Abstract
Objective/background
The aim of this study was to evaluate the efficacy of the autologous fascia rectus sling in treating stress urinary incontinence in female patients with neuropathic bladder. Furthermore, correlations between preoperative parameters and outcome were evaluated.
Methods and design
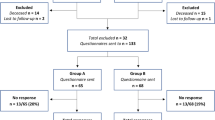
We retrospectively reviewed operative logs from a single surgeon (EM) of 33 female patients with neuropathic bladder treated over a 3-year period for stress urinary incontinence by implantation of an autologous fascia rectus sling. Efficacy was evaluated objectively in terms of the number of pads used per day, while subjective patient satisfaction was also recorded using a global assessment question. Possible correlations between age, obesity, preoperative Valsalva leak point pressure and incontinence severity and outcome were investigated using univariate analysis.
Outcome measures and results
The mean follow-up time was 52 months, while the mean age of the patients was 37 years. Causes of neuropathic bladder were myelomeningocele in 21 (63.63 %) and spinal cord injury in 12 patients (36.36 %). A total of 30 patients were successfully treated and satisfied with the outcome of the operation (90.9 %). Twenty-five patients (75.75 %) were totally dry, while 5 patients (15.15 %) had markedly improved but still required one pad per day. The complication rate was 15.20 %. Univariate analysis failed to show any correlation between the final outcome and the checked parameters.
Conclusion
The free autologous rectus fascia sling is a highly effective technique for the treatment of female stress incontinence in patients with neuropathic bladder, while the morbidity is mild.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The suburethral sling procedure was first described by von Giordano in 1907, but it was not until its re-introduction in 1978 by McGuire and Lytton that it gained increased clinical use [1]. The pubo-vaginal sling (PVS) is a widely used suburethral procedure for the treatment of female stress urinary incontinence (SUI). Urinary stress incontinence is frequently present in female patients with neuropathic bladder as a result of spinal cord injury or other underlying neurological condition and represents a major disabling feature in females with neurovesical dysfunction [2]. Neuropathic female stress urinary incontinence and non-neuropathic female stress urinary incontinence are different entities with different pathophysiology. The goal of the procedure in the case of neuropathic stress urinary incontinence is to induce increased outlet resistance so that the patient can be managed with self intermittent catheterization (SIC), a common and acceptable method of bladder emptying in neuropathic patients. In patients with neurogenic incontinence, the dysfunction of lower urinary tract is combined with bladder problems such as decreased bladder capacity, low compliance and neuropathic overactivity which can be even life-threatening. As a rule, treatment of neurogenic incontinence follows or is combined with medical or surgical methods aiming to decrease bladder pressure to acceptable levels; this has been the initial goal for our patient cohort. We evaluated the efficacy of the autologous free rectus fascia sling for the treatment of stress urinary incontinence in female patients with neuropathic bladder, through our experience at a single institution from a single surgeon over a period of 3 years. Patient satisfaction and morbidity were also recorded. In addition, we investigated possible correlations between preoperative parameters and outcome.
Patients and methods
A retrospective chart review for 33 female SUI patients who underwent an autologous PVS rectus fascia sling by a single surgeon (E.M.) during a period of 3 years was conducted, following Institutional Review Board (IRB) approval. Preoperative evaluation included urogynecological history and physical examination, urinalysis and flexible urethrocystoscopy. Patients also underwent fluoroscopic urodynamic studies (FUDS) to quantify the degree of intrinsic sphincter deficiency (ISD) and to evaluate detrusor function. Valsalva leak point pressure (VLPP) was also estimated. Demographic data included age and presence of obesity (BMI > 35). Preoperative incontinence severity was quantified by the number of pads used per day and stratified as mild (0–1 pads per day), moderate (2–4 pads) and severe (5 or more pads). The operative technique has been previously described [3]. The goal of the procedure in this cohort of patients was to induce increased outlet resistance so that the patient could be managed with SIC. Selection criteria for our group of patients were the presence of neurogenic incontinence and the willingness of patients to perform SIC.
Primary outcome measures after surgery included urinary continence assessed by the mean number of pads used per day [4], clinical evaluation and patients’ expressed satisfaction. Persistent or recurrent urethral incontinence was recorded as “failure” and was defined as leakage requiring >1 pad per day during follow-up. The use of 1 pad per day was defined as “improvement” only if this represented a reduction in pad use greater of or equal to 50 % and, additionally, was reported as “satisfactory” by the patient. “Cure” was defined as no leakage per urethra. Patient satisfaction was evaluated by the Yes/No answer to the single, global assessment question: “Are you satisfied with the outcome of the performed operation?” Postoperative surgical complications and re-operations were also recorded. Correlation of outcome to the following preoperative factors was also evaluated: patient age (≤65 vs. ≥66 years), presence of obesity, incontinence severity, VLPP (≤60 cm H2O, or 61–90 cm H2O, or ≥91 cm H2O).
Statistical analyses were performed using the commercially available Graph Pad PRISM 5.0 statistical software. Student’s t test and Pearson chi-square test were used for continuous and non-continuous variables accordingly. A 5 % significance level was used for all tests.
Results
The mean follow-up time was 52 months (range: 12–62), while the mean age of the patients was 37 years (range: 10–67). Causes of neuropathic bladder were myelomeningocele in 21 (63.63 %) and spinal cord injury in 12 patients (36.36 %). Preoperative incontinence severity was mild in 3 (9.1 %), moderate in 3 (9.1 %) and severe in 27 (81.8 %) cases.
Preoperative urodynamic evaluation revealed low bladder pressure in 9 patients. The remaining 24 patients initially received medical treatment with triple combination of antimuscarinics plus α-blocker plus imipramine, as previously described [5]. This treatment was successful in lowering bladder pressure in 7 patients. For the remaining 17 non-responders, concomitant augmentation cystoplasty or myectomy was performed in 14 patients (42.42 % of total) and 3 patients (9.1 % of total), respectively. Postoperatively, all patients had intravesical pressure within safe limits (<40 mmH2O). Pre- and postoperative urodynamic parameters are shown in Table 1.
A total of 30 patients (90.9 %) were considered successfully treated (cured + improved). Twenty-five patients (75.75 %) were totally dry, while 5 patients (15.15 %) had markedly improved but still required one pad per day. All these patients were further treated with SIC for bladder emptying. Failure was encountered in only 3 patients (9.09 %) (Table 2). In one of these patients, an artificial sphincter was implanted; in the remaining two patients, closure of bladder neck combined with vesico-vesicostomy was performed. According to the global assessment question, 30 patients (90.9 %) were satisfied with the outcome of the operation, a percentage matching the “cure + improvement” rate. The complication rate was 15.20 % (5/33). Sling erosion, vesicovaginal fistula and urethral stenosis occurred in one patient each and required re-operation (3/33, 9.10 %), while 2 patients developed bladder overactivity during the first postoperative week which was managed successfully with anticholinergics. The vesicovaginal fistula and the urethral stenosis were successfully treated surgically, while the sling erosion occurred in one patient of the failure group, and a surgical take-down of the sling was performed. During the follow-up period and while patients were managed with SIC, improvement of upper urinary tract dilatation was observed in 14 out of 18 patients with previous hydronephrosis on ultrasound scan. Furthermore, only 5 patients presented with febrile urinary tract infection (UTI) during the follow-up period.
In an attempt to identify possible factors affecting outcome, we evaluated the following preoperative parameters: patient age, obesity, incontinence severity, preoperative VLPP. Univariate analysis did not reveal any statistical significant differences for the above parameters.
Discussion
Success rates for the PVS procedure in the general population of female patients with SUI range from 73 to 100 % [6–8]. Traditionally, autologous slings have been constructed from fascia obtained from the abdominal rectus fascia or tensor fascia lata. These autografts have the benefit of a significantly decreased risk of rejection or erosion when compared to synthetic (allogenic or xenogenic) slings [9]. So far, there is extensive evidence in the literature supporting the use of native tissue with cure rates ranging from 80 to 93 % [10]. Alternatively, a tension-free vaginal tape can be used as a sling procedure [11] but despite its effectiveness, this procedure is rather costly in comparison with PVS. Moreover, the high cost of an artificial sphincter limits its potential advantages [12].
In the current study in a population with neurogenic stress incontinence, an objective measure of outcome was provided by the number of pads used per day before and after operation. The overall success rate in our series was 90.9 % (cure + improvement). These patients were happy with the result, as reflected at the identical subjective improvement rate (90.9 %). The success rate in our series is comparable to what has been reported previously in a few existing trials where PVS has been used for the treatment of SUI of neuropathic origin [6, 13–15]. In a small study where tension-free vaginal tape was used with very long follow-up, 7 out of 9 patients were completely dry and 2 improved [13]. It is worth to mention that in our cohort of patients, the majority had had severe incontinence. The presence of low-pressure bladder is clearly a prerequisite for the performance (and success) of the sling procedure; proper management of bladder dysfunction by anticholinergics (or botulinum toxin as a newer approach) is important. It is also important to mention that the combination of low-pressure bladder combined with SIC generally improves previous upper tract dilatation and function and exerts minimal risk for severe UTIs. Moreover, in neurogenic patients, it is of critical importance to accurately distinguish whether urinary incontinence is related to neuropathic detrusor dysfunction or to sphincter and/or bladder neck insufficiency [15].
We did not find any statistically significant results when the effect of preoperative parameters such as patient age, obesity, severity of incontinence and preoperative VLPP on outcome was investigated. Hence, we cannot recommend on any special parameter to improve patient selection and outcome or even to decrease complications. A meticulous dissection in the right plane at the level of urethra probably would be the most important surgical tip.
Our results should be viewed within the limits of a retrospective study. Moreover, one should keep in mind that the pad scoring system, although practical and “accurate” as it may be, cannot exclude bias created by pad use for reasons other than SUI, for example, urgency. Nevertheless, this is a series with an adequate follow-up, attained by a single surgeon, and this may contribute to the uniformity of the operative results.
In conclusion, our results indicate that the free autologous rectus fascia sling is a highly effective technique for the treatment of female stress incontinence in patients with neuropathic bladder, while the morbidity remains acceptable.
References
Albo ME, Richter HE, Brubaker L, Urinary Incontinence Treatment Network et al (2007) Burch colposuspension versus fascial sling to reduce urinary stress incontinence. N Engl J Med 356(21):2143–2155
Hunskaar S et al (1999) Epidemiology and natural history of urinary incontinence. In: Abrams P, Khoury S, Wein AJ (eds) Incontinence, 1st edn. Health Publications Ltd, Plymouth, pp 199–226
Athanasopoulos A, Gyftopoulos K, McGuire EJ (2011) Efficacy and preoperative prognostic factors of the autologous fascia rectus sling for the treatment of female stress urinary incontinence. Urology 78(5):1034–1039
Stoffel JT, Smith G, Crivellaro S, Smith JJ 3rd, Bresette JF (2009) Self-reported pad use per day reflects patient quality of life after pubovaginal sling surgery. Int Urogynecol J Pelvic Floor Dysfunct 20(11):1321–1325
Cameron AP, Clemens JQ, Latini JM, McGuire EJ (2009) Combination drug therapy improves compliance of the neurogenic bladder. J Urol 182(3):1062–1067
Ghoneim GM, Shaaban A (1994) Sub-urethral slings for treatment of stress urinary incontinence. Int Urogynecol J 5:228–232
McGuire EJ, O’Connell HE (1995) Surgical treatment of intrinsic urethral dysfunction. Slings. Urol Clin North Am 22:657–664
Chaikin DC, Rosenthal J, Blaivas JG (1998) Pubovaginal fascial sling for all types of stress urinary incontinence: long-term analysis. J Urol 160:1312–1316
Leach GE, Dmochowski RR, Appell RA, Blaivas JG, Hadley HR, Luber KM, Mostwin JL, O’Donnell PD, Roehrborn CG (1997) Female stress urinary incontinence clinical management guidelines panel summary report on surgical management of female stress urinary incontinence. J Urol 158:875–880
Simsiman AJ, Powell CR, Stratford RR, Menefee SA (2005) Suburethral sling materials: best outcome with autologous tissue. Am J Obstet Gynecol 193(6):2112–2116
Hamid R, Khastgir J, Arya M, Patel H, Shah P (2003) Experience of tension-free vaginal tape for the treatment of stress incontinence in females with neuropathic bladders. Spinal Cord 41:118–121
Bosch JL, Klijn AJ, Schroder FH, Hop WC (2000) The artificial urinary sphincter in 86 patients with intrinsic sphincter deficiency: satisfactory actuarial adequate function rates. Eur Urol 38:156–160
Austin PF, Westney OL, Leng WW, McGuire EJ, Ritchey ML (2001) Advantages of rectus fascial slings for urinary incontinence in children with neuropathic bladders. J Urol 165(6 Pt 2):2369–2371 (discussion 2371–22372)
Blaivas JG, Jacobs BZ (1991) Pubovaginal fascial sling for the treatment of complicated stress urinary incontinence. J Urol 145:1214–1218
Abdul-Rahman A, Attar KH, Hamid R, Shah PJ (2010) Long-term outcome of tension-free vaginal tape for treating stress incontinence in women with neuropathic bladders. BJU Int 106(6):827–830
Conflict of interest
A. Athanasopoulos: is or has been an investigator, lecturer and consultant for pharmaceutical companies producing or developing drugs for lower urinary tract symptoms (Pfizer, Astellas, Ucb, Lilly, Allergan, Bard, Amgen). K. Gyftopoulos: None. E. McGuire: financial interest and/or other relationship with Pfizer, Novartis, Astellas, Carbon Medical technologies, Pharmacia and Ortho-McNeil.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Athanasopoulos, A., Gyftopoulos, K. & McGuire, E.J. Treating stress urinary incontinence in female patients with neuropathic bladder: the value of the autologous fascia rectus sling. Int Urol Nephrol 44, 1363–1367 (2012). https://doi.org/10.1007/s11255-012-0247-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-012-0247-4