Abstract
Laparoscopic ventral mesh rectopexy (VMR) has become a popular surgical technique for treating women with full-thickness rectal prolapse with a low recurrence rate, as demonstrated by several studies. In addition, it is increasingly applied to female patients with obstructive defecation syndrome (ODS) caused by intussusception ± rectocele. Functional improvement can be achieved in a high number of patients with ODS, but expectations need to be discussed carefully, as a few patients may not benefit at all. In particular, long-term data on functional outcome and complications following laparoscopic VMR for ODS are still lacking in the literature. Notably, laparoscopic VMR appears to be better than alternative operations for prolapse, intussusception, and rectocele in terms of efficacy, recurrence rates, and adverse effects, but there is a lack of evidence directly comparing techniques through randomized controlled trials; thus, its exact role stills needs to be defined in the future.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the last decade, laparoscopic ventral mesh rectopexy (VMR) has become a popular surgical technique for treating women with full-thickness rectal prolapse, especially in Europe. Although long-term data are still limited, available studies showed promising results, with low recurrence rates and improved functional outcomes [1]. In addition, laparoscopic VMR has also been applied to female patients with obstructive defecation syndrome (ODS) due to intussusception ± anterior rectoceles [2]. Again, several studies reported good results with enhanced defecation and less faecal incontinence following surgical repair [3]. Particularly, the preservation of the lateral ligaments and their autonomic nerves by avoiding posterolateral rectal mobilization is considered to reduce the risk of postoperative constipation [4]. This is a clear advantage over alternative abdominal rectopexy procedures, where posterior rectal mobilization is usually required.
Notably, pelvic organ prolapse commonly affects multiple compartments including both rectal and urogenital prolapse [5,6,7]. Thus, combined procedures of colorectal and urogynecological surgeons to correct anatomical alterations are often necessary to achieve the best outcome for the patients. Indeed, a recent study assessing robot-assisted sacrocolporectopexy for multicompartment prolapse, performed by both specialities, revealed improved functional outcome, quality of life, and sexual function postoperatively [6].
New techniques tend to quickly become popular throughout the surgical community, although clinical outcome, and especially long-term data, are not available. Therefore, it is of immense importance to perform clinical well-designed studies to constantly and objectively re-evaluate the efficacy and the complication rate associated with the procedure.
Words of caution
In general, laparoscopic VMR is considered to be a safe technique, which can even be conducted as a day-case operation in selected patients by experienced colorectal surgeons [8]. However, complications do occur and can potentially lead to serious consequences for affected patients. In particular, mesh-related morbidity needs to be taken into account and discussed with the patients. A large multicentre collaboration including 2,200 patients revealed a mesh erosion rate of 2%, requiring local excision, low anterior resections or the creation of stomata [9]. In the same analysis, the authors identified that polyester mesh was associated with a significantly higher incidence of mesh erosion than polypropylene, titanium-coated polypropylene or biological grafts. In addition, it was speculated that the use of non-absorbable stitches further increased the risk of infections and subsequently erosion. In a systematic review evaluating the safety of laparoscopic VMR, no significant differences between biological and synthetic meshes in terms of recurrence and mesh complications were reported [10]. However, current evidence may suggest that choosing a biological graft with absorbable suture material is the best option for reducing the risk of certain adverse events.
Another large study comprising patients operated on between 1999 and 2013 observed mesh-related complications in 4.6% [1]. In 5 of these patients, laparoscopic VMR was combined with a perineotomy to correct low rectoceles. Van der Hagen et al. evaluated transvaginal posterior colporrhaphy combined with laparoscopic ventral mesh rectopexy for isolated grade III rectocele [11]. They reported improved ODS scores, but the short-term follow-up and the small number of patients enrolled limited its clinical conclusion. Overall, it would be reasonable not to combine perineal or vaginal procedures with laparoscopic VMR, as the risk of developing mesh complications tends to be higher.
Ongoing pain was another adverse event revealed by Evans et al. and was observed in about 2% of patients [9]. Most can usually be managed conservatively with analgesics; however, others may undergo detailed radiological evaluation and even laparoscopic exploration. Notably, no operation is without risk, but procedures for functional disorders in particular are expected to cause no harm.
Functional consideration
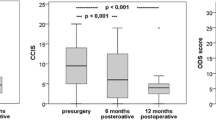
Laparoscopic VMR for ODS caused by rectocele and/or intussusception can ease defecation disorders and improve faecal incontinence, as demonstrated by several studies [1, 3, 12]. However, functional outcome was measured in various ways, using either self-reporting questions or scoring systems of various qualities; thus, the comparison of data remains challenging. A recent review showed improvement of ODS following surgery ranging from 52% to 84.2% [3]. Furthermore, a systematic review found the overall weighted mean decrease in constipation rate after surgery to be 23.9% [13]. It is noteworthy that new onset constipation was noted in a few studies as well.
Clearly, there are many other factors crucial to successful evacuation, including appropriate neurological function—merely restoring anatomical position is unable to reverse ODS secondary to neurological dysmotility [14]. Although laparoscopic VMR is beneficial for many, a significant number of patients still have significant difficulties with defecation and voluntary control of their stool, a question is how to select those patients who will benefit from this type of procedure. Interestingly, there is a lack of studies aimed at defining risk factors for a less successful outcome after laparoscopic VMR. Some patients with a long history of constipation or a considerable birth trauma may develop severe nerve damage potentially because of the extensive stretching, resulting in an “non-functional” rectum [14, 15]. This group of patients may continue to have functional impairment, despite correction of anatomical alterations. Faecal incontinence can also be caused by various pathological conditions, such as sphincter defects following birth trauma or anal surgery, neurological disorders, diarrhoea or inflammatory changes with subsequent loss of reservoir capacity and alterations in anorectal sensation [16]. Therefore, careful clinical workup is essential before definite treatment.
Alternatives to keep in mind
A large number of techniques have been published that treat symptomatic rectoceles and/or intussusceptions with various approaches ranging from abdominal, transanal, transvaginal to perineal [17]. No clear consensus over the ideal access for optimal management has been reached.
The stapled transanal resection (STARR) has become popular in the last decades too, with promising functional results as reported by several studies [18]. A large series from the Stapled Transanal Resection Registry involving 2,838 patients revealed a significant improvement according to the ODS questionnaire from 15.8 before to 4 points 1 year after surgery [19]. However, complications occurred in up to 36%, including septic events in 4.4%. Furthermore, STARR may lead to persistent urgency and faecal incontinence, which has a significant impact on the patient’s quality of life.
Internal Delorme’s procedure is still a good alternative, with reasonably low postoperative complication rates [20]. However, the recurrence rate seems to increase with a longer follow-up.
Gynaecologists tend to repair a rectocele through the vagina, with little workup on co-existing intussusceptions. It is noteworthy that a pilot randomized controlled trial found comparable results for transanal and vaginal rectocele repair, although a trend was detected towards fewer symptoms in the vaginal group [21]. This highlights the importance of joint pelvic floor multidisciplinary meetings to discuss patients with combined anatomical disorders and to find the appropriate treatment for each one.
Conclusion
In general, laparoscopic VMR appears to be a safe procedure, with a small number of immediate complications. However, mesh-related adverse events may occur in the years following surgery and can lead to severe consequences for affected patients. It can be speculated that choosing a biological graft with absorbable suture material is the best option for reducing a complicated outcome.
Functional improvement can be achieved in a high number of female patients with ODS, but expectations needs to be carefully discussed and a few patients may not benefit at all. Its advantage over alternative procedures is not clearly demonstrated and future randomized controlled trials may be necessary to define the role of laparoscopic VMR. Studies of risk factors for the success or failure of specific procedures are also required, to guide clinicians and patients to the optimal procedure for each individual.
References
Consten EC, van Iersel JJ, Verheijen PM, Broeders IA, Wolthuis AM, D’Hoore A. Long-term outcome after laparoscopic ventral mesh rectopexy: an observational study of 919 consecutive patients. Ann Surg. 2015;262(5):742–747; discussion 747–748. doi:10.1097/SLA.0000000000001401.
Makela-Kaikkonen JK, Rautio TT, Koivurova S, Paakko E, Ohtonen P, Biancari F, et al. Anatomical and functional changes to the pelvic floor after robotic versus laparoscopic ventral rectopexy: a randomised study. Int Urogynecol J. 2016;27(12):1837–45. doi:10.1007/s00192-016-3048-y.
Van Iersel JJ, Paulides TJ, Verheijen PM, Lumley JW, Broeders IA, Consten EC. Current status of laparoscopic and robotic ventral mesh rectopexy for external and internal rectal prolapse. World J Gastroenterol. 2016;22(21):4977–87. doi:10.3748/wjg.v22.i21.4977.
Boons P, Collinson R, Cunningham C, Lindsey I. Laparoscopic ventral rectopexy for external rectal prolapse improves constipation and avoids de novo constipation. Colorectal Dis. 2010;12(6):526–32. doi:10.1111/j.1463-1318.2009.01859.x.
Guzman Rojas R, Kamisan Atan I, Shek KL, Dietz HP. The prevalence of abnormal posterior compartment anatomy and its association with obstructed defecation symptoms in urogynecological patients. Int Urogynecol J. 2016;27(6):939–44. doi:10.1007/s00192-015-2914-3.
Van Iersel JJ, de Witte CJ, Verheijen PM, Broeders IA, Lenters E, Consten EC, et al. Robot-assisted sacrocolporectopexy for multicompartment prolapse of the pelvic floor: a prospective cohort study evaluating functional and sexual outcome. Dis Colon Rectum. 2016;59(10):968–74. doi:10.1097/DCR.0000000000000669.
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J. 2010;21(1):5–26. doi:10.1007/s00192-009-0976-9.
Powar MP, Ogilvie JW Jr, Stevenson AR. Day-case laparoscopic ventral rectopexy: an achievable reality. Colorectal Dis. 2013;15(6):700–6. doi:10.1111/codi.12110.
Evans C, Stevenson AR, Sileri P, Mercer-Jones MA, Dixon AR, Cunningham C, et al. A multicenter collaboration to assess the safety of laparoscopic ventral rectopexy. Dis Colon Rectum. 2015;58(8):799–807. doi:10.1097/DCR.0000000000000402.
Smart NJ, Pathak S, Boorman P, Daniels IR. Synthetic or biological mesh use in laparoscopic ventral mesh rectopexy—a systematic review. Colorectal Dis. 2013;15(6):650–4. doi:10.1111/codi.12219.
Van der Hagen SJ, van Gemert WG, Soeters PB, de Wet H, Baeten CG. Transvaginal posterior colporrhaphy combined with laparoscopic ventral mesh rectopexy for isolated grade III rectocele: a prospective study of 27 patients. Colorectal Dis. 2012;14(11):1398–402. doi:10.1111/j.1463-1318.2012.03023.x.
Gosselink MP, Joshi H, Adusumilli S, van Onkelen RS, Fourie S, Hompes R, et al. Laparoscopic ventral rectopexy for faecal incontinence: equivalent benefit is seen in internal and external rectal prolapse. J Gastrointest Surg. 2015;19(3):558–63. doi:10.1007/s11605-014-2696-9.
Samaranayake CB, Luo C, Plank AW, Merrie AE, Plank LD, Bissett IP. Systematic review on ventral rectopexy for rectal prolapse and intussusception. Colorectal Dis. 2010;12(6):504–12. doi:10.1111/j.1463-1318.2009.01934.x.
Gladman MA, Scott SM, Williams NS, Lunniss PJ. Clinical and physiological findings, and possible aetiological factors of rectal hyposensitivity. Br J Surg. 2003;90(7):860–6. doi:10.1002/bjs.4103.
Engel AF, Kamm MA. The acute effect of straining on pelvic floor neurological function. Int J Colorectal Dis. 1994;9(1):8–12.
Saldana Ruiz N, Kaiser AM. Fecal incontinence—challenges and solutions. World J Gastroenterol. 2017;23(1):11–24. doi:10.3748/wjg.v23.i1.11.
Riss S, Stift A. Surgery for obstructed defecation syndrome—is there an ideal technique. World J Gastroenterol. 2015;21(1):1–5. doi:10.3748/wjg.v21.i1.1.
Liu WC, Wan SL, Yaseen SM, Ren XH, Tian CP, Ding Z, et al. Transanal surgery for obstructed defecation syndrome: literature review and a single-center experience. World J Gastroenterol. 2016;22(35):7983–98. doi:10.3748/wjg.v22.i35.7983.
Jayne DG, Schwandner O, Stuto A. Stapled transanal rectal resection for obstructed defecation syndrome: one-year results of the European STARR registry. Dis Colon Rectum. 2009;52(7):1205–1212; discussion 1212–1204. doi:10.1007/DCR.0b013e3181a9120f.
Heriot AG, Skull A, Kumar D. Functional and physiological outcome following transanal repair of rectocele. Br J Surg. 2004;91(10):1340–4. doi:10.1002/bjs.4543.
Nieminen K, Hiltunen KM, Laitinen J, Oksala J, Heinonen PK. Transanal or vaginal approach to rectocele repair: a prospective, randomized pilot study. Dis Colon Rectum. 2004;47(10):1636–42.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
Riss, S., Winstanley, J. & Collie, M. Laparoscopic ventral mesh rectopexy for obstructive defecation syndrome: still the way to go?. Int Urogynecol J 28, 979–981 (2017). https://doi.org/10.1007/s00192-017-3378-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-017-3378-4