Abstract
Introduction and hypothesis
Conservative treatment is recommended as first-line therapy for stress urinary incontinence (SUI). We hypothesized that CO2 laser treatment would demonstrate safety and efficacy for women with SUI.
Methods
A prospective, open-label, cohort study of 33 women (mean age 43 years) referred from a continence clinic after urologist/urogynecologist assessment, with a verified stress urinary incontinence diagnosis based on urodynamic testing. The participants completed three outpatient treatments with laser therapy and were subsequently evaluated at 1, 3 and 6 months. The independent t and chi-square tests were used to assess changes in sanitary pad usage and SUI symptoms.
Results
Sanitary pad usage decreased from a median of 12 per day at baseline to 7 at 1–3 months post-treatment (P < 0.0001) and returned to 12 at 6 months post-treatment. Scores on the Urogenital Distress Inventory and the International Consultation of Incontinence Questionnaire decreased (improved) significantly at 1–3 months post-treatment: from 45 ± 2 and 16 ± 4, respectively, to 29.3 ± 14.7 and 8.15 ± 3.1, respectively (P < 0.0001). The scores returned to levels similar to baseline at 6 months after treatment. Participants reported mild and transient side effects, with significant improvement in quality of life.
Conclusions
Laser therapy can be an optional conservative treatment for women who seek minimally invasive non-surgical treatment for the management of SUI. No serious adverse effects were reported though the sample size was not large, a possible limitation of the study. Further large randomized control trials are needed to appraise the efficacy and safety of laser therapy for stress urinary incontinence and to demonstrate the ultimate utility of this modality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
According to the International Continence Society and the International Urogynecology Association, urinary incontinence (UI) is defined as involuntary leakage of urine. The prevalence of UI in women is estimated to reach 40% [1, 2]. UI is associated with several risk factors including older age, vaginal births, high BMI, pelvic floor trauma, constipation, chronic diseases and a history of pelvic floor surgery [2,3,4].
UI has an immense impact on quality of life, including physical, social, economic and psychological aspects [1, 2]. The extent of impact of UI on quality of life depends on both the frequency and the quantity of the leakage and the woman’s experience of the symptoms [5]. Thus, reaching decisions regarding possible intervention depends on a patient’s willingness and desire.
Stress UI (SUI) occurs from pressure on the bladder, such as from coughing, sneezing, running or heavy lifting. Management of SUI may include either conservative or surgical treatment. According to the NICE guidelines, conservative treatment is offered initially, including pelvic muscle training, electrical stimulation or biofeedback [6]. Though these treatments can attain excellent results, the majority of patients fail to improve to a sufficient level because of low compliance [5, 6]. Following failure of conservative treatment for SUI, surgical treatment may be offered. Surgical treatment options include mid-urethral slings, Burch colpo-suspension and the autologous rectus fascial sling. Mid-urethral slings have gained popularity and have been declared the operation of choice in the past decade, especially because of the high success rate and minimally invasive nature of the procedure. Though reasonably effective in treating SUI, several complications may arise after surgical treatment including infection, bleeding, pain, urethral or vaginal discharge, voiding dysfunction and mesh exposure [1, 3, 7,8,9]. These complications enhance patients’ reluctance to undergo surgical interventions. In addition, public concern has increased regarding surgeries that utilize mesh because of the unknown risk of long-term complications. Based on their own investigation and on a Cochrane systematic review [10], the US Food and Drug Administration (FDA) has implemented stricter regulations for the use of vaginal mesh implants and has removed a number of implants from the market [11].
As the future of mid-urethral slings remains uncertain, the need for alternative treatment has become well recognized. In the past few years, energy-based devices for treating SUI, including laser- and radiofrequency- based devices, have gained popularity. Several prospective open-label clinical case series have assessed the efficacy and short-term safety of various modalities of laser treatment, with conflicting results. Randomized controlled trials are noticeably lacking. Laser treatment has been studied for treatment of various gynecological indications including genitourinary syndrome of menopause, vulvovaginal atrophy, SUI, vaginal rejuvenation or tightening and vestibulo/vulvodynia, with varying efficacies [12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28]. The effect of laser treatment at a histological level is described as a local inflammatory response, leading to rapid contraction of collagen fibers, shrinkage of the exposed tissue and increased collagen and elastin production [29,30,31,32].
The aim of the current study was to evaluate the efficacy and safety of CO2 laser treatment for women with SUI. We hypothesized that CO2 laser treatment would demonstrate safety and efficacy for women with SUI up to 6 months post-treatment, as demonstrated by the absence of adverse events and the reduction of symptoms.
Materials and methods
Study design and characteristics of the study participants
This single-center, prospective, open-label, cohort study was conducted between September 2017 and February 2019. The local Helsinki ethics committee approval number was 0205–16-RMB, and the clinicaltrials.gov registration number was NCT02861391. Written informed consent was obtained from all participants prior to screening. Similar pre-treatment assessment and procedures were carried out for all participants, including a urine culture, PAP smear, urodynamic testing and a thorough gynecological examination.
Patients were referred from the continence clinic after assessment by a urologist or urogynecologist to participate in the study screening process. The study included women ages 18–52 years with a verified pure SUI diagnosis based on urodynamic testing, cough test and patient history. Exclusion criteria included mixed incontinence, pregnancy/up to 2 years postpartum, recurrent urinary tract infections, pelvic inflammatory diseases, and vaginal surgery or an unexplained vaginal bleeding episode during the 9 months prior to initiation of the study.
Study intervention
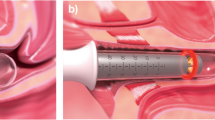
Women meeting the study eligibility criteria received three outpatient treatments with the Lumenis Acupulse System with the FemTouch vaginal handpiece (cleared by the US FDA). Laser therapy was delivered circumferentially to the entire length of the vaginal mucosal surface. Each treatment took up to 5 min to complete, and all participants completed all three treatments. Neither pre- or posttreatment medications were required. Study participants were requested to refrain from vaginal intercourse or tampon use for a period of 14 days following each treatment. The interval between treatments was 4 weeks based on company specifications and previous study history. All participants attended follow-up visits at 1, 3 and 6 months after completion of the treatment protocol. All laser treatments were performed by a single doctor with previous training with laser devices.
Study outcomes
The primary outcomes were changes in sanitary pad usage and in scores on the Urogenital Distress Inventory (UDI6) and the International Consultation of Incontinence Questionnaire (ICIQ-UI). These are widely accepted, validated, global assessment tools used in SUI studies. The maximal score in ICIQ-UI is 21. This questionnaire accesses reasons for SUI, incidence, frequency and the impact on daily lifestyle. A higher score indicates more impact. The UDI6 questionnaire comprises six questions about frequency, urgency, amount of leakage, difficulty emptying the bladder and pain, which sums to a total score of 0–75. A higher score indicates worse symptoms.
All participants in the study filled the UDI6 and ICIQ-UI during the screening visit (baseline), prior to the second and third treatments, and at 1, 3 and 6 months after completing all treatments. All participants underwent the cough test and urodynamic testing before the first treatment and at the 3-month follow-up visit. Adverse events were also recorded at each study interval. Pain was assessed on a 10-point visual analog scale (VAS) immediately after each treatment.
Statistical analyses
SPSS for Windows version 18 (SPSS, Inc., Chicago, IL) was used for data management and statistical analysis. The independent t and chi-square association tests were used to compare between independent groups of continuous and categorical variables, respectively. All tests were two-sided and considered significant at the 0.05 level.
Group size was calculated by an a priori power analysis aimed at 90% power. To allow a difference of 16 changes on the UDI score following laser treatment, we used an effect size of 16 based on minimal important differences [33] at a two-sided significance level of 5% for each of the variables examined. Accordingly, for a sample size of 30 participants, we recruited 35 participants, considering a loss to follow-up of 15%.
Results
Of the 67 women screened for the study, 35 were found eligible and willing to participate. Two participants were lost to follow-up, and 33 women were included in the final analysis. Demographic and clinical characteristics of the participants are presented in Table 1. Their mean age was 43 years.
The baseline mean UDI-6 score was 45 ± 2, with a statistically significant improvement to 29 ± 15 (P < 0.0001) at 3 months post-treatment and a return to the baseline UDI-6 score 6 months post-treatment (Table 2, Fig. 1). These changes were observed in all participants.
The baseline mean ICIQ-UI score was 16 ± 4. A statistically significant improvement to 8 ± 3 (P < 0.0001) was observed at 3 months post-treatment and a return to baseline ICIQ-UI score at 6 months post-treatment (Table 2, Fig. 1).
Median sanitary pad usage decreased significantly from 12 (range: 6–18) per day before study commencement to 7 (range: 2–10) per day at 3 months post-treatment (P < 0.0001) and returned to the baseline frequency of 12 per day at 6 months post-treatment (Table 2, Fig. 1). At 6 months post-treatment, 80% of the participants contacted the study team to inquire regarding an option for additional treatments. Since additional treatments were not part of the study protocol, these patients were referred to a parallel study.
Most participants (80%) reported a suction sensation during internal laser treatment, and these same women reported a stinging sensation during external laser treatment. Reported treatment discomfort, assessed as pain, according to the VAS did not exceed 3 during or after treatments. Immediate adverse effects reported by the participants included a stinging sensation that lasted up to 13 min (70%), vulvar sensitivity that lasted up to 3 days (30%) and untimely menstrual pain (10%). No complications were reported during the 6-month follow-up period. No vaginal or urinary tract infections were reported during the study period.
Discussion
This study demonstrated improvement in urinary symptoms at 3 months following three CO2 laser treatments for all participants. This improvement is evident in the scores on questionnaires and in the decreased frequency of sanitary pad usage. The median number of pads decreased significantly from 12 per day before study commencement to 7 per day at 3 months post-treatment. These findings concur with other studies [24, 34,35,36,37,38,39]. The strength of the current study compared with previous studies is the homogeneous premenopausal population. In addition, only patients with pure SUI were included while patients with mixed incontinence were excluded. Furthermore, all patients underwent pre- and post-treatment urodynamic testing for treatment efficiency evaluation. Studies regarding the effect of lasers on SUI complaints in postmenopausal women are required.
Subjective improvement was demonstrated in quality of life after the treatment session. In addition, a positive trend was evident in urodynamic testing but not in stress tests. Two previous studies comprised a total of 133 patients examined the correlation between urodynamics and validated questionnaires, with inconsistent results. Follow-up periods lasted 6 months post-treatment, and improvement rates were 60% in urodynamic testing and 80% according to subjective reports, with a moderate decrease in treatment effect 6 months post-treatment [40, 41]. Although the changes reported herein were subjective, they are relevant, since the main purpose of the treatment was improvement in quality of life.
Another encouraging finding of this study was that the majority (80%) of participants asked for a follow-up treatment. Their motivation to undergo more treatments is due to the significant improvement in quality of life and the only mild and transient side effects.
Previous studies of laser treatment for SUI generally included short-term follow-up of up to 3–6 months post-treatment. These studies comprised a total of 154 patients and demonstrated temporary treatment effects, which were sustained for a few months post-treatment with reported SUI recurrence 6 months post-treatment [23, 24, 35, 36]. These findings concur with those of the current study, specifically, the recurrence of symptoms to levels similar to baseline, at 6 months post-treatment. Larger studies are needed to assess the long-term sustained efficacy of laser treatment. Since the reason for the the short-term effect remains a mystery, studies including protocols with additional treatments may prove to be beneficial and enable the establishment of a long-term treatment program that may allow patients to plan ahead both clinically with their physicians and financially with their family and insurance. Notably, the FDA and the International Urogynecology Association issued a warning about the use of energy-based devices, such as radiofrequency and laser treatment, to perform vaginal “rejuvenation,” cosmetic procedures and non-surgical vaginal procedures. This is because the safety and effectiveness of these treatments for long-term use have not been established [42].
This study has a number of limitations. Due to the small sample size, the findings may not reflect the true efficacy and safety of the treatment. In addition, the lack of a sham laser control group does not enable evaluating the placebo effect of the treatment. Furthermore, the follow-up period was only 6 months post-treatment. Also, power calculations were based on the Chinese language UDI-6 and the MID reported there. Using the UDI-stress subscale in English might have been a more precise method of evaluating change in SUI specifically and has a set MID.
Conclusion
Laser therapy is an optional conservative treatment for women who seek minimally invasive non-surgical treatment for SUI. Its use is associated with only mild and transient adverse effects.
In the current study, urinary symptoms after treatment with CO2 laser were evaluated by urodynamic testing, questionnaires and sanitary pad usage. Statistically significant improvement at 3 months post-treatment was shown, and a return to baseline at 6 months post-treatment. Thus, further large randomized control trials are needed to appraise the efficacy and safety of laser therapy for stress urinary incontinence and to demonstrate the ultimate utility of this modality.
References
Castro RA, Arruda RM, Bortolini MA. Female urinary incontinence: effective treatment strategies. Climacteric: the journal of the International Menopause Society. 2015;18:135–41.
MacLennan AH, Taylor AW, Wilson DH, Wilson D. The prevalence of pelvic floor disorders and their relationship to gender, age, parity and mode of delivery. BJOG: an international journal of obstetrics and gynaecology. 2000;107:1460–70.
Norton P, Brubaker L. Urinary incontinence in women. Lancet. 2006;367:57–67.
Nystrom E, Sjostrom M, Stenlund H, Samuelsson E. ICIQ symptom and quality of life instruments measure clinically relevant improvements in women with stress urinary incontinence. Neurourol Urodyn. 2015;34:747–51.
Gil KM, Somerville AM, Cichowski S, Savitski JL. Distress and quality of life characteristics associated with seeking surgical treatment for stress urinary incontinence. Health Qual Life Outcomes. 2009;7:8.
Urinary incontinence and pelvic organ prolapse in women: management National Institute for Health and Care Excellence (NICE) guideline [NG123].
Bump RC, Norton PA, Zinner NR, Yalcin I. Mixed urinary incontinence symptoms: urodynamic findings, incontinence severity, and treatment response. Obstet Gynecol. 2003;102:76–83.
Schimpf MO, Rahn DD, Wheeler TL, et al. Sling surgery for stress urinary incontinence in women: a systematic review and metaanalysis. Am J Obstet Gynecol. 2014;211:71 e1–71 e27.
Barski D, Gerullis H, Georgas E, et al. Coating of mesh grafts for prolapse and urinary incontinence repair with autologous plasma: exploration stage of a surgical innovation. Biomed Res Int. 2014;2014:296498.
Maher C, Feiner B, Baessler K, Christmann-Schmid C, Haya N, Brown J. Surgery for women with anterior compartment prolapse. Cochrane Database Syst Rev. 2017;11:Cd004014.
Surgical Mesh for Transvaginal Repair of Pelvic Organ Prolapse in the Anterior Vaginal Compartment. FDA Executive Summary. https://www.fda.gov/media/122854. Accessed July 20 2019.
Arunkalaivanan A, Kaur H, Onuma O. Laser therapy as a treatment modality for genitourinary syndrome of menopause: a critical appraisal of evidence. Int Urogynecol J. 2017;28:681–5.
Gambacciani M, Levancini M. Short-term effect of vaginal erbium laser on the genitourinary syndrome of menopause. Minerva Ginecol. 2015;67:97–102.
Salvatore S, Nappi RE, Zerbinati N, et al. A 12-week treatment with fractional CO2 laser for vulvovaginal atrophy: a pilot study. Climacteric: the journal of the International Menopause Society. 2014;17:363–9.
Salvatore S, Leone Roberti Maggiore U, Athanasiou S, et al. Histological study on the effects of microablative fractional CO2 laser on atrophic vaginal tissue: an ex vivo study. Menopause. 2015;22:845–9.
Hutchinson-Colas J, Segal S. Genitourinary syndrome of menopause and the use of laser therapy. Maturitas. 2015;82:342–5.
Pieralli A, Fallani MG, Becorpi A, et al. Fractional CO2 laser for vulvovaginal atrophy (VVA) dyspareunia relief in breast cancer survivors. Arch Gynecol Obstet. 2016;294:841–6.
Arroyo C. Fractional CO2 laser treatment for vulvovaginal atrophy symptoms and vaginal rejuvenation in perimenopausal women. Int J Women’s Health. 2017;9:591–5.
Pagano T, De Rosa P, Vallone R, et al. Fractional microablative CO2 laser for vulvovaginal atrophy in women treated with chemotherapy and/or hormonal therapy for breast cancer: a retrospective study. Menopause. 2016;23:1108–13.
Gambacciani M, Levancini M. Vaginal erbium laser as second-generation thermotherapy for the genitourinary syndrome of menopause: a pilot study in breast cancer survivors. Menopause. 2017;24:316–9.
Sokol ER, Karram MM. An assessment of the safety and efficacy of a fractional CO2 laser system for the treatment of vulvovaginal atrophy. Menopause. 2016;23:1102–7.
Salvatore S, Nappi RE, Parma M, et al. Sexual function after fractional microablative CO(2) laser in women with vulvovaginal atrophy. Climacteric: the journal of the International Menopause Society. 2015;18:219–25.
Fistonic N, Fistonic I, Gustek SF, et al. Minimally invasive, non-ablative Er:YAG laser treatment of stress urinary incontinence in women--a pilot study. Lasers Med Sci. 2016;31:635–43.
Ogrinc UB, Sencar S, Lenasi H. Novel minimally invasive laser treatment of urinary incontinence in women. Lasers Surg Med. 2015;47:689–97.
Filippini M, Del Duca E, Negosanti F, et al. Fractional CO2 laser: from skin rejuvenation to Vulvo-vaginal reshaping. Photomed Laser Surg. 2017;35:171–5.
Lee MS. Treatment of vaginal relaxation syndrome with an erbium:YAG laser using 90 degrees and 360 degrees scanning scopes: a pilot Study & Short-term Results. Laser therapy. 2014;23:129–38.
Lev-Sagie A, Kopitman A, Brzezinski A. Low-level laser therapy for the treatment of provoked Vestibulodynia-a randomized, placebo-controlled pilot trial. J Sex Med. 2017;14:1403–11.
Murina F, Karram M, Salvatore S, Felice R. Fractional CO2 laser treatment of the vestibule for patients with Vestibulodynia and genitourinary syndrome of menopause: a pilot study. J Sex Med. 2016;13:1915–7.
Drnovsek-Olup B, Beltram M, Pizem J. Repetitive Er:YAG laser irradiation of human skin: a histological evaluation. Lasers Surg Med. 2004;35:146–51.
Zerbinati N, Serati M, Origoni M, et al. Microscopic and ultrastructural modifications of postmenopausal atrophic vaginal mucosa after fractional carbon dioxide laser treatment. Lasers Med Sci. 2015;30:429–36.
Poon VK, Huang L, Burd A. Biostimulation of dermal fibroblast by sublethal Q-switched Nd:YAG 532 nm laser: collagen remodeling and pigmentation. J Photochem Photobiol B. 2005;81:1–8.
Jiang X, Ge H, Zhou C, Chai X, Ren QS. The role of vascular endothelial growth factor in fractional laser resurfacing with the carbon dioxide laser. Lasers Med Sci. 2012;27:599–606.
Chan SS, Cheung RY, Lai BP, Lee LL, Choy KW, Chung TK. Responsiveness of the pelvic floor distress inventory and pelvic floor impact questionnaire in women undergoing treatment for pelvic floor disorders. Int Urogynecol J. 2013 Feb;24(2):213–21.
Lin HY, Tsai HW, Tsui KH, et al. The short-term outcome of laser in the management of female pelvic floor disorders: focus on stress urine incontinence and sexual dysfunction. Taiwanese journal of obstetrics & gynecology. 2018;57:825–9.
Lin KL, Chou SH, Long CY. Effect of Er:YAG laser for women with stress urinary incontinence. Biomed Res Int. 2019;2019:7915813.
Blaganje M, Scepanovic D, Zgur L, Verdenik I, Pajk F, Lukanovic A. Non-ablative Er:YAG laser therapy effect on stress urinary incontinence related to quality of life and sexual function: a randomized controlled trial. Eur J Obstet Gynecol Reprod Biol. 2018;224:153–8.
Lin YH, Hsieh WC, Huang L, Liang CC. Effect of non-ablative laser treatment on overactive bladder symptoms, urinary incontinence and sexual function in women with urodynamic stress incontinence. Taiwanese journal of obstetrics & gynecology. 2017;56:815–20.
Gonzalez Isaza P, Jaguszewska K, Cardona JL, Lukaszuk M. Long-term effect of thermoablative fractional CO2 laser treatment as a novel approach to urinary incontinence management in women with genitourinary syndrome of menopause. Int Urogynecol J. 2018;29:211–5.
Gaspar A, Brandi H. Non-ablative erbium YAG laser for the treatment of type III stress urinary incontinence (intrinsic sphincter deficiency). Lasers Med Sci. 2017;32:685–91.
Neimark AI, Yakovleva AY, Lapii GA. Outcomes of ER:YAG LASER treatment of stress urinary incontinence in women. Urologiia. 2018:20–5.
Tien YW, Hsiao SM, Lee CN, Lin HH. Effects of laser procedure for female urodynamic stress incontinence on pad weight, urodynamics, and sexual function. Int Urogynecol J. 2017;28:469–76.
US Food and Drug Administration. FDA Warns Against Use of Energy-Based Devices to Perform Vaginal “Rejuvenation” or Vaginal Cosmetic Procedures [Internet]. FDA Safety Communications.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dabaja, H., Lauterbach, R., Matanes, E. et al. The safety and efficacy of CO2 laser in the treatment of stress urinary incontinence. Int Urogynecol J 31, 1691–1696 (2020). https://doi.org/10.1007/s00192-019-04204-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-019-04204-4