficulty defecating, and sexual intercourse problems) and nocturnal enuresis, as pelvic organ prolapse symptoms are usually associated with stress incontinence related to obstetric events, whereas nocturnal enuresis usually occurs in patients with overactive bladders or urgency UI. In addition, using an objective measurement to evaluate UI may have produced more accurate results about the presence and type of UI. However, this might be difficult to apply in large settings, such as that of our study. Additionally, a longitudinal design to monitor pregnant women for UI after birth could have prevented possible measurement errors of obstetric events due to recall bias as well as created a temporal sequence that could establish a causal relationship between obstetric events and UI. Having multiple collectors perform the interviews might have affected the data collection consistency and influenced bias, even though the data collectors were trained to unify their approach. This anticipated bias could be raised from unintentional guidance by the interviewers toward the participants’ responses. Finally, in the absence of a computerized appointment system in the PHC regarding the time of data collection, it was difficult to apply simple or systematic random techniques for sampling. However, the collectors were informed to extend their period of data collection (to 1 month) while covering various days of the week and various hours of the day to best reflect the sociodemographic features of the attendees and minimize the magnitude of selection bias. There were several aspects of UI risk factors that were not investigated in this article, including menopause and hormonal imbalance, Kegel exercises, and other treatment modalities as well as the effect of constipation and physical strains on the pelvic floor. Accordingly, the researchers should cover these aspects in future research (especially in the KSA), given that limited relevant studies were found in the literature. Despite these limitations, this study raises concerns about the high prevalence of UI in the Kingdom of Saudi Arabia and the relation between obstetric events and UI, especially since its design included multiple centers and patients with various sociodemographic backgrounds and health indicators.
In conclusion, UI symptoms were common among participants, especially multiparous women with older age, obesity, and diabetes. Unlike urgency incontinence and its symptoms, the risk of stress incontinence and its related symptoms could be linked with obstetric events, which is further aggravated by the presence of health-related risk factors. Further research (preferably including a longitudinal design, objective measurements of UI, and obstetric data extracted from medical reports) is needed to improve our understanding of the development of UI symptoms in relation to obstetric events as well as various health indicators.
References
Nelson HD, Cantor A, Pappas M, Miller L. Screening for urinary incontinence in women: a systematic review for the Women’s Preventive Services initiative. Ann Intern Med. 2018;169(5):311–9.
Abrams P, Andersson KE, Apostolidis A, et al. 6th International Consultation on Incontinence. Recommendations of the international scientific committee: evaluation and treatment of urinary incontinence, pelvic organ prolapse and faecal incontinence. Neurourol Urodyn. 2018;37(7):2271–2.
Krhut J, Gärtner M, Mokris J, et al. Effect of severity of urinary incontinence on quality of life in women. Neurourol Urodyn. 2018;37(6):1925–30.
Osman NI, Chapple CR. Urinary incontinence principles. In: Hamdy F, Eardly I, editors. Oxford textbook of urological surgery. Oxford: Oxford University Press; 2017. p. 244–50.
MacArthur C, Wilson D, Herbison P, et al. Urinary incontinence persisting after childbirth: extent, delivery history, and effects in a 12–year longitudinal cohort study. BJOG. 2016;123(6):1022–9.
Altaweel W, Urinary AM. Incontinence: prevalence, risk factors, and impact on health related quality of life in Saudi women. Neurourol Urodyn. 2017;31(5):642–5.
Dayili AAY, Mohammed A, Mohammed S, et al. Urinary incontinence in healthy Saudi women. EGHM. 2017;69(7):2890–6.
Bradley CS, Rovner ES, Morgan MA, et al. A new questionnaire for urinary incontinence diagnosis in women: development and testing. Am J Obstet Gynecol. 2005;192(1):66–73.
Milsom I, Gyhagen M. The prevalence of urinary incontinence. Climacteric. 2019;22(3):217–22.
Al-Badr A, Brasha H, Al-Raddadi R, Noorwali F, Ross S. Prevalence of urinary incontinence among Saudi women. Int J Gynecol Obstet. 2012;117(2):160–3.
Bakarman MA, Al-Ghamdi SS. The effect of urinary incontinence on quality of life of women at childbearing age in Jeddah, Saudi Arabia. Global J Health Sci. 2016;8(2):281–7.
Uebersax JS, Wyman JF, Shumaker SA, McClish DK. Short forms to assess life quality and symptom distress for urinary incontinence in women: the incontinence impact questionnaire and the urogenital distress inventory. Neurourol Urodyn. 1995;14(2):131–9.
Narayanamurthy V, Slopnick EA, Sheyn DD, Bukavina L, Mishra K, Hijaz AK. Overactive bladder in diabetes mellitus. Current Bladder Dysfunction Reports. 2019;22(10):1–7.
Rortveit G, Daltveit AK, Hannestad YS, Hunskaar S. Urinary incontinence after vaginal delivery or cesarean section. N Engl J Med. 2003;348(10):900–7.
Afshari P, Dabagh F, Iravani M, Abedi P. Comparison of pelvic floor muscle strength in nulliparous women and those with normal vaginal delivery and cesarean section. Int Urogynecol J. 2017;28(8):1171–5.
Rørtveit G, Hannestad YS. Association between mode of delivery and pelvic floor dysfunction. Tidsskrift for den Norske laegeforening: tidsskrift for praktisk medicin, ny raekke. 2014;134(19):1848–52.
Culligan PJ, Myers JA, Goldberg RP, Blackwell L, Gohmann SF, Abell TD. Elective cesarean section to prevent anal incontinence and brachial plexus injuries associated with macrosomia—a decision analysis. Int Urogynecol J. 2005;16(1):19–28.
Campbell S. Fetal macrosomia: a problem in need of a policy. Ultrasound Obstet Gynecol. 2014;43(1):3–10.
Snooks SJ, Swash M, Mathers SE, Henry MM. Effect of vaginal delivery on the pelvic floor: a 5-year follow-up. Br J Surg. 1990;77(12):1358–60.
Michel MC, Chapple CR. Basic mechanisms of urgency: preclinical and clinical evidence. Eur Urol. 2009;56(2):298–308.
Griffiths D, Clarkson B, Tadic SD, Resnick NM. Brain mechanisms underlying urge incontinence and its response to pelvic floor muscle training. J Urol. 2015;194(3):708–15.
Findik RB, Unluer AN, Şahin E, Bozkurt ÖF, Karakaya J, Ünsal A. Urinary incontinence in women and its relation with pregnancy, mode of delivery, connective tissue disease and other factors. Adv Clin Exp Med. 2012;21(2):207–13.
Panicker JN, Anding R, Arlandis S, et al. Do we understand voiding dysfunction in women? Current understanding and future perspectives: ICI-RS 2017. Neurourol Urodyn. 2018;37(S4):S75–85.
Blomstrand M, Boij R, Christensson L, Blomstrand P. Systematic bladder scanning identifies more women with postpartum urinary retention than diagnosis by clinical signs and symptoms. Int J Nurs Midwifery. 2015;7(6):108–15.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Contributions
AA Alghamdi drafted the article and performed the analysis. AA Alghamdi and GF Alyousif contributed equally to the study design, group work supervision, and final draft editing. RL Alghamdi, FA Almulhim, HM Alsadah, JM Almutawaa, and KA Alnakhli contributed equally to the questionnaire design, participant interviews, data collection, literature summarization, and revision of the article’s final draft. NA Almansour helped write and revise the final draft.
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Alghamdi, A.A., Alyousif, G.F., Alghamdi, R.L. et al. The prevalence of urinary incontinence symptoms among multiparous women: a survey of Saudi health-care centers. Int Urogynecol J 32, 403–411 (2021). https://doi.org/10.1007/s00192-020-04443-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-020-04443-w