Abstract
Introduction and hypothesis
To estimate the incidence rates of stress urinary incontinence (SUI) surgery among Finnish women from 1987 to 2009 by age, and to evaluate the trends in SUI surgery.
Methods
We conducted a retrospective register-based study. All SUI procedures on adult women over age 18 years in Finland were identified from the nationwide Care Register for Health Care. Age-specific incidence rates per 1,000 women were calculated for each year. The cumulative incidence of SUI surgery was calculated.
Results
There were 38,340 procedures for SUI in 1987–2009. The overall age-adjusted incidence rate increased 2.6-fold from 0.5/1,000 women in 1987 to 1.3/1,000 in 2002, but declined thereafter by 2009 to 0.8/1,000. There was a six-fold increase in the incidence rate in the age group 60–69 years and a ten-fold increase in the age group 70–79 years from 1987 to 2002. These marked increases in operation rates coincided with the increased use of tension-free vaginal tape (TVT). In 2002, TVT accounted for 96 % of all SUI procedures. Mid-urethral slings with transobturator techniques surpassed TVT in popularity in 2007. The life-long cumulative incidence of SUI surgery was 9.9 % in 2002 and 6.3 % in 2009.
Conclusions
The incidence rates of SUI surgery increased significantly in Finland, especially among women aged 60 to 79 years. Mid-urethral slings have become the dominant procedure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
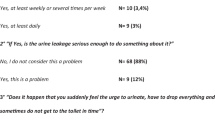
Stress urinary incontinence (SUI) is defined as an involuntary leakage of urine on straining, physical activity, and sneezing or coughing [1]. It is a common problem among women of all ages with an overall prevalence of 20–25 % [2, 3]. The reported prevalence of SUI varies with age, and is highest among women aged 40–59 years (16–36 %), and slightly lower in younger (20–39 years, rate 4–23 %) and older (60–79 years, rate 8–23 %) age groups [4]. SUI affects the daily life of women; it has an impact on recreational activities, such as sports and social events, and sexual function. The quality of life deteriorates as symptoms become more bothersome [5, 6]. In addition, there are substantial costs involved in incontinence pads, diapers and hygiene products for women with SUI [7].
The widely cited study by Olsen et al. [8] found that the risk for a woman to have undergone at least one surgical procedure for either SUI or pelvic organ prolapse by the age of 79 years was 11.1 %, based on surgery rates in 1995. Since then, the number of surgical procedures for SUI has increased in several countries [9–13] and a recent study by Wu et al. estimates the lifelong risk for SUI surgery to be 13.6 % by the age of 80 [14]. Burch colposuspension used to be the gold standard procedure for the surgical treatment of SUI, but since the late 1990s, surgical practices have changed and mid-urethral slings have replaced the traditional method.
The objective of this study was to examine the current changes in the surgical treatment of SUI in Finland. Our aim was to establish the trends in the operative management of SUI over 23 years (from 1987 to 2009). We also looked at the age-specific rates and cumulative incidences of SUI surgery at this time.
Materials and methods
We conducted a register-based study to identify surgical procedures for SUI among the adult female population in Finland in 1987–2009. Data were obtained from the Care Register for Health Care kept by the National Institute for Health and Welfare (THL), a research and development institute under the Finnish Ministry of Social Affairs and Health. Data collection on health registers is regulated by law, and all health care institutions are obliged to submit the requested information regarding hospital care to the register. THL functions as the statistical authority who maintains data files and registers. The Care Register for Health Care (before 1994 known as the Hospital Discharge Register) collects data on all inpatient care provided by public and private hospitals and health care centers in Finland. Specialized outpatient care (since 1998) including day surgeries (since 1994) are detailed in the same register. Although the Care Register has more comprehensive data than its predecessor, the most essential data concerning patients, admission and discharge dates, diagnoses, and procedure codes have remained unchanged.
We used the Care Register to identify all surgical procedures performed for SUI in Finland on women aged 18 years or older from 1987 to 2009. The first classification of surgical procedures was published in Finland in 1983 and it included nine procedure codes for stress incontinence surgery. This classification was replaced by the Finnish version of the NOMESCO (Nordic Medico-Statistical Committee) Classification of Surgical Procedures introduced in 1997 and it included 17 procedures for anti-incontinence surgery. This version of the NOMESCO Classification of Surgical Procedures was revised in 2004. Additional codes were entered to include new surgical methods: tension-free vaginal tape (TVT) in 1997, the outside-in transobturator tape technique (TOT) in 2003, and the inside-out transobturator technique (TVT-O) in 2004. The procedures were grouped into four groups (Burch colposuspension, TVT, transobturator tap, and others). Tables 1 and 2 show the listing and grouping of procedure codes.
We searched the Care Register to identify all hospitalization episodes, which included a procedure for SUI. Procedures performed in both inpatient and outpatient settings are included. The register data include an encrypted identification number for each patient; repeated operations for the same patient can be identified and were excluded, as only the primary operations included in these analyses. Those women with more than one procedure code for SUI surgery for the same date were excluded. Patients with concomitant cystoscopy, operation for prolapse or surgery for reasons other than SUI are included. We calculated the annual rates for different SUI surgery procedures. For the estimation of the incidence of age-specific surgery, we obtained statistics on Finnish women by age and by year from the Population Database kept by Statistics Finland (http://www.stat.fi/tup/tilastotietokannat/index_en.html). The age-specific incidence of surgery for SUI was calculated for the following age groups: 18–39, 40–49, 50–59, 60–69, 70–79, and 80 years or more. Age-standardized rates were calculated by using the Nordic Standard Population [15]. To estimate the risk of having had an operation for SUI by any given age, the cumulative incidence was calculated by adding age-specific incidences divided by the number of years at risk. Incidence rates in 1995, 2002, and 2009 and the mean incidence rate for the whole study period were used. The year 1995 was chosen for comparisons with previous data, 2002 for peak incidences, and 2009 for the most recent data.
The THL authorized the use of register data. The register authorities assessed the ethics of the study and as all data were anonymous, the study was exempted from evaluation by an Ethics Committee.
Analyses were performed using SAS JMP 9.0 for Mac and Microsoft Excel 2011 for Mac.
Results
A total of 38,500 women had surgery for SUI during the study period. 2,776 women (7.2 %) had one or more repeat operations after the first surgery during the study period. Only the primary operations are included in this analysis. 160 women (0.4 %) had multiple codes for SUI surgery for the same date and the data on these women were excluded. The total number of primary procedures for SUI was thus 38,340. Of all SUI procedures, the tension-free vaginal tape (TVT) and the transobturator slings (TOT, TVT-O) contributed with 23,635 procedures (61.6 %) followed by Burch colposuspension with 9,437 procedures (24.6 %). Other procedures had smaller numbers (Fig. 1).
From 1987 to 2002, the age-adjusted overall incidence of SUI surgery rose from 0.5 per 1,000 women to 1.3 per 1,000 women (Fig. 2). This increase was mainly due to the popularity of tension-free tape (TVT). By 2009, the incidence had dropped by 38 % to 0.8 per 1,000 women. Before 1999 SUI surgery was most often performed on women aged 50–59 years, followed by women aged 40–49 years (Fig. 2). An explicit increase in the incidence rate of SUI surgery was seen within the older age groups, as the rate for women aged 60–69 years rose almost six-fold from 0.5 per 1,000 in 1987 to 2.9 per 1,000 in 2002. Also, a nearly ten-fold increase from 0.2 to 1.9 per 1,000 women in the age group of 70–79 years was seen.
Stress urinary incontinence surgery for women above the age of 80 years was rare before the introduction of the TVT, but from 2002 to 2009 the rate in this age group has remained quite stable at 0.5 per 1,000 women. Surgery to treat SUI for women aged 18–39 years was uncommon and remained at the level of 0.1 per 1,000 women throughout the study period.
We estimated the risk for a woman to have undergone SUI surgery by a certain age and the lifelong risk. The lifelong risk for SUI surgery at the operation rates in 1995 was 3.6 % and in 2002 no less than 9.9 %. Thus, every tenth woman will undergo surgery for stress urinary incontinence (Fig. 3). Since the operation rate decreased notably during the last 7 years of our study period, the lifelong risk of SUI surgery calculated on the basis of the figures from 2009 was one third lower, or 6.3 %.
Discussion
This study shows a drastic increase in the number of surgical procedures for SUI from 1987 to 2002 and then a clear decline from 2002 to 2009. After the introduction of TVT, there may have been certain enthusiasm among gynecologists to offer less invasive and efficient methods to a large number of patients, which was more subdued during the later years of our study.
The number of procedures and the per capita rate more than doubled from 1987 to 2002. This phenomenon has been observed worldwide as well. In the USA, the rate of inpatient SUI surgery increased from 0.32/1,000 women in 1979 to 0.60/1,000 women in 1997 [16]. More recent figures from the USA show an increased rate, from 0.4/1,000 women in 1998 to the highest rate of 1.1/1,000 in 2002, after which a decline to 0.8/1,000 in 2007 took place [17]. In Belgium, the rate of anti-incontinence surgery per 1,000 women increased from 0.54 in 1997 to 2.03 in 2004 and has remained stable ever since [10]. Overall, the Finnish trend parallels the trend in Central Europe. In Australia, the rate of SUI surgery among Medicare beneficiaries treated in private hospitals rose from 4.2/1,000 in 1994 to 6.2/1,000 women in 2009, with a peak incidence rate in 2002, after which rates have remained quite stable [12]. The reason for the substantially higher incidence rates may be that only insured patients treated in private hospitals were included.
Tension-free vaginal tape was introduced in 1995 and soon it became available commercially [18]. The TVT has changed the way in which women with SUI are treated. It also explains the substantial increase in SUI operations worldwide. The rapid increase in the number of SUI surgeries in Finland (Fig. 1) is solely attributable to TVT; at the same time, Burch colposuspension has become a rarity. The transition from colposuspension to mid-urethral slings also occurred in Belgium [10], where TVT accounted for 88 % of SUI procedures in 2007. In Australia, 85.5 % of SUI surgeries in 2009 were mid-urethral slings. The USA also reports a notable increase in the rates of “other repair of stress urinary incontinence” [9, 11, 17, 19]. The ICD-9-based surgical procedure coding system used in these studies does not separate mid-urethral slings from other procedures, but the authors speculate that procedures coded as “other” were, in fact, mid-urethral slings [17]. The next stage in mid-urethral slings was the transobturator technique (TOT, outside-in and TVT-O, inside-out), which was introduced in an effort to reduce the risk of bladder and vessel injuries [18]. In 2007, transobturator slings surpassed TVT in popularity in Finland and accounted for two thirds of all SUI procedures in 2009.
From the perspective of patient age, anti-incontinence surgery was most frequent in 1987 to 1997 in the age group 40–59 years. With the rise in popularity of the TVT, the rate of surgical repair of SUI increased in elderly women and since 1999, the age-specific incidence of SUI surgery has been highest in the age group 60–69 years, with a substantial rise in the older age groups. The same trend toward the treatment of older women with SUI with surgery has also been reported from Australia, where the rate per capita among women over 55 years rose from 1994 to 2009 with 87 % and among women over 75 years with 206 % [12]. In the United States, a more subtle increase was reported in 1979–2004: the rate of surgical treatment of SUI among women over the age of 52 years increased from 0.64/1,000 to 1.60/1,000 [19]. In Belgium, on the other hand, an increase in older age groups did not take place [10]. We assume that the less invasive nature of mid-urethral sling procedures is the primary reason for the shift toward treating older women surgically. Also, as this effective means of treating stress urinary incontinence became acknowledged among patients, more women who had probably suffered from SUI symptoms for years sought help.
The lifelong risk for a woman to have undergone at least one surgery for urinary incontinence and pelvic organ prolapse before the age of 80 is reported to be 11.1 % [8]. We wanted to test this widely cited number in the Finnish target population and calculated the cumulative incidences for SUI surgery by age 49, 59, 69, and 79 years, and lifelong, i.e., up to 95 years, which was the oldest age at which SUI surgery was performed. The incidence rates of 2002 were used to calculate the lifelong risk for a Finnish woman of having an operation for SUI and arrived at 9.9 %. As the number of operations and the incidence rates have declined notably since 2002, a 9.9 % lifelong risk would currently be an exaggeration. A more accurate figure is derived from using the incidence rates of 2009, which yields a lifelong risk of SUI surgery of 6.3 %.
The strengths of this study are based on the proven quality and high coverage of nationwide, compulsory health care registries in Finland. Although most SUI surgery is performed in public hospitals, private hospitals are also obliged to report all their surgical procedures to the Care Registry for Health Care. Thus, all SUI surgeries performed in Finland were included in our study, and this included women of all ages treated in public and private hospitals, regardless of insurance status.
A weakness of this study is the risk of coding errors. There was a major change in the coding system of operations at the beginning of 1997, which coincided with the surge of TVT. There is a high risk that coding errors did take place, as it always takes time for clinicians to adapt to new codes and more refined coding options. We looked exclusively at anti-incontinence surgery. Patients who had other surgery as the primary procedure and whose SUI surgery was coded as the second or third procedure were included, but patients who may have had an SUI diagnosis and underwent surgery for prolapse, e.g., anterior colporrhaphy, without anti-incontinence surgery, were excluded, because we did not analyze the prevalence or type of concomitant surgical procedures.
This study shows how the surgical treatment of SUI has evolved in Finland over 22 years. A shift from Burch colposuspension to less invasive mid-urethral slings has taken place, and there has been a tendency toward treating older patients surgically. This study does not address the question of outcomes and quality of life changes and it is critically important to further analyze the rates and types of reoperations for recurrent SUI in the aftermath of the profound changes in the treatment of SUI that have taken place.
Abbreviations
- SUI:
-
Stress urinary incontinence
- TVT:
-
Tension-free transvaginal tape (TVT is used for all suprapubic mid-urethral sling procedures as it is in the Finnish coding system)
- TOT:
-
Transobturator tension-free vaginal tape outside-in
- TVT-O:
-
Transobturator tension-free vaginal tape inside-out
References
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, Monga A, Petri E, Rizk DE, Sand PK, Schaer GN (2010) An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J 21:5–26
Mäkinen JI, Gronroos M, Kiilholma PJA, Tenho TT, Pirhonen JP, Erkkola RU (1992) The prevalence of urinary incontinence in a randomized population of 5247 adult Finnish women. Int Urogynecol J 3:110–113
Coyne KS, Kvasz M, Ireland AM, Milsom I, Kopp ZS, Chapple CR (2012) Urinary incontinence and its relationship to mental health and health-related quality of life in men and women in Sweden, the United Kingdom, and the United States. Eur Urol 61:88–95
Buckley BS, Lapitan MCM (2010) Prevalence of urinary incontinence in men, women, and children--current evidence: findings of the Fourth International Consultation on Incontinence. Urology 76:265–270
Riss P, Kargl J (2011) Quality of life and urinary incontinence in women. Maturitas 68:137–142
Tennstedt SL, Fitzgerald MP, Nager CW, Xu Y, Zimmern P, Kraus S, Goode PS, Kusek JW, Borello-France D, Mallett V (2007) Quality of life in women with stress urinary incontinence. Int Urogynecol J 18:543–549
Subak LL, Brubaker L, Chai TC, Creasman JM, Diokno AC, Goode PS, Kraus SR, Kusek JW, Leng WW, Lukacz ES, Norton P, Tennstedt S (2008) High costs of urinary incontinence among women electing surgery to treat stress incontinence. Obstet Gynecol 111:899–907
Olsen A, Smith V, Bergstrom J, Colling J, Clark A (1997) Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol 89:501–506
Anger JT, Weinberg AE, Albo ME, Smith AL, Kim J-H, Rodríguez LV, Saigal CS (2009) Trends in surgical management of stress urinary incontinence among female Medicare beneficiaries. Urology 74:283–287
Cammu H, Saeys F, Haentjens P (2010) Dramatic increase (1997-2007) in the number of procedures for stress urinary incontinence in Belgium. Int Urogynecol J 21:1511–1515
Jonsson Funk M, Levin PJ, Wu JM (2012) Trends in the surgical management of stress urinary incontinence. Obstet Gynecol 119:845–851
Lee J, Dwyer PL (2010) Age-related trends in female stress urinary incontinence surgery in Australia - Medicare data for 1994-2009. Aust N Z J Obstet Gynaecol 50:543–549
Rogo-Gupta L, Litwin MS, Saigal CS, Anger JT (2013) Trends in the surgical management of stress urinary incontinence among female Medicare beneficiaries, 2002–2007. Urology 82:38–41
Wu JM, Matthews C a, Conover MM, Pate V, Jonsson Funk M (2014) Lifetime risk of stress urinary incontinence or pelvic organ prolapse surgery. Obstet Gynecol 123:1201–1206
Nordic Medico-Statistical Committee (NOMESCO) (2006) Health statistics in the nordic countries 2006. Available from: http://nowbase.org/∼/media/Projekt%20sites/Nowbase/Publikationer/Helse/Helse%202006.ashx
Boyles S, Weber A, Meyn L (2003) Procedures for urinary incontinence in the United States, 1979–1997. Am J Obstet Gynecol 189:70–75
Wu JM, Gandhi MP, Shah AD, Shah JY, Fulton RG, Weidner AC (2011) Trends in inpatient urinary incontinence surgery in the USA, 1998–2007. Int Urogynecol J 22:1437–1443
Rapp DE, Kobashi KC (2008) The evolution of midurethral slings. Nat Clin Pract Urol 5:194–201
Oliphant SS, Wang L, Bunker CH, Lowder JL (2009) Trends in stress urinary incontinence inpatient procedures in the United States, 1979–2004. Am J Obstet Gynecol 200:521.e1–521.e6
Acknowledgements
Funding
This study was supported by grants from The National Graduate School of Clinical Investigation and State-granted, university-level health research funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Financial disclaimer
None.
Rights and permissions
About this article
Cite this article
Kurkijärvi, K., Aaltonen, R., Gissler, M. et al. Surgery for stress urinary incontinence in Finland 1987–2009. Int Urogynecol J 27, 1021–1027 (2016). https://doi.org/10.1007/s00192-015-2926-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-015-2926-z