Abstract
Introduction and hypothesis
Although there is clear consensus on the use of monofilament polypropylene tapes for treating stress urinary incontinence (SUI), tapes differ in weight, stiffness, and elasticity. In this study, we compared outcomes of two tape types: high-stiffness Intramesh SOFT L.I.F.T versus low-stiffness Intramesh L.I.F.T. tape. Our null hypothesis was that in terms of performance, SOFT tape equaled L.I.F.T. tape.
Methods
Six hundred and sixty women underwent prospective transvaginal tape (TVT) surgery for SUI: 210 had the SOFT tape placed and 450 the L.I.F.T. tape. Follow-ups were scheduled at 3 and 12 months.
Results
Objective cure at 3-months’ follow-up was 87 % in the SOFT group vs 94 % in the L.I.F.T. group (p = 0.003) and at 12 months 86 vs 96 % (p = 0.0004), respectively. Subjective outcomes were equal. For SOFT tape, the objective failure rate at 3 months was especially pronounced in women older than 70 years: 31 vs 10 % (p = 0.008), and subjective failure was 24 vs 7 % (p = 0.01). At 12 months, objective failure for the SOFT tape was significantly higher in both age groups compared with L.I.F.T. [odds ratio (OR) 2.17]. Multivariate analysis showed that body mass index (BMI) ≥30 (OR 2.41), mixed incontinence (MUI) (OR 2.24), use of SOFT tape (OR 2.17), and age ≥ 70 years are significant independent risk factors for surgical failure.
Conclusions
Outcomes with SOFT tape are significantly inferior than with L.I.F.T. tape, especially among elderly women. Therefore, the two variants of monofilament polypropylene tape are not interchangeable.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Retropubic tension-free midurethral tape surgery was introduced in the mid-1990s and has become a globally established procedure for managing female stress urinary incontinence (SUI). Tension-free vaginal tape (TVT), being the most notable, has become the gold standard due to its high rate of success, low rate of complications, and short surgeon learning curve. Mesh materials used to date have been of different types and designs, and the consensus of evidence is that the least morbidity will be achieved by using a lightweight, large-pore, monofilament polypropylene type 1 mesh [1]. Following the success of TVT, a variety of polypropylene tapes have been released onto the market without proper evaluation. Each brand uses a unique tape formulation, and there is no evidence to support one in favor of another. However, mesh weight and composition are well-known important factors for healing and complications, as the extent of chronic inflammation is related to the amount of foreign material left in the body. Differences in mechanical properties, such as stiffness and elasticity, have been examined in the laboratory but not in vivo [2, 3]; the impact on the body and clinical outcomes after surgical treatment for SUI is almost unknown, but material stiffness has been associated with the risk of erosion [2, 3]. During the initial postoperative days, the implant is held in place by friction acting on the tape passing through the tissue [4]. The impact of the tape’s mechanical and physical properties on friction force in the early and vulnerable phase of healing has not been studied in humans to date.
The idea for this study arose from observations that: (1) friction force of a new, high-stiffness version of a basic low-stiffness tape was lower; (2) informal reviews of outcome data predict a lower cure rate in women fitted with the newer, high-stiffness tape. The aim of the study was to compare the performance of two monofilament polypropylene tapes from the same manufacturer: a light-weight and high-stiffness (inelastic) Intramesh SOFT tape with smooth edges, and a heavyweight and low-stiffness Intramesh L.I.F.T. tape with rough edges. The null hypothesis was that in terms of performance, SOFT tape equals L.I.F.T. tape.
Materials and methods
From May 2005 to September 2012, a single-center prospective cohort study was conducted in our outpatient clinic. Six hundred and sixty women with urodynamic SUI were enrolled consecutively and underwent retropubic tension-free midurethral tape (TVT) surgery as their sole procedure. Of these, 450 had the L.I.F.T. tape placed and 210 the SOFT tape. The latter tape was introduced in October 2006 and used until March 2010. Both tapes are type I, polypropylene, monofilament, macroporous TVT tapes manufactured by Cousin Biotec. They are available as a basic L.I.F.T. tape with low stiffness and 100 g/m2; and a newer, lighter-weight variant, SOFT tape, with high-stiffness and 60 g/m2. Another striking difference is the surface property is that L.I.F.T. tape has rough edges and SOFT tape has smooth edges; the latter is characterized as an inelastic (high-stiffness) tape with nonaggressive edges. Dimensions of both tapes are 1 cm × 45 cm.
All patients underwent a standardized preoperative evaluation: a 2-day bladder diary, postvoid residual urine (PVR) measured by a catheter, filling cystometry, and pressure-flow study in the seated position. An ultrashort pad-test with the patient in a standing position was performed; while the patient performed ten vigorous coughs, the amount of urine loss was quantified by measuring the increase in pad weight [5]. The ultrashort pad test was performed with 300 ml saline in the bladder, which was filled in conjunction with catheterization for PVR measurement. Lastly, a free uroflowmetry at voided volume ≥150 ml was performed. The voiding function was assessed by maximum flow rate (Qmax), corrected Qmax (Qmax/√voided volume), average flow rate (Qave), flow time, time to maximum flow and voided volume. Methods, definitions, and units conform to the standards jointly recommended by the International Continence Society (ICS) and the International Urogynecological Association (IUGA) [6]. All patients had anterior vaginal wall prolapse < stage 2 [Pelvic Organ Prolapse Quantification system (POP-Q)], and no concomitant prolapse surgery was done [7]. All postmenopausal women were treated at least 1 month before surgery with, mainly, locally applied estrogens.
The TVT operation was performed under local anesthesia. A full-thickness midline incision was placed under the midurethra, and the tape was placed so it touched the urethra and then adjusted until the leaking stopped while the patient coughed vigorously at a bladder volume of 300 ml, whereupon cystoscopy was performed. The midline incision was closed with absorbable stitches and the Foley catheter removed. All patients received prophylactic cefuroxime 1.5 g intravenously during surgery. The majority of patients (92 %) were discharged from hospital a few hours after the procedure.
Follow-up
Follow-up visits were scheduled at 3 and 12 months after surgery. Both visits involved PVR, standardized cough stress test performed with a bladder volume of 300 ml saline in the supine position, and a short-term pad test in the standing position. Last, a free uroflowmetry at voided volume ≥150 ml was performed.
Definition of outcomes
To evaluate the effect of treatment, both subjective (patients’ perception of clinical improvement expressed in an open interview) and objective definition criteria were applied, as follows:
-
Subjective cure: if the reported incontinence episodes were ≤1 per week (a reduction in incontinence episodes >90 %) and the patient was satisfied
-
Subjective improvement: if there was a reported reduction in incontinence episodes ≥75 % and the patient was satisfied
-
Subjective failure: if the outcomes were any less positive than the above
-
Objective cure: if the ultrashort pad test was negative (pad weight increase <1 g)
-
Objective failure: if the ultrashort pad test was positive (pad weight increase ≥1 g)
-
Vaginal exposure was defined as tape exposure within the vagina at the suture line after vaginal incision had healed
The study was registered with the Danish Data Protection Agency. Ethical approval was not required.
Statistical analysis
Data were analyzed using statistical package R [8]. For univariate data, testing of significance was performed by applying chi-square, Fisher’s exact, or Wilcoxon two-sample tests, as indicated. Logistic regression modeling was performed to search for significant associations (R-command “glm”). The model was reduced using automated stepwise removal of variables (R-command “step”) to find the best model fit using the Akaike information criterion (AIC). Power calculation for two proportions with different sample sizes were performed with the command pwr.2p2n.test from the pwr package. Significance levels were set at p = 0.05 or 95 % confidence intervals (CI).
Results
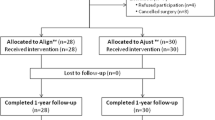
Six hundred and sixty women were enrolled consecutively, with 210 in the SOFT group and 450 in the L.I.F.T. group. At baseline, patient characteristics (Table 1), bladder diary and cystometry (Table 2), and bladder function (Table 3) were similar between groups, except for a higher ratio of mixed urinary incontinence (MUI) and a lower maximum cystometric capacity in the SOFT group. At 12-months’ follow-up, 83 % in the SOFT group and 74 % in the L.I.F.T. group were examined and evaluated according to the protocol. At 12 months, 133 (20 %) 645 patients were lost to follow-up, and the proportion of patients >70 years was nearly unchanged: 19.5 % at 3 months and 22.5 % at 12 months (Table 4).
Power calculation
A difference of 5–10 % in subjective or objective cure was considered clinically important. Given the number of cases available at 3- and 12-months’ follow-up, a difference of 6 and 7 % is detectable with a power of ∼80 %. A difference of 10 % may be detected with a power >97 % at both follow-up times. At a 5 % difference, power falls sharply toward 50 %; thus, a difference of 10 % in any variable analyzed would not be missed
Objective outcome
Objective cure was significantly lower in the SOFT group at both 3- and 12-months’ follow-up (Table 4). Failure rate at 3 months was especially pronounced in women >70 years: 31 % in the SOFT group vs 10 % in the L.I.F.T. group (p = 0.008). Similarly, at 12-months’ follow-up, we found a significantly higher failure rate in the SOFT group; however, this time it was among women both older and younger than 70 years: 21 and 12 %, respectively. In the L.I.F.T. group, failure rates among women > 70 and < 70 was 5 and 4 %, respectively (Table 4).
Logistic regression of basic variables as significant predictors of objective failure of surgery shows that the most independent risk factors are age >70 years, body mass index (BMI) >30, mixed UI, and the use of SOFT tape (Table 5).
Subjective outcome
At 3-months’ follow-up, failure was reported by 24 % of the elderly in the SOFT group vs 7 % in the L.I.F.T. group (p = 0.01). Otherwise, 89 % of all patients in the SOFT group and 93 % in the L.I.F.T. group reported cure or improvement and this difference was not significant (Table 4).
Logistic regression of basic variables as significant predictors of no subjective improvement/cure shows that the most independent risk factors for subjective failure are mixed UI, BMI body mass index >30 and micturition frequency (Table 5).
Changes in bladder function
There was a considerable change in voiding function after surgery in terms of free Qmax, average Qmax, flow and voiding time, and PVR (Table 3). The reduction in free Qmax and average Qmax was significantly lower in the SOFT group at both 3- and 12-months’ follow-up. Flow and voiding time were significantly lower for the SOFT group at 3 months, as was PVR; differences at 12 months were not significant. Ultrashort pad test at 3- and 12-months’ follow-up showed significantly higher urine loss in the SOFT group. We saw no healing defects or vaginal exposure.
Discussion
The hypothesis that cure rates of a newer high-stiffness and smooth SOFT tape and a basic low-stiffness and rough L.I.F.T. That tapes are equal in efficacy was disproven. Women >70 years treated with the smooth-(SOFT) tape experienced a significantly higher failure rate: objective failure rate was 31 vs 10 % and subjective failure rate 24 vs 7 %. Logistic regression analyses of basic variables showed that risk factors for surgical failure included mixed UI, age >70 years, high BMI and the use of SOFT tape.
The three main differences between the tapes used in this study are: (1) stiffness (resistance to deformation), (2) elasticity (ability to return to initial size and shape after being deformed), and (3) outer structure of the tapes. The lightweight SOFT tape has a high-stiffness, high elasticity, and smooth edges; whereas the heavyweight L.I.F.T. tape has a low-stiffness and low elasticity (deformation is the result of being deformed) and rough edges.
How the TVT-band is kept in place during the initial postoperative period depends on three main variables: (1) the outer structure of the tape, (2) the type of tissue the tape passes through and (3) the strength of that tissue [4].
We found that the SOFT tape was not as effective as the L.I.F.T. tape. One plausible explanation for the poorer result may be attributed to the outer structure of the tape: that is, its smooth edges, which may impair tape fixation in the very early phase of the healing process before tissue incorporation takes place, thus the tape slips. The theory that SOFT tape cannot hold its position explains the lower subjective and objective cure rates seen in elderly women especially, where the combination of low friction force due to smooth edges and fragile tissue is present. This theory is in accordance with the study by Lei et al. [9], which found that the stiffness of vaginal tissue was higher in postmenopausal compared with premenopausal women and the maximum fracture was significantly lower; thus, tissue is more fragile in the elderly. Furthermore, this theory may account for the postoperative observation that SOFT tape obstructs bladder function less than does L.I.F.T. tape. The poorer cure rate and lesser obstructive effect of the SOFT tape may have one more explanation: its high stiffness. This may be advantageous because, unlike low-stiffness tape that deforms under strain, high-stiffness tape allows individualized tensioning without tape deformation; thus, the surgeon may be able to place the tape more precisely and thereby avoid adverse postoperative events, such as voiding dysfunction and postvoid residual. Our results are similar to those of Prien-Larsen et al. [10], who compared high-stiffness and smooth intravaginal slingplasty (IVS) tape with low-stiffness and rough TVT tape and found a poorer cure rate and lesser obstructive effect of the high-stiffness and smooth IVS tape. Rechenberger et al. [11] found a lower cure rate in the IVS compared with the TVT group (80 vs 88 %), but the difference was not significant—probably due to small sample size. Furthermore, they reported a lesser obstructive effect of high-stiffness and smooth IVS tape and attributed this to high-stiffness tape permitting precise positioning. Jijon et al. [12], who used an inelastic (high-stiffness) polypropylene tape comparable with our high-stiffness SOFT tape, found, as we did, an improvement/cure rate of 87 % and a failure rate of 13 %. None of these studies took into consideration the impact of the smooth edges as an explanation for the poorer outcomes and lesser obstructive effects.
In our multivariate analysis, we found that patient age affected objective but not subjective cure rate, and this is supported by results from a large-scale study by Stav et al. [13]. Contrary to our finding in another large study, Hellberg et al. [14] found a sharp decrease in subjective cure rate among women over the age of 75 years; Bohlin et al. [15] also found lower subjective cure rates in women >80.
Logistic regression analyses revealed three risk factors for subjective failure of surgery: mixed- I, BMI >30, and micturition frequency. Furthermore, we found four risk factors for objective failure, of which three were present in both SOFT and the L.I.F.T. groups: BMI and age in equal proportions in both groups and M-UI in a greater proportion in the SOFT group. The fourth risk factor, the use of SOFT tape, was only present in the SOFT group. It is a fact that the groups were slightly differently regarding mixed UI, the SOFT group with the worst results, included more patients with mixed UI (MUI). It is well known that cure rates are lower among patients with MUI [16], and this fact could be responsible for the poor result in the SOFT group. Because logistic regression analyses showed that contribution of the two risk factors MUI and the use of SOFT tape are nearly equal, it is unlikely that only MUI is responsible for the poor results; therefor, SOFT tape also contriutes to objective failure of surgery in the SOFT group.
Like us, Stav et al. [13] found, in a retrospective large-scale study, that MUI and BMI >25 were significant independent risk factors for subjective failure of surgery and that age was not a risk factor. Furthermore, they showed that tape type was not a risk factor. Also, Paick et al., in a prospective study [17], that MUI was a risk factor for failure; they also found that transobturator tape procedure was a risk factor. Recently, Gleason et al. [18] showed in a retrospective study of 534 patients with MUI that the cure rate was significantly lower—64 vs 85 % in pure SUI—and that MUI was a risk factor on multivariate analyses.
Other studies were not able to reveal any independent risk factors, perhaps because these studies were too small [19, 20]. In a recent study by Weltz et al. [21] in which they pooled data from 13 studies, of which the majority were retrospective and highly inhomogeneous, they found lower but comparable cure rates in obese and nonobese women. Our finding, that BMI is a risk factor for surgical failure, accords with the results of Lopes et al. [22], which found that BMI > 25 was associated with higher tissue stiffness and thus more fragile tissue; also, Bohlin et al. [15], in a large-scale study, that women with BMI >30 experienced lower cure rates. Furthermore, it is well known from the study by Noblett et al. that there is a strong association between intraabdominal pressure and BMI [23].
Tape weight and composition are important and well-known factors affecting healing and complications, whereas the optimal biomechanical properties, such as stiffness, elasticity, and structure of tape edges, are unknown [24]. We found that both stiffness and the property of tape edges might have any impact on outcomes; however, what we cannot determine is the relationship between the impacts of the two parameters. We therefore urgently need clarification of these issues. First, studies are needed to correlate stiffness, elasticity, and friction forces with clinical outcomes and impact on bladder function; then, we need proper evaluation of a given tape and information on how differences in biomechanical properties affect the body and thus clinical outcomes before that tape is launched onto the market.
The strength of this study is that, to the best of our knowledge, it is the first comparative study that seeks to describe the impact of tape properties on outcomes of SUI surgery; 20 % of cases were lost to follow-up at 12 months. This loss is considered quite small; age distribution remained unchanged and should not affect the outcome analysis at 12 months. Furthermore, it is prospective and includes a standardized preoperative and postoperative clinical evaluation of both bladder function and subjective and objective cure rates as outcome metrics; also, it includes a large number of patients in each group. Finally, all operations were performed under local anesthesia, and no concomitant prolapse surgery was done. A limitation of the study is that it is not randomized, but the large number of patients counteracts this necessity.
Conclusion
This study shows that tape properties should be taken into consideration before new tapes are launched onto the market and before their adoption for use; different polypropylene tapes have different properties and may therefore have different impacts on outcome metrics. Different tape types are not interchangeable.
Abbreviations
- Stiffness:
-
Resistance to deformation
- Elasticity:
-
Ability to return to initial size and shape after being deformed (reversible)
References
Deprest J, Zheng F, Konstantinovic M et al (2006) The biology behind fascial defects and the use of implants in pelvic organ prolapse repair. Int Urogynecol J 17:S16–S25
Moalli PA, Papas N, Menefee S, Albo M, Meyn L, Abramowitch SD (2008) Tensile properties of five commonly used mid-urethral slings relative to the TVTTM. Int Urogynecol J 19:655–663
Mangera A, Bullock AJ, Chapple CR, MacNeil S (2012) Are biochemical properties predictive of the success of prostheses used in stress urinary incontinence and pelvic organ prolapse? A systematic review. Neurourol Urodyn 31:13–21
Alcalay M, Livneh M, Braun NM, Tov YS, Hod E (2014) Mesh pullout force: comparative study of different deployment techniques in a sheep model. Int Urogynecol J 25:103–107
Persson J, Bergqvist CE, Wølner-Hanssen P (2001) An ultra-short perineal pad-test for evaluation of female stress urinary incontinence treatment. Neurourol Urodyn 20:277–285
Haylen BT, Ridder DD, Freeman RM et al (2010) An international urogynecological association (IUGA)/international continence society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn 29:4–20
Bump RC et al (1996) The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol 175:10–17
R Core Team (2015) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL http://www.r-project.org/
Lei L, Song Y, Chen R (2007) Biomechanical properties of prolapsed vaginal tissue in pre- and postmenopausal women. Int Urogynecol J 18:603–607
Prien-Larsen JC, Hemmingsen L (2009) Long-term outcomes of TVT and IVS operations for treatment of female stress urinary incontinence: monofilament vs. multifilament polypropylene tape. Int Urogynecol J 20:703–709
Rechberger T, Rzezniczuk K, Skorupski P, Adamiak A, Tomaszewski J, Baranowski W, Jakowicki JA (2003) A randomized comparison between monofilament and multifilament tapes for stress incontinence surgery. Int Urogynecol J 14:432–43
Jijon A, Hegde A, Arias B, Aguilar V, Davila GW (2013) An inelastic retropubic suburethral sling in women with intrinsic sphincter deficiency. Int Urogynecol J 24:1325–1330
Stav K, Dwyer PL, Rosamilia A, Schierlitz L, Lim YN, Lee J (2010) Risk factors of treatment failure of midurethral sling procedures for women with urinary stress incontinence. Int Urogynecol J 21:149–155
Hellberg D, Holmgren C, Lanner L, Nilsson S (2007) The very obese woman and the very old woman: tension-free vaginal tape for the treatment of stress urinary incontinence. Int Urogynecol J 18:423–429
Bohlin KS, Ankerdal M, Pedroletti C, Lindkvist H, Milsom I (2015) The influence of the modifiable life-style factors body mass index and smoking on the outcome of mid-urethral sling procedures for female urinary incontinence. Int Urogynecol J 26:343–351
Kulseng-Hanssen S, Husby H, Schiøtz HA (2008) Follow-up of TVT operations in 1113 women with mixed urinary incontinence at 7 and 38 months. Int Urogynecol J 19:391–396
Paick J-S, Cho MC, Oh S-J, Kim SW, Ku JH (2007) Factors influencing the outcomes of mid urethral sling procedures for female urinary incontinence. J Urol 178:985–989
Gleason JL, Parden AM, Jauk V, Balllard A, Sung V, Richter HE (2015) Outcomes of midurethral sling procedures in women with mixed urinary incontinence. Int Urogynecol J 26:715–720
Paick JS, Oh SJ, Kim SW, Ku JK (2008) Tension-free vaginal tape, suprapubic arc sling, and transobturator tape in the treatment of mixed urinary incontinence in women. Int Urogynecol J 19:123–129
Rechberger T, Futyma K, Jankiewicz K, Adamiak A, Bogusiewicz M, Skorupski P (2010) Body mass index does not influence the outcome of anti-incontinence surgery among women whereas menopausal status and ageing do: a randomized trial. Int Urogynecol J 21:801–806
Weltz V, Guldberg R, Lose G (2015) Efficacy and perioperative safety of synthetic mid-urethral slings in obese women with stress urinary incontinence. Int Urogynecol J 26:641–648
Lopez SO, Eberhart RC, Zimmern PE, Chuong CJ (2015) Influence of body mass index on the biomechanical properties of the human prolapsed anterior vaginal wall. Int Urogynecol J 26:519–525
Noblett KL, Jensen JK, Ostergard DR (1997) The relationship of body mass index to intra-abdominal pressure as measured by multichannel cystometry. Int Urogynecol J 8:323–326
Patel H, Ostergaard DR, Sternschuss G (2012) Polypropylene mesh and the host response. Int Urogynecol J 23:669–679
Acknowledgments
The authors acknowledge Margrethe Foss Hansen, MA, for her assistance with data collection and editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
RBD received honoraria outside this work. The remaining authors declare they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Prien-Larsen, J.C., Prien-Larsen, T., Cieslak, L. et al. Influence of TVT properties on outcomes of midurethral sling procedures: high-stiffness versus low-stiffness tape. Int Urogynecol J 27, 1039–1045 (2016). https://doi.org/10.1007/s00192-015-2921-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-015-2921-4