Abstract
Introduction and hypothesis
Preliminary reports show promising data on tension-free vaginal tape (TVT) in women with lower motor neuron lesion (LMNL) presenting with stress urinary incontinence (SUI). We compared efficacy and safety of TVT to pubovaginal sling (PVS) in treating SUI in women with LMNL.
Methods
This was a pilot, nonrandomized clinical trial evaluating women with SUI associated with pathology at or below S2 spinal segment. Failure was defined as leakage of urine during cough test at 250 ml bladder volume. Primary outcome was time to treatment failure based on positive cough stress test. Other outcomes were Urogenital Distress Inventory Short Form-6 (UDI-6), Incontinence Impact Questionnaire Short Form-7 (IIQ-7) and urodynamics. Regression models were used to adjust for confounders.
Results
The study evaluated 40 women: 20 TVT and 20 PVS, and cure rates were 80 and 85 %, respectively. Time to treatment failure in the TVT group was comparable with the PVS group, with an unadjusted hazard ratio (HR) of 2.90 [95 % confidence interval (CI), 0.61–15.42, P = 0.154]. After adjusting for confounders, adjusted HR for treatment failure was 1.04 (95 % CI, 0.12–8.66, likelihood ratio chi-square P = 0.973). Both groups showed significant reductions in UDI-6 and IIQ-7 scores after surgery. One patient had mesh erosion in the TVT group.
Conclusions
TVT is feasible, effective and safe for women with LMNL presenting with SUI, with comparable treatment outcomes to PVS. TVT might be of benefit to women who do not use clean intermittent catheterization (CIC) at baseline.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Stress urinary incontinence (SUI) is the involuntary leakage of urine associated with sudden increase in intra-abdominal pressure [1] and is a highly prevalent condition, with one study estimating the prevalence to be as high as 55 % in some communities; and this condition may seriously impair the quality of women’s lives [2]. Neurogenic and genuine SUI in women are different pathologies. Obstetric trauma is the most important established risk factor for genuine SUI. Common mechanisms proposed involve damage to the anatomic support of the pelvic floor. The endopelvic fascia forms a supportive suburethral hammock that compresses the urethra during stress [3]. In addition, the pubourethral ligament kinks the urethra during stress. Midurethral slings (MUS) were developed on the basis of these features [4].
Lower motor neuron lesions (LMNL) involve the conus medullaris (terminal end of the spinal cord), cauda equina (bundle of spinal nerve roots consisting of: L2–L5, S1–S5, coccygeal or peripheral nerves [5]. This classically occurs in sacral spinal cord injuries, lumber disc prolapse, myelodysplasia, after radical pelvic surgery, pelvic injury, sacral agenesis, and spinal cord tumors. Malfunction of the pudendal nerve in these patients, which innervates the external sphincter, will result in an open fixed bladder neck and prevent reflex contraction of the striated sphincteric fibers during stress, leading to SUI. Associated malfunction of pelvic nerves that innervate the detrusor muscle may lead to detrusor underactivity [6]. Classically, the urodynamic finding is SUI and hypotonic areflexic bladder without rise in intravesical pressure. Sometimes, there may be poor compliance. The sphincter is typically denervated, as documented on electromyelogram (EMG) [7].
Treatment of neurogenic SUI (nSUI) includes obstructing pubovaginal slings (PVS) [8], bulking agents [9], and artificial urinary sphincter [10]. Women with nSUI have been traditionally treated with PVS, with excellent continence resulting (85–90 %) and low complication rates [11]. These slings are put under tension with the intent to occlude the urethra, so subsequent clean intermittent catheterization (CIC) is the rule [12]. Bulking agents did not show satisfactory cure rates, especially among women using CIC [9]. The artificial urinary sphincter, though effective, is expensive and may be associated with significant complication and revision rates [13].
There are little data in the literature about the use of the minimally invasive MUS in women with nSUI. Two retrospective studies show mid- and long-term outcomes of tension-free vaginal tape (TVT) in women with nSUI, reporting continence rates of 83 % at 2 years [14] and 77 % at 10 years [15]. Preliminary data from these two studies provided promising information on the efficacy and safety of MUS in women with LMNL presenting with SUI; however, to date, no comparative data are published on the topic. To provide more information, we designed this clinical trial to compare the efficacy and safety of TVT compared with the standard rectus fascia PVS in treating SUI in women with LMNL.
Materials and methods
This clinical trial was approved by the Ethical Committee of the Faculty of Medicine, Asyut University. Women ≥18 years with SUI associated with spinal pathology at or below S2 (LMNL) who attended the Female Urology and NeuroUrology Outpatient Clinic, Asyut University Urology Hospital, were considered for participation. SUI must be demonstrated by physical examination and confirmed urodynamically. Women with spinal lesion above the sacral cord and those with higher stages of pelvic organ prolapse (POP) that required surgical intervention were excluded. Those already using CIC before the operation were asked to maintain CIC; those not using CIC at baseline were informed about the need to initiate CIC after the procedure. All participants provided their informed consent for participation and also have consent for surgery, including the need for CIC after surgery.
Baseline patient evaluation included history, pelvic examination, focused neurological exam, and urine analysis. Postvoid residual urine volume (PVR) was assessed using ultrasound. All patients performed a 24-h voiding diary. Women’s perception of their symptoms and the impact of incontinence on their quality of life (QoL) were assessed by two questionnaires before the operation: the Urogenital Distress Inventory-6 (UDI-6), and the Incontinence Impact Questionnaire-7 (IIQ-7) [16]. All patients underwent dual-channel subtracted filling cystometry as well as pressure-flow studies with EMG, both before and after surgery. Urodynamics was done according to the recommendations of Good Urodynamic Practice [17]. Cystometry was performed using sterile water at 50 ml/min. Valsalva leak-point pressure (LPP) was assessed beginning with bladder volume of 100 ml, with the patient in the semisitting position, and increasing in increments of 50 ml to maximum capacity, unless leakage was already seen at lower volumes. Estimation of outlet resistance was performed using the abdominal LPP (ALPP) and EMG (for sphincter denervation). Methods, definitions, and units conformed to the standards jointly recommended by the International Urogynecological Association (IUA) and the International Continence Society (ICS), except where specifically noted [1].
In this nonrandomized trial, the decision to perform TVT or PVS was dependent on the preference of the patient and surgeon. We report the outcome in patients with a minimum 12-month follow-up, since we believe that most early failures and urodynamic outcomes manifest by that time. The operative technique of PVS has been previously described [18]. The aim was to insert the sling under tension to occlude the urethra. TVT was performed in accordance with the standard technique of TVT under spinal anesthesia. A Foley catheter was fixed for 24 h, and patients were asked to void spontaneously.
The primary outcome was an objective failure rate based on the finding of standardized cough stress test during physical examination. Failure of treatment was defined as any leakage of urine during cough and Valsalva maneuvers at a bladder volume of 250 ml. This test was repeated on each follow-up visit. Time to failure was the endpoint for that outcome. The procedure was considered as failed if the patient leaked urine on examination. Secondary outcomes were UDI-6 and IIQ-7 before and 12 months after the procedure. Proportion of women with voiding dysfunction (PVR > 150 ml), amount of PVR, and other related urodynamic variables were compared between the two groups. Finally, complications including mesh erosion, infection, pain, and reoperation in relation to treatment failure or to treat complications were recorded.
Statistical analysis
Continuous variables are presented as mean and standard deviation (SD) or median and range according to their distribution. Categorical variables are presented as count and percent. Independent t test was used to compare continuous variables with normal distribution between groups, while paired t test was used to compare changes from baseline in the same group. Wilcoxon rank-sum test was used to compare independent continuous variables with skewed distribution; Wilcoxon signed-rank test was used to compare dependent continuous variables with skewed distribution; chi-square tests and Fisher’s exact test were used to compare categorical variables. The primary outcome of the study was objective treatment failure based on diagnosis of leakage on a standard cough stress test. Time to failure was the endpoint for that outcome, and Kaplan–Meier curves were used to calculate the cumulative failure rate in each group. Proportional hazard regression models were used to evaluate the associations with treatment failure and adjust for possible confounders. A total sample of 40 patients (20 in each group) provides a power of 80 % to detect a difference in failure rate of 15 %, assuming a possible failure rate of 10 % in the control group from previous literature [11]. Significance was considered when P < 0.05, and we used JMP 10.0 software (SAS Inc, Carey NC, USA).
Results
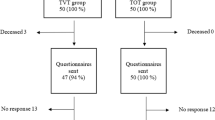
From June 2007 to November 2013, a total of 52 women with LMNL presenting with SUI met the inclusion criteria and were invited to participate in the study. Twelve patients refused to consent because of the possibility of postoperative CIC and were thus excluded. Therefore, 40 women were evaluated: 20 had TVT and 20 had PVS. The etiology of nSUI in the TVT group was sacral spinal cord injury in 16 women, myelomeningocele in three, and spinal cord tumor in one. Etiology in the PVS group was sacral spinal cord injury in 14, myelomeningocele in four, and lumber disc surgery in two. All patients had no previous incontinence or bladder surgeries.
At baseline, women in the TVT group had a higher parity and reported worse incontinence-related QoL reflected as higher total scores on the IIQ. Women in the TVT group had lower median PVR (27.5 vs 150 ml, Wilcoxon rank-sum test P = 0.039), fewer with PVR <150 (20 % vs. 55 %, χ2 test P = 0.022), and fewer with baseline CIC (25 % vs 55 %, χ 2 test P = 0.053).;ALPP was lower in the TVT group. Other baseline characteristics were comparable between groups (Table 1.).
For our primary outcome, objective failure at the last follow up, seven of 40 (17.5 %) women had a positive 250-cc standardized cough stress test and were considered treatment failures: four (20 %) in the TVT group and three (15 %) in PVS group. Time to treatment failure in the TVT group was comparable with the PVS group with an unadjusted hazard ratio (HR) of 2.90 [95% confidence interval (CI) 0.61–15.42, long-rank test P value = 0.154) (Fig. 1). At 2 year, the cumulative objective failure rate was 5.9 % in the TVT group compared with 0 % in the PVS group. At 4 years, the cumulative failure rate was 41.8 % in the TVT group compared with 25.4 % in the PVS group. After adjusting for baseline characteristics that were significantly different at baseline, including parity, preoperative total score on the modified IIQ-7, preoperative PVR >150, and preoperative CIC, adjusted HR for treatment failure was 1.04 [95% CI, 0.12, 8.66, likelihood ratio (LR) chi-square P = 0.973}.
In both groups, there were significant reductions in UDI-6 and IIQ-7 total scores (Fig. 2). In the UDI subitem of frequency, the reduced score was significantly greater in the PVS group (Wilcoxon rank-sum test, P = 0.026). Reduction in the total modified IIQ-7 score was significantly greater in the TVT group (Wilcoxon rank-sum test, P = 0.012), which can be explained by higher baseline total modified IIQ-7 scores in the TVT group. This significantly greater improvement in the TVT group was also noted in the subitem scores for Prayer, Travel, Social Activities, and Emotional Health (Table 2).
After surgery, the median PVR in the TVT group was 200 ml (range 70–450), which was significantly less than that in PVS group: 300 ml (range 180–600) (Wilcoxon rank sum P = 0.008). While all patients in the PVS group had PVR >150 ml after surgery and required CIC, eight patients (53 %) in the TVT group had PVR <150 ml and did not require CIC after surgery. Of the remaining 12 patients in the TVT group, five were using CIC before surgery; the remaining seven had de novo increased PVR (PVR > 150) and required CIC after surgery. The prevalence of de novo urge urinary incontinence (UUI) was significantly higher after TVT (30 % n = 6) than after PVS (10 %, n = 2). Urodynamics 1 year after operation in those patients with de novo urge symptoms reveal low compliance in two patients and unstable bladder contractions in six (four TVT; two PVS). Those patients were completely cured by anticholinergics, and they were all asymptomatic of UUI at each subsequent follow-up visit.
Discussion
This pilot clinical trial compared the efficacy and safety of using synthetic MUS with autologous rectus fascia pubovaginal sling (PVS) in treating women with lower motor neuronal lesion (LMNL) presenting with SUI. The main finding of this study is that the use of MUS in treating female SUI associated with LMNL is feasible, safe, and effective. The objective failure rate with TVT is comparable with that following PVS, with less need for CIC as reflected by lower PVR and a lower percentage of women with PVR >150 in the TVT group compared with the PVS group. Reduction in the number of women with voiding dysfunction in the TVT group results in less need for lifelong CIC, which is always needed in women after the classic PVS. In both groups, there was considerable improvement in symptoms and QoL. Complications were infrequent in both groups, with only one patient experiencing TVT vaginal mesh erosion. The overall reoperation rate for failure was women (20 %) in the TVT group compared with three women (15 %) in the PVS group during the study duration. The prevalence of de novo urge symptoms after TVT was higher after PVS (30 % vs. 10 %). Patients who underwent TVT for nSUI should be followed by urodynamics. Even if postoperative urge symptoms occurred, this did not greatly affect patient satisfaction with the procedure.
To date, there are no evidence-based recommendations about the use of MUS for nSUI; the exact mechanism of action of MUS in nSUI is unknown. The MUS does not help close the open bladder neck in those patients. Many authors have personal experience and prefer not to use TVT in women with nSUI, as these tension-free slings may not provide the necessary compression to achieve continence [19]. Review of the literature revealed only two retrospective studies that evaluated TVT for treating nSUI. One study (12 women with 10-year follow-up) reported that seven patients were completely dry, two improved, and three were lost to follow-up. No urethral erosions were reported. There was no report on urodynamic parameters after TVT. The authors reported that of three women who were voiding spontaneously before TVT, one experienced transient retention postoperatively [15]. Another study (12 women, mean follow-up 2 years) reported that ten patients (83.3 %) were dry whereas one developed detrusor hyperreflexia postoperatively on urodynamics [14]. Athanasopoulos et al. reported on 33 women with nSUI treated with the standard PVS; 25 (75 %) were totally dry, five (15.15 %) improved, and three were considered failures. All patients required postoperative CIC [20].
The strength of this study comes from the fact that outcome was evaluated in a prospective structured methodology. Both subjective and urodynamic criteria were reported at regular follow-up periods. This is the first study to assess urodynamic parameters for patients before and after surgery. Obviously, a limitation of this study is the small sample size; however, it is related to the rare and unique nature of the study population. Nonetheless, within our current sample of 40, if there is a true difference in favor of the standard treatment of 5 %, then our 40 patients would provide 80 % power to exclude a difference in favor of the standard group of >40 % when using a noninferiority, one-sided power estimation. While we believe 40 % difference might be a large difference to define superior treatment, we believe within the context of the rare and challenging clinical condition, our data adds to the current literature. Another limitation is the lack of randomization. When considering the lack of evidence supporting the use of TVT in treating SUI in women with bladder LMNL, our institutional ethical committee refused randomization and demanded that participating patients in our trial select the treatment approach. To avoid bias associated with differences in symptom severity in the PVS group compared with the MUS group, specifically in parity, preoperative total score on the modified IIQ-7, preoperative PVR >150, and preoperative CIC were applied. We used regression models to adjust for those differences to the best of our ability.
Conclusions
Both traditional PVS and TVT can be used effectively and safely to treat women with nSUI associated with spinal pathology. While postoperative CIC is needed in all patients after PVS, de novo postoperative CIC after TVT can be avoided in 50 % of patients. The use of MUS might be of great benefit to women with lower motor neuron spinal pathologies presenting with SUI who have good voiding function with PVR <150 and do not require CIC at baseline; postoperative CIC can be avoided in 50 % of such patients.
Abbreviations
- TVT :
-
tension-free vaginal tape
- PVS :
-
Pubovaginal Sling
- nSUI :
-
neurogenic stress urinary incontinence
- UDI-6 :
-
Urogenital Distress Inventory Short Form−6
- IIQ-7 :
-
Incontinence Impact Questionnaire Short Form−7
- PVR :
-
postvoid residual urine volume
- CIC :
-
Clean intermittent self catheterization
References
Haylen BT, de Ridder D, Freeman RM et al (2010) An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J 21:5–26
El-Azab AS, Mohamed EM, Sabra HI (2007) The prevalence and risk factors of urinary incontinence and its influence on the quality of life among Egyptian women. Neurourol Urodyn 26:783–788
Delancey JO (2002) Fascial and muscular abnormalities in women with urethral hypermobility and anterior vaginal wall prolapse. Am J Obstet Gynecol 187:93–98
Petros PE (1998) The pubourethral ligaments–an anatomical and histological study in the live patient. Int Urogynecol J Pelvic Floor Dysfunct 9:154–157
Harrop JS, Hunt GE Jr, Vaccaro AR (2004) Conus medullaris and cauda equina syndrome as a result of traumatic injuries: management principles. Neurosurg Focus 16:e4
Fidas A, MacDonald HL, Elton RA et al (1988) Neurophysiological measurements in patients with genuine stress incontinence of urine and the relation of neurogenic defects to the presence of spina bifida occulta. Br J Urol 62:46–50
Watanabe T, Chancellor MB, Rivas DA (1998) Neurogenic voiding dysfunction. In: Nitti VW (ed) Practical Urodynamics. W.B. Saunders Company, Philadelphia, pp 142–146
Daneshmand S, Ginsberg DA, Bennet JK et al (2003) Puboprostatic sling repair for treatment of urethral incompetence in adult neurogenic incontinence. J Urol 169:199–202
De Vocht TF, Chrzan R, Dik P et al (2010) Long-term results of bulking agent injection for persistent incontinence in cases of neurogenic bladder dysfunction. J Urol 183:719–723
Chartier-Kastler E, Van Kerrebroeck P, Olianas R et al (2011) Artificial urinary sphincter (AMS 800) implantation for women with intrinsic sphincter deficiency: a technique for insiders? BJU Int 107:1618–1626
Austin PF, Westney OL, Leng WW et al (2001) Advantages of rectus fascial slings for urinary incontinence in children with neuropathic bladders. J Urol 165:2369–2371
Gormley EA, Bloom DA, McGuire EJ et al (1994) Pubovaginal slings for the management of urinary incontinence in female adolescents. J Urol 152:822–825
Chung E, Cartmill RA (2010) 25-year experience in the outcome of artificial urinary sphincter in the treatment of female urinary incontinence. BJU Int 106:1664–1667
Hamid R, Khastgir J, Arya M et al (2003) Experience of tension-free vaginal tape for the treatment of stress incontinence in females with neuropathic bladders. Spinal Cord 41:118–121
Abdul-Rahman A, Attar KH, Hamid R et al (2010) Long-term outcome of tension-free vaginal tape for treating stress incontinence in women with neuropathic bladders. BJU Int 106:827–830
El-Azab AS, Mascha EJ (2009) Arabic validation of the urogenital distress inventory and adapted incontinence impact questionnaires-short forms. Neurourol Urodyn 28:33–39
Schafer W, Abrams P, Liao L et al (2002) Good urodynamic practices: uroflowmetry, filling cystometry, and pressure-flow studies. Neurourol Urodyn 21:261–274
Chaikin DC, Rosenthal J, Blaivas JG (1998) Pubovaginal fascial sling for all types of stress urinary incontinence: long-term analysis. J Urol 160:1312–1316
Lee E, Nitti VW, Brucker BM (2012) Midurethral slings for all stress incontinence: a urology perspective. Urol Clin N Am 39:299–310
Athanasopoulos A, Gyftopoulos K, McGuire EJ (2012) Treating stress urinary incontinence in female patients with neuropathic bladder: the value of the autologous fascia rectus sling. Int Urol Nephrol 44:1363–1367
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
El-Azab, A.S., El-Nashar, S.A. Midurethral slings versus the standard pubovaginal slings for women with neurogenic stress urinary incontinence. Int Urogynecol J 26, 427–432 (2015). https://doi.org/10.1007/s00192-014-2521-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-014-2521-8