Abstract
Aim
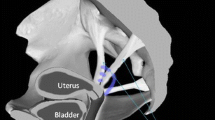
To review the safety and efficacy of anterior vaginal compartment pelvic organ prolapse surgery.
Methods
Every 4 years and as part of the Fifth International Collaboration on Incontinence we reviewed the English-language scientific literature after searching PubMed, Medline, Cochrane library and the Cochrane database of systematic reviews, published up to January 2012. Publications were classified as level 1 evidence (randomised controlled trials [RCT] or systematic reviews), level 2 (poor quality RCT, prospective cohort studies), level 3 (case series or retrospective studies) and level 4 case reports. The highest level of evidence was utilised by the committee to make evidence-based recommendations based upon the Oxford grading system. A grade A recommendation usually depends on consistent level 1 evidence. A grade B recommendation usually depends on consistent level 2 and/or 3 studies, or “majority evidence” from RCTs. A grade C recommendation usually depends on level studies or “majority evidence” from level 2/3 studies or Delphi processed expert opinion. A grade D “no recommendation possible” would be used where the evidence is inadequate or conflicting and when expert opinion is delivered without a formal analytical process, such as by Delphi.
Results
Absorbable mesh augmentation of anterior compartment native tissue repair improves the anatomical outcome compared with native tissue repair alone with no increased complication rate in meta-analysis of 2 RCTS (grade B). Biological grafts in meta-analysis have improved anatomical outcomes with no change in subjective outcomes compared with native tissue repairs (grade B). There is conflicting level 1 evidence to support porcine dermis and a single RCT to support small intestine submucosa as graft agents in anterior compartment prolapse surgery (grade B). Consistent level 1 data support a superior anatomical outcome for polypropylene mesh compared with a biological graft in the anterior compartment. Mesh exposure rate was significantly higher in the polypropylene mesh group (grade A). Consistent level 1 evidence demonstrates superior subjective and objective outcomes following anterior transvaginal polypropylene mesh as compared to anterior colporrhaphy (grade A). These outcomes did not translate into improved functional results using validated questionnaires or a lower reoperation rate for prolapse. The mesh group was also associated with longer operating time, greater blood loss and apical or posterior compartment prolapse as compared with anterior repair. Anterior polypropylene mesh had a mesh extrusion rate of 10.4 % with 6.3 % requiring a surgical correction (grade B). Single level 3 evidence does not support the use of transvaginal polypropylene mesh for recurrent anterior vaginal wall prolapse (grade C).
Conclusion
Polypropylene anterior compartment mesh offers improved objective and subjective outcomes compared with native tissue repair; however, these benefits must be considered in the context of increased morbidity associated with anterior polypropylene transvaginal mesh.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ahlfelt stated in 1909 that the only remaining problem in plastic gynaecology was the permanent cure of cystocele, and now, more than a century, later this problem persists [1]. Following high reported objective failure rates and reoperation rates after native tissue repairs and the success of suburethral tapes in continence surgery and mesh utilised abdominally at sacral colpopexy, the last decade has seen an unprecedented introduction of biological and permanent meshes into the management of anterior compartment prolapse.
Native tissue repairs
Historically, anterior colporrhaphy was the standard procedure in the management of anterior compartment prolapse with objective success rates ranging from 80 to 100 % in retrospective series [2–5]. White [6], as early as 1912, demonstrated the importance of paravaginal defects in anterior compartment prolapse (Table 1). Richardson et al. [7], in 1976, described a series of defects in the pubocervical fascia explaining why no single repair should be applied indiscriminately to all patients with anterior compartment defects. He also advocated the abdominal paravaginal repair, which has a 75–97 % success rate for cystoceles reported in case series (Table 1) [7, 27–30]. The surgical technique of the laparoscopic paravaginal repair is well described; however, little information is available on the efficacy of this approach. Shull et al. [31] also reported on the safety and efficacy of vaginal paravaginal repair in 1994. Although the success rates of the vaginal paravaginal repair for cystoceles in case series vary from 67 to 100 % [6, 31–35], significant complications have been reported recently. Mallipeddi et al. [34] reported on complications in a series of 45 patients including: 1 with bilateral ureteric obstruction, 1 with retropubic haematoma requiring surgery, 2 with vaginal abscesses and 2 with transfusions. In a series of 100 women Young et al. [35] reported 21 major complications and a 16 % transfusion rate.
No randomised controlled trials (RCT) have evaluated the abdominal or vaginal paravaginal repair in isolation. Benson et al. [36] and Maher et al. [37] have reported RCTs on upper vaginal prolapse comparing abdominal sacral colpopexy and vaginal sacrospinous colpopexy. Abdominal paravaginal repair was performed in the abdominal group if required and an anterior colporrhaphy with or without vaginal paravaginal laterally. Both authors reported the abdominal group to have a statistically lower rate of postoperative anterior vaginal prolapse than the vaginal group.
Raz et al. [38] popularised the needle suspension-type procedure for cystoceles and reported that success rates in case series may vary from 90 to 98 % [39–41]. The addition of polyglactin mesh to the repair appears to have little impact on the success [42]. Dmochowski et al. [43] reported a lower success rate using a stricter outcome definition of success.
Goldberg et al. [44] reported results from a case–control study of women with cystocele and stress urinary incontinence. He suggested that the addition of the pubovaginal sling to the anterior colporrhaphy significantly reduced the recurrence rate of cystocele from 42 % in the control group to 19 % in the anterior colporrhaphy and sling group (P < 0.05).
In line with our surgical colleagues there has been a move towards the use of prosthesis to augment native tissue repair in reconstructive gynaecology. This movement took much of its impetus from two early papers. First, Olsen et al. [45] reported a reoperation rate of 29 % following prolapse and or continence surgery and Weber et al. [15] reported a 70 % failure rate of native tissue anterior compartment repair. Recent re-evaluation of Olsen’s same demographic 10 years later revealed a significantly lower re-operation rate of 17 % [46] and the reader should be cautious in making conclusions even from these data, as the surgical interventions performed in 1995 are not representative of interventions performed today. More importantly, Weber et al. [15] and Sand et al. [14] in randomised control trials reported anterior colporrhaphy to be successful in the management of cystocele in only 30 % and 57 % respectively. Recent re-analysis of data from Weber’s paper using the hymen as the threshold for objective success reported considerably better outcomes, with only 10 % of subjects developing anatomical recurrence beyond the hymen, 5 % of subjects developing symptomatic recurrence and less than 1 % re-operations at 23 months’ follow-up [47].
During the decade between these initial and subsequent publications surgeons have introduced a plethora of biological and mesh grafts to improve the outcomes of anterior compartment prolapse surgery.
Synthetic grafts in anterior compartment surgery
As seen in Table 2, as early as 1996, Julian et al. [8] demonstrated in a prospective case control study that in women who had undergone at least 2 previous vaginal repairs, the overlaying of a Marlex (Bard) mesh to the anterior colporrhaphy reduced the recurrence rate of cystocele from 33 % to 0 %. The Marlex mesh was associated with a mesh erosion rate of 25 %. Flood et al. [10] in a retrospective review of 142 women with Marlex mesh augmentation of anterior colporrhaphy demonstrated a 100 % success rate for cystoceles at 3.2 years and a mesh erosion rate of only 2 %.
Absorbable meshes are an attractive option as an augmenting material as they offer increased strength during the early healing phase without the long-term complications of permanent mesh and have been evaluated in two randomised controlled trials. Weber et al. [15], in a randomized control trial, compared the anterior colporrhaphy [10], ultra-wide anterior colporrhaphy [43] or anterior colporrhaphy with absorbable polyglactin (Vicryl) 910 mesh [45] in the management of cystocele. The study size was too small to detect small differences in efficacy or adverse events. However, at a mean follow-up of nearly 2 years the groups had similar proportions of women experiencing satisfactory or optimal anatomical results, 30 %, 46 % and 42 % respectively.
Sand et al. [14], in a larger RCT, allocated cystoceles to anterior colporrhaphy alone (n = 70) and to anterior colporrhaphy plus polyglactin mesh underlay (n = 73). At 1 year the success rate in the mesh group was 75 % and significantly greater than the 57 % success rate in the anterior repair group alone (P = 0.02). Concurrent paravaginal defects were present in 11 women and concomitant paravaginal repair was significantly associated with a lower recurrence of cystocele overall (P = 0.02).
A variety of permanent polypropylene mesh overlays have been evaluated in case series for the management of anterior wall prolapse. The anatomical success rate varies from 76 to 100 % [8, 16–18]. Salvatore et al. reported worrying functional outcomes after a prolene mesh overlay, including a mesh erosion rate of 13 %, overactive bladder increasing from 28 to 56 % and dyspareunia increasing from 18 to 38 % postoperatively [16]. More recently, 3 years’ follow-up after the polypropylene mesh overlay in the anterior compartment has been reported. Cervigni et al. reported 218 women and found a 76 % objective success rate at 3 years [18]. Mesh erosions were identified in 12.3 % and vaginal stenosis in 7.7 % [18]. De Tayrac et al. reported 55 women at 3-year review with an 89 % success rate, 9.1 % mesh erosions, 5.5 % mesh shrinkage and 16.7 % dyspareunia [24]. They concluded that lower weight and coated meshes were required to limit the rate of complications and duly reported 132 women, 12 months after low weight coated polypropylene mesh with a 92 % success rate [23]. Unfortunately, local problems remained with mesh erosions in 6.3 % and de novo dyspareunia in 12.8 %. Rane et al. provided a 5-year review of 376 consecutive women with grade 3 anterior compartment prolapse after Perigee (American Medical System, Minnetonka, MN, USA) and reported a 94 % success rate, 11.1 % mesh extrusion rate and deteriorating sexual function in 4 % [53].
Carey et al. [54] performed an RCT comparing anterior and posterior fascial plication and repair with self styled anterior and posterior polypropylene Gynemesh (Ethicon, Somerville, NJ, USA,) overlay and reported no significant advantage to adding a mesh overlay at 1 year. The morbidity in the mesh group was lower than that reported above with a mesh erosion rate of 6.5 % and no difference in dyspareunia and de novo dyspareunia rates between the groups.
Five randomised control trials have been published comparing armed or trans-obturator polypropylene mesh and traditional anterior colporrhaphy (Table 3). Nieminen et al. [25] compared 104 women undergoing anterior compartment prolapse repair with self-styled 6 × 11cm low-weight monofilament four-armed polypropylene mesh (Parietene light, Sofradim Co, Trevoux, France) with 97 undergoing traditional anterior colporrhaphy. Concomitant hysterectomy and posterior compartment prolapse surgery was allowed. At 3 years the objective success (stage 0 or 1 Aa and Ba) rate was 87 % in the mesh group and 59 % in the no mesh group (P <0.001). Awareness of a bulge was seen in 18 % in the repair group compared with 10 % (p = 0.07) in the mesh group. The mesh exposure rate was 19 % with 66 % requiring surgical correction. The reoperation rate for prolapse was 10 % in the native tissue group with all but one of the recurrences in the anterior compartment. In the mesh group the prolapse reoperation was 6 % with all six recurrences occurring in the posterior or apical compartments.
Sivaslioglu et al. reported on 43 undergoing low-weight self-styled polypropylene mesh compared with 42 undergoing site-specific vicryl repair and at 12 months found the objective success rate to be significantly higher at 91 % in the mesh group than at 72 % in the non-mesh group [26]. The mesh erosion rate was 6.9 % and de novo dyspareunia was reported in 4.6 % in the mesh group. Quality of life assessment demonstrated no difference in outcomes between the groups and no patient in either group underwent further surgery for anterior compartment prolapse.
Nguyen and Burchette compared anterior polypropylene (Perigee, AMS) mesh (n = 37) with anterior colporrhaphy (n = 38). At 1 year the objective success rate was higher in the mesh group (89 % vs 55 %). Functional outcomes, including quality of life, sexual activity and dyspareunia, were similar in both groups, with 5 % mesh erosion and 2 % unilateral leg pain that settled at 8 weeks following the mesh surgery (Table 3) [48].
Altman and colleagues reported on behalf of the Nordic transvaginal mesh group a multicentre study (funded by the Karolinska Institute and Ethicon unrestricted grants) comparing anterior colporrhaphy (n = 182) with anterior transvaginal trocar mesh kit (n = 186, Prolift; Ethicon) in women with symptomatic stage II or greater cystocele [50]. Although the need for concomitant prolapse and continence surgery were excluded an undetermined number of women with posterior and apical compartment prolapse well beyond the introitus were included. Reviewers were unblinded, surgeons were reviewers and conflict of interest statements were not available for authors or members of the Nordic transvaginal mesh group. At 1 year, the success rate (composite Point Ba < −1 and absence of vaginal bulging) was significantly greater after the mesh repair (61 %) compared with the colporrhaphy group (35 %). The subjective success rate was also significantly greater after the mesh repair (75 % vs 62 % p = 0.008) compared with the native tissue repair, while no difference was detected on validated pelvic floor questionnaires (Urinary Distress Inventory) between the groups. The Prolift mesh procedure was associated with greater morbidity with a longer operating time, greater blood loss, higher rate of intraoperative cystotomy (3.5 vs 0.5 %), postoperative de novo stress urinary incontinence (12.3 vs 6.0 %), and combined reoperation rate for USI, prolapse and mesh exposure (6 % vs 0.5 %). De novo dyspareunia was seen in 7.3 % after the mesh surgery compared with 2 % after anterior colporrhaphy (p = 0.07); however, no difference was detected between the groups utilising the Pelvic organ Prolapse Urinary Incontinence Questionnaire (PISQ-12). The mesh exposure rate was 11.5 % (21 out of 183)
Last, Vollebregt and colleagues reported a multicentre randomised control trial from the Netherlands with blinded reviewers comparing anterior colporrhaphy (n = 58) with a polypropylene trans-obturator mesh kit (n = 56; Avulta Bard, Covington, LA, USA) for stage 2 primary anterior compartment prolapse [52]. Concomitant hysteropexy and posterior compartment surgery was allowed with hysterectomies being excluded. At 1 year the objective success rate was significantly greater in the mesh group than in the anterior colporrhaphy group (91 % versus 41 %). Reoperation for anterior compartment prolapse was performed in 5 % after native tissue repair and in no patients in the mesh group (p > 0.05). No difference in awareness of prolapse or outcomes using validated questionnaires (Urogenital Distress Inventory and Incontinence Impact Questionnaire) was identified between the groups. The authors attributed the low mesh exposure rate of 4 % to not performing hysterectomy and/or the collagen coating on the polypropylene mesh. Resolution of preoperative dyspareunia occurred in 80 % in the repair group compared with 20 % in the mesh group. De novo dyspareunia was reported in 15 % following mesh and 9 % after native tissue repair and de novo rectocele in 23 % versus 10 % respectively. The authors concluded that despite the significantly improved anatomical outcome in the mesh arm when using a functional outcome as a definition of success that there was not enough evidence to support the use of trans-obturator mesh in primary anterior compartment prolapse surgery.
The 2012 Cochrane meta-analysis [55] found that trans-obturator meshes had a lower rate of recurrence on examination (59 out of 424, 14 %) compared with anterior colporrhaphy alone (200 out of 410, 49 %) RR 3.50, 95 % CI 2.71 to 4.52. This finding was consistent for both the self-styled (RR 3.41, 95 % CI 2.04 to 5.67) [25, 26] and the commercial trans-obturator polypropylene mesh kits (RR 3.53, 95 % CI 2.62 to 4.74) [48, 50, 52]. Three trials demonstrated that anterior colporrhaphy (94 out of 333, 28 %) also had a higher subjective failure rate than anterior transvaginal mesh repair (60 out of 344, 17 %; RR1.62, 95 % CI 1.22, 2.14) [25, 50, 52]. Further prolapse surgery was not significantly more common after anterior colporrhaphy (14 out of 459, 3 %) compared with 6 out of 470 (1.3 %) after trans-obturator polypropylene mesh (RR 2.18, 95 % CI 0.93 to 5.10). No difference was detected between individual studies in validated prolapse-specific questions and meta-analysis was not possible owing to variations in the questionnaires utilised. The operating time and blood loss were significantly greater in the mesh group and there was a tendency towards a lower cystotomy rate (0.4 % vs 2.7 %, RR.0.19, 95% CI 0.03, 1.07) [25, 50], de novo dyspareunia (4 % vs 8 %, RR 0.51, 95 % CI 0.21 to 1.23) and de novo stress urinary incontinence (7.3 % vs 11.4 %, RR 0.65, 95 % CI 0.4 to 1.07) [25, 26, 50] after anterior colporrhaphy. Further continence surgery was performed in 15 out of 368 women following anterior colporrhaphy and 12 out of 380 after the polypropylene mesh procedure (RR 1.29, 95 % CI 0.63 to 2.63). These data need to be interpreted with caution as there were variations in concomitant surgeries. Mesh erosions were reported in 10.4 % of women (41 out of 393) who had anterior compartment polypropylene mesh, and surgical intervention to correct mesh erosion was required in 6.3 % (34 out of 540).
Withagen et al., in an observational study of 150 women undergoing polypropylene mesh kit procedure (Prolift; Ethicon) found that after an isolated anterior polypropylene repair there was a 46 % incidence of stage 2 prolapse in the untreated compartment [56]. Altman et al., performed no concomitant surgery in the study and no difference in posterior compartment prolapse was identified between the groups or postoperatively within the mesh group when evaluating median Point Bp. However, meta-analysis of those studies [25, 52] that reported de novo prolapse in the apical or posterior compartment following anterior compartment mesh repair found a lower rate after the anterior colporrhaphy (14 out of 147, 9.5 %) compared with trans-obturator mesh (26 out of 148, 17.7 %; RR 0.49, 95 % CI 0.24 to 0.97) Both study protocols allowed concomitant posterior compartment prolapse surgery. Although the reoperation rate for prolapse was similar in Nieminen et al. between the two groups, all the reoperations in the AC group were anterior compartment failures and all in the trans-obturator mesh group were in the posterior or apical compartment [25]. This outcome is not surprising as we have seen previously that when the vaginal axis is significantly altered compensatory prolapse can develop in other compartments. Compensatory prolapse is described in the posterior compartment after colposuspension [57] or in the anterior compartment after sacrospinous colpopexy [58, 59].
In the eight trials evaluating 553 patients who underwent some form of transvaginal mesh surgery in the management of anterior compartment prolapse none of the patients underwent surgical intervention for vaginal pain or dyspareunia. This is in contrast to the Food and Drug Administration (FDA) transvaginal mesh alert where vaginal pain and dyspareunia accounted for 39 % of adverse events and was marginally more frequent than mesh erosions at 38 % of adverse event reports (http://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/ucm262435.htm). While mesh exposure and its management remain well described, vaginal pain and dyspareunia associated with anterior trans-obturator polypropylene mesh remain poorly characterised and will be fully evaluated in the complications and sexual function section of this article.
Given the relatively robust anatomical outcomes associated with trans-obturator mesh many clinicians were surprised that many mesh kit manufactures recently elected to introduce trocarless mesh kits and the majority have few or no data supporting their claims of superiority. Most recently, Moore et al. [60] described single-incision anterior elevate (American Medical Systems, Minnetonka, MN, USA) using a lightweight polypropylene graft (24 g/m2) and reported a 92 % objective success rate at 13 months in 60 patients with anterior and/or apical prolapse. No mesh exposures were reported and the authors who reviewed the patients reported a financial relationship with the company manufacturing the product being evaluated.
Another new system involves a polypropylene mesh (Prosima; Ethicon) overlay with arms extending, but not secured to deeper structures. Patients use a vaginal support device that is removed in the outpatient setting 3–4 weeks postoperatively, to splint the mesh while it is being incorporated into the paravaginal tissues. On prospective evaluation performed by surgeons, all of whom have declared financial agreements with the manufacturing company, they reported a 77 % objective success rate (<stage 2 POP-Q) at 1 year [61] and 69 % at 2 years [62] with a mesh exposure rate of 9 % in women with stage 2 anterior and/or posterior compartment prolapse. Significant further prospective comparative trials with blinded independent reviewers are required for all mesh kits.
Biological graft anterior compartment surgery
As an alternative to synthetic prosthetic grafts autologous material may have a lower risk of host rejection or infection. Cosson et al. [63] described an autologous vaginal patch measuring 6–8 cm long and 4 cm wide suspended from the tendinous arches of the pelvic fascia and tucked under the anterior repair. The success rate (<grade 1 POP) was 93 % at a mean follow-up of 16 months.
Allografts from post-mortem tissue banks have been used for many years in orthopaedic surgery and decrease the risk associated with harvesting autologous rectus sheath or fascia lata. Cadaveric fascia lata with or without pubovaginal sling has been utilised to correct anterior compartment prolapse with a success rate varying from 81 to 100 % with acceptable complication rates [64–67]. Gandhi et al. have reported preliminary results of a randomised control trial comparing anterior colporrhaphy alone and augmented with fascia lata graft for cystoceles [68]. At 1 year they were not able to demonstrate that the addition of the fascial lata graft improved outcomes, with the success rate after anterior colporrhaphy alone being 71 % compared with 82 % in those augmented with the fascia lata graft (P = 0.07). No complications were reported. Cadaveric dermis has been employed as a graft material in the anterior compartment with success rates varying from 42 to 84 % at 2 years [69–72]. Concerns regarding prion transmission causing infectious diseases [73] or residual antigenicity [74] that may cause host graft reactions have encouraged the use of porcine or bovine xenografts, as detailed in Table 4.
Leboeuf et al. retrospectively reviewed 24 women with native tissue four corner defect repair (FDR) and 19 FDR with porcine dermis [75]. At 15 months the success rate was 100 % in the FDR group and reduced to 84 % if porcine dermis overlay was utilised. Wheeler et al. reported on 36 women who all underwent high uterosacral vault suspension with anterior repair augmented with porcine dermis and at 17 months found a 50 % recurrence rate [78]. The authors highlighted that despite the high objective failure rate more that 90 % of the women were satisfied or somewhat satisfied with the repair and 83 % would undergo the surgery again. Handel et al. retrospectively compared anterior colporrhaphy (n = 18), porcine dermis (n = 56) and polypropylene graft (n = 24) in those with cystocele [80]. The success rate at 13 months was 94 %, 64 % and 96 % respectively with a 21 % rate of vaginal extrusion of the porcine dermis graft. In contrast to these relatively disappointing results, a number of groups have reported satisfactory objective results utilising porcine dermis [77, 81].
Meschia et al., in a multicentre randomised clinical trial, compared anterior colporrhaphy (n = 103) and anterior colporrhaphy augmented with 4- × 7-cm piece of porcine dermis [79]. The success rate at 1 year was 93 % in the anterior colporrhaphy with porcine graft overlay group compared with 81 % in the anterior colporrhaphy alone group (P < 0.001) with a 1 % rate of graft erosion.
Hviid et al. reported a smaller randomised controlled trial comparing polyglactin plication anterior colporrhaphy and a porcine dermis 4- × 7-cm graft at 1 year [84]. The objective failure rate (defined as point Ba ≥ −1) was 2 out of 28 in the porcine dermis group compared with 4 out of 26 in the anterior colporrhaphy group and was not significantly different. Guerette et al. compared the anterior colporrhaphy group (n = 17) and anterior colporrhaphy with bovine pericardium collagen (n = 27) matrix graft reinforcement and reported no difference on objective examination with success rate of 63 % after the AC and 77 % with bovine pericardium collagen repair at 2 years [83]. The reoperation rate for prolapse was 37 % in the AC group and 23 % in the bovine pericardium group. De novo dyspareunia occurred in 5 % following AC only. There was no difference in quality of life outcomes between the groups utilising the Urinary Distress Inventory and the Pelvic Organ Prolapse and Incontinence Sexual Questionnaire.
Feldner et al. compared anterior colporrhaphy with a 7- × 10-cm small intestine submucosa (SIS) graft in a randomised control trial and demonstrated reduced operating time in the AC group (30 min vs 46) compared with SIS (p = 0.02) [85]. The objective failure rate of 33 % (9 out of 27) was significantly higher after the AC versus 14 % (4 out of 29) in the SIS group. The dyspareunia rate was similar in both groups (AC 4 out of 27 vs 5 out of 20 SIS) and no reoperations were reported. Prolapse quality of life assessment (P-QOL) improved postoperatively in both groups with no significant difference between the groups. In another RCT, Natale et al. compared polypropylene mesh (Gynemesh) with porcine dermis (Pelvicol). At 2 years, significantly fewer women had anterior vaginal wall recurrence in the mesh group 28 % (27 out of 96) vs 44 % (41 out of 94) of the porcine graft group (RR 0.64, 95 % CI 0.43 to 0.96). Mesh erosion was seen in 6.3 % following mesh surgery. Although similar numbers of women reported dyspareunia (10 vs 12), the authors reported superior sexuality outcomes in the porcine graft group compared with polypropylene mesh (p = 0.03) [86].
Finally, Menefee et al., in a randomised control trial, compared three operations, anterior colporrhaphy, vaginal paravaginal repair using porcine dermis graft and vaginal paravaginal with self-styled polypropylene mesh and also reported a higher objective success rate after the polypropylene mesh 86 % (25 out of 29) compared with 52 % (12 out of 23) in the porcine dermis arm [87] and 53 % (10 out of 19) in the AC arm. The subjective failure rate was not significantly different and was 3.4 %, 12 % and 13 % respectively. The graft erosion rate was 1 out of 23 (4.3 %) in the porcine dermis group and 4 out of 29 (13.8 %) in the mesh group.
The 2012 Cochrane meta-analysis concluded that when anterior colporrhaphy was compared with any biological graft the objective failure rate in the anterior compartment was significantly higher in the anterior colporrhaphy group (56 out of 222; 25 %) compared with the biological graft group (31 out of 218; 14 %) [55]. Results from three trials [68, 79, 83] demonstrated no difference in prolapse symptoms when native tissue repair was compared with biological graft repair (RR 1.03 0.61 to 1.75). The methodology and nature of the different biological grafts utilised in five trials [78, 79, 83, 84, 85, 87] were considered to be too dissimilar to combine with any other results in a meta-analysis, except to highlight that two RCTs [85, 87] demonstrated superior objective outcomes following polypropylene mesh compared with porcine graft overlay.
While many clinicians believe that the primary role of polypropylene mesh may be in complex or high-risk prolapse, such as recurrent prolapse, there is little evidence to support these proposals. Fayyad et al. prospectively evaluated 36 women with recurrent anterior compartment prolapse and reported an objective success rate (less than stage 2 anterior compartment prolapse) of 47 % with a mesh exposure rate of 19 % [88].
In a prospective multicentre Dutch RCT trial women who had undergone prior prolapse surgery were randomised between native tissue repairs and tension-free vaginal polypropylene mesh [89]. Allocation concealment was not confirmed and patient, surgeon and assessor were not blinded. Surgeons performed the reviews and all authors declared a financial relationship with the company manufacturing the commercial mesh product. Unfortunately, the two groups were significantly different preoperatively, pointing to a systematic failure in the randomisation process, which discredits the remaining findings of the manuscript.
The reported failure rate in the native tissue group using an unorthodox outcome definition (no prolapse in the treated compartment or reoperation) was 45 % AC vs 9 % mesh group at 1 year. Utilising the definition any grade 2 prolapse or subsequent prolapse surgery, the failure rate was 66 % in the conventional surgery group compared with 49 % (p = 0.03) in the mesh group. The mesh exposure rate was 16.7 % with 6 % undergoing surgical intervention. Utilising the Patients’ Global Impression of Improvement (PGII) and Urogenital Distress Inventory, both groups had similar outcomes.
The following conclusion can be made regarding surgical interventions for anterior vaginal compartment repairs:
-
Absorbable mesh augmentation of native tissue repair improves the anatomical outcome compared with native tissue repair alone, with no increased complication rate in the meta-analysis of two RCTS (grade B)
-
Biological grafts in meta-analysis have improved anatomical outcomes with no change in subjective outcomes compared with native tissue repairs (grade B). Conflicting level 1 evidence supports porcine dermis graft [81, 84, 87] and single RCT supports small intestine submucosa as a graft agent in anterior compartment prolapse surgery (grade B) [85].
-
Consistent level 1 data support a superior anatomical outcome for polypropylene mesh compared with biological graft (Pelvicol) in the anterior compartment [85, 87]. The mesh exposure rate was significantly higher in the polypropylene mesh group (grade A)
-
Consistent level 1 evidence demonstrates improved anatomical and subjective outcomes for polypropylene mesh compared with anterior colporrhaphy (grade A). These outcomes did not translate into improved functional outcomes using validated questionnaires or a lower reoperation rate for prolapse. The mesh group was also associated with longer operating time, greater blood loss and a non-significant tendency towards higher cystotomy, de novo dyspareunia and de novo stress urinary incontinence rate compared with AC. Apical or posterior compartment prolapse was significantly more common following polypropylene mesh and the mesh extrusion rate was 10.4 %, with 6.3 % undergoing surgical correction (grade B)
-
Single level 3 evidence does not support the use of polypropylene mesh for recurrent anterior vaginal wall prolapse (grade C)
References
White GR (1909) Cystocele. JAMA 853:1707–1710
Stanton SL, Hilton P, Norton C, Cardozo L (1982) Clinical and urodynamic effects of anterior colporrhaphy and vaginal hysterectomy for prolapse with and without incontinence. Br J Obstet Gynaecol 89(6):459–463
Macer GA (1978) Transabdominal repair of cystocele, a 20 year experience, compared with the traditional vaginal approach. Am J Obstet Gynecol 131(2):203–207
Walter S, Olesen KP, Hald T, Jensen HK, Pedersen PH (1982) Urodynamic evaluation after vaginal repair and colposuspension. Br J Urol 54(4):377–380
Porges RF, Smilen SW (1994) Long-term analysis of the surgical management of pelvic support defects. Am J Obstet Gynecol 1994(171):1518–1528
White GR (1912) An anatomic operation for the cure of cystocele. Am J Obstet Dis Women Children 65:286–290
Richardson AC, Lyon JB, Williams NL (1976) A new look at pelvic relaxation. Am J Obstet Gynecol 126:568
Julian TM (1996) The efficacy of Marlex mesh in the repair of severe, recurrent vaginal prolapse of the anterior midvaginal wall. Am J Obstet Gynecol 175(6):1472–1475
Nicita G (1998) A new operation for genitourinary prolapse. J Urol 160(3 Pt 1):741–745
Flood CG, Drutz HP, Waja L (1998) Anterior colporrhaphy reinforced with Marlex mesh for the treatment of cystoceles. Int Urogynecol J Pelvic Floor Dysfunct 9(4):200–204
Migliari R, Usai E (1999) Treatment results using a mixed fiber mesh in patients with grade IV cystocele. J Urol 161(4):1255–1258
Migliari R, De Angelis M, Madeddu G, Verdacchi T (2000) Tension-free vaginal mesh repair for anterior vaginal wall prolapse. Eur Urol 38(2):151–155
Natale F, Marziali S, Cervigni M (2000) Tension-free cystocele repair(TCR): longterm follow-up. Int Urogynecol J Pelvic Floor Dysfunct 11 [Supp 1]:S51
Sand PK, Koduri S, Lobel RW et al (2001) Prospective randomized trial of polyglactin 910 mesh to prevent recurrence of cystoceles and rectoceles. Am J Obstet Gynecol 184(7):1357–1362
Weber AM, Walters MD, Piedmonte MR, Ballard LA (2001) Anterior colporrhaphy: a randomized trial of three surgical techniques. Am J Obstet Gynecol 185(6):1299–1304
Salvatore S, Soligo M, Meschia M, Luppino G, Piffarotti P, Arcari V (2002) Prosthetic surgery for genital prolapse: functional outcome. Neurourol Urodyn 21(4):296–297
O’Reilly BA, Dwyer PL. Functional results of transvaginal surgery with atrium polypropylene mesh. Int Urogynecol J Pelvic Floor Dysfunct 2003; Proceeds 28th International Urogynecology Meeting Buenos Aires: Abstract 90
Cervigni M, Natale F, La Penna C, Panae M, Mako A (2008) Transvaginal cystocele repair with polypropylene mesh using a tension-free technique. Int Urogynecol J Pelvic Floor Dysfunct 19(4):489–496
Jo H, Kim JW, Park NH, Kang SB, Lee HP, Song Y-S (2007) Efficacy and outcome of anterior vaginal wall repair using polypropylene mesh (Gynemesh). J Obstet Gynaecol Res 33(5):700–704
Rodriguez LV, Bukkapatnam R, Shah SM, Raz S (2005) Transvaginal paravaginal repair of high-grade cystocele central and lateral defects with concomitant suburethral sling: report of early results, outcomes, and patient satisfaction with a new technique. Urology 66(5, Suppl 1):57–65
Amrute KV, Eisenberg ER, Rastinehad AR, Kushner L, Badlani GH (2007) Analysis of outcomes of single polypropylene mesh in total pelvic floor reconstruction. Neurourol Urodyn 26(1):53–58
de Tayrac R, Gervaise A, Chauveaud A, Fernandez H (2005) Tension-free polypropylene mesh for vaginal repair of anterior vaginal wall prolapse. J Reprod Med 50(2):75–80
de Tayrac R, Devoldere G, Renaudie J et al (2007) Prolapse repair by the vaginal route using a new protected low-weight polypropylene mesh; 1-year functional and anatomical outcome in prospective multicentre study. Int Urogynecol J Pelvic Floor Dysfunct 18(3):251–256
de Tayrac R, Picone O, Chauveaud-Lambling A, Fernandez H (2006) A 2-year anatomical and functional assessment of transvaginal rectocele repair using a polypropylene mesh. Int Urogynecol J Pelvic Floor Dysfunct 17(2):100–105
Nieminen K, Hiltunen R, Takala T et al (2010) Outcomes after anterior vaginal wall repair with mesh: a randomized, controlled trial with a 3 year follow-up. Am J Obstet Gynecol 203(3):235e1–235e8
Sivaslioglu A, Unlubilgen E, Dolen I (2008) A randomized comparison of polypropylene mesh surgery with site-specific surgery in treatment of cystocele. Int Urogynecol J Pelvic Floor Dysfunct 19(4):467–471
Richardson AC, Edmonds PB, Williams NL (1981) Treatment of stress urinary incontinence due to paravaginal fascial defect. Obstet Gynecol 57(3):357–362
Shull BL, Baden WB (1989) A six-year experience with paravaginal defect repair for stress urinary incontinence. Am J Obstet Gynecol 160:1432–1440
Bruce RG, El Galley RE, Galloway NT (1999) Paravaginal defect repair in the treatment of female stress urinary incontinence and cystocele. Urology 54(4):647–651
Scotti RJ, Garely AD, Greston WM, Flora RF, Olson TR (1998) Paravaginal repair of lateral vaginal wall defects by fixation to the ischial periosteum and obturator membrane. Am J Obstet Gynecol 179(6 Pt 1):1436–1445
Shull BL, Benn SJ, Kuehl TJ (1994) Surgical management of prolapse of the anterior vaginal segment :an analysis of support defects, operative morbidity, and anatomical outcome. Am J Obstet Gynecol 171:1429–1439
Grody MHT, Nyirjesy P, Kelley LM et al (1995) Paraurethral fascial sling urethropexy and vaginal paravaginal defects cystopexy in the correction of urethrovesical prolapse. Int Urogynecol J Pelvic Floor Dysfunct 6:80–85
Elkins TE, Chesson RR, Videla F et al (2000) Transvaginal paravaginal repair. A useful adjunctive procedure at pelvic relaxation surgery. J Pelvic Surg 6:11–15
Mallipeddi PK, Steele AC, Kohli N, Karram MM (2001) Anatomic and functional outcome of vaginal paravaginal repair in the correction of anterior vaginal wall prolapse. Int Urogynecol J Pelvic Floor Dysfunct 12(2):83–88
Young SB, Daman JJ, Bony LG (2001) Vaginal paravaginal repair: one-year outcomes. Am J Obstet Gynecol 185(6):1360–1366
Benson JT, Lucente V, McClellan E (1996) Vaginal versus abdominal reconstructive surgery for the treatment of pelvic support defects: a prospective randomized study with long-term outcome evaluation. Am J Obstet Gynecol 175(6):1418–1421
Maher CF, Qatawneh A, Dwyer PL, Carey MP, Cornish A, Schluter P (2004) Abdominal sacral colpopexy or vaginal sacrospinous colpopexy for vaginal vault prolapse. A prospective randomized trial. Am J Obstet Gynecol 190:20–26
Raz S, Klutke CG, Golomb J (1989) Four-corner bladder and urethral suspension for moderate cystocele. J Urol 142:712–715
Raz S, Little NA, Juma S, Sussman EM (1991) Repair of severe anterior vaginal wall prolapse (grade IV cystourethrocele). J Urol 146(4):988–992
Gardy M, Kozminski M, DeLancey J, Elkins T, McGuire EJ (1991) Stress incontinence and cystoceles. J Urol 145(6):1211–1213
Benrizi EJ, Volpe P, Pushkar D et al (1996) A new vaginal procedure for cystocele repair and treatment of stress urinary incontinence. J Urol 156(5):1623–1625
Safir MH, Gousse AE, Rover ES, Ginsberg DA, Raz S (1999) 4-defect repair of grade 4 cystocele. J Urol 161:587–594
Dmochowski RR, Zimmern PE, Ganabathi K, Sirls L, Leach GE (1997) Role of the four-corner bladder neck suspension to correct stress incontinence with a mild to moderate cystocele. Urology 49(1):35–40
Goldberg RP, Koduri S, Lobel RW et al (2001) Protective effect of suburethral slings on postoperative cystocele recurrence after reconstructive pelvic operation. Am J Obstet Gynecol 185(6):1307–1312
Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL (1997) Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol 89(4):501–506
Denman MGW, Boyles S, Smith V, Edwards R, Clark A (2008) Reoperation rate 10 years after surgically managed pelvic organ prolapse and urinary incontinence. Am J Obstet Gynecol 198:555
Chmielewski L, Walters MD, Weber AM, Barber MD (2011) Reanalysis of a randomized trial of 3 techniques of anterior colporrhaphy using clinically relevant definitions of success. Am J Obstet Gynecol 205(1):69e1–69e8
Nguyen JN, Burchette RJ (2008) Outcome after anterior vaginal prolapse repair: a randomized controlled trial. Obstet Gynecol 111(4):891–898
Altman D, Falconer C (2007) Perioperative morbidity using transvaginal mesh in pelvic organ prolapse repair. Obstet Gynecol 109(2 Pt 1):303–308
Altman D, Vayrynen T, Engh ME, Axelsen S, Falconer C (2011) Anterior colporrhaphy versus transvaginal mesh for pelvic-organ prolapse. N Engl J Med 364(19):1826–1836
Carey M, Slack M, Higgs P, Wynn-Williams M, Cornish A (2008) Vaginal surgery for pelvic organ prolapse using mesh and a vaginal support device. BJOG 115(3):391–397
Vollebregt A, Fischer K, Gietelink D, van der Vaart CH (2011) Primary surgical repair of anterior vaginal prolapse: a randomised trial comparing anatomical and functional outcome between anterior colporrhaphy and trocar-guided transobturator anterior mesh. BJOG 118(12):1518–1527
Rane A, Iyer J, Kannan K, Corstiaans A (2012) Prospective study of the Perigee system for treatment of cystocele—our five-year experience. Aust N Z J Obstet Gynaecol 52(1):28–33
Carey M, Higgs P, Goh J et al (2009) Vaginal repair with mesh versus colporrhaphy for prolapse: a randomised controlled trial. BJOG 116(10):1380–1386
Maher C, Feiner B, Baessler K, Schmid C (2013) Surgical management of pelvic organ prolapse. Cochrane Database Syst Rev 4:CD004014
Withagen MI, Vierhout ME, Milani AL (2010) Does trocar-guided tension-free vaginal mesh (Prolift) repair provoke prolapse of the unaffected compartments? Int Urogynecol J Pelvic Floor Dysfunct 21(3):271–278
Ward KL, Hilton P (2008) Tension-free vaginal tape versus colposuspension for primary urodynamic stress incontinence: 5-year follow up. BJOG 115(2):226–233
Paraiso MF, Ballard LA, Walters MD, Lee JC, Mitchinson AR (1996) Pelvic support defects and visceral and sexual function in women treated with sacrospinous ligament suspension and pelvic reconstruction. Am J Obstet Gynecol 175(6):1423–1430
Maher CF, Murray CJ, Carey MP, Dwyer PL, Ugoni AM (2001) Iliococcygeus or sacrospinous fixation for vaginal vault prolapse. Obstet Gynecol 98(1):40–44
Moore RD, Mitchell GK, Miklos JR (2012) Single-incision vaginal approach to treat cystocele and vault prolapse with an anterior wall mesh anchored apically to the sacrospinous ligaments. Int Urogynecol J 23(1):85–91
Zyczynski HM, Carey MP, Smith AR et al (2010) One-year clinical outcomes after prolapse surgery with nonanchored mesh and vaginal support device. Am J Obstet Gynecol 203(6):587e1–587e8
Sayer T, Lim J, Gauld JM et al (2011) Medium-term clinical outcomes following surgical repair for vaginal prolapse with tension-free mesh and vaginal support device. Int Urogynecol J 23(4):487–493
Cosson M, Collinet P, Occelli B, Narducci F, Crepin G (2001) The vaginal patch plastron for vaginal cure of cystocele. Preliminary results for 47 patients. Eur J Obstet Gynecol Reprod Biol 95(1):73–80
Groutz A, Chaikin DC, Theusen E, Blaivas JG (2001) Use of cadaveric solvent-dehydrated fascia lata for cystocele repair–preliminary results. Urology 58(2):179–183
Kobashi KC, Leach GE, Chon J, Govier FE (2002) Continued multicenter followup of cadaveric prolapse repair with sling. J Urol 168(5):2063–2068
Powell CR, Simsiman AJ, Menefee SA (2004) Anterior vaginal wall hammock with fascia lata for the correction of stage 2 or greater anterior vaginal compartment relaxation. J Urol 171(1):264–267
Frederick RW, Leach GE (2005) Cadaveric prolapse repair with sling intermediate outcomes with 6 months to 5 years of follow up. J Urol 173(4):1229–1233
Gandhi S, Goldberg RP, Kwon C et al (2005) A prospective randomized trial using solvent dehydrated fascia lata for the prevention of recurrent anterior vaginal wall prolapse. Am J Obstet Gynecol 192(5):1649–1654
Chung SY, Franks M, Smith CP, Lee J-Y, Lu S-H, Chancellor M (2002) Technique of combined pubovaginal sling and cystocele repair using a single piece of cadaveric dermal graft. Urology 59(4):538–541
Clemons JL, Myers DL, Aguilar VC, Arya LA (2003) Vaginal paravaginal repair with an AlloDerm graft. Am J Obstet Gynecol 189(6):1612–1618
Ward RM, Sung VW, Clemons JL, Myers DL (2007) Vaginal paravaginal repair with an AlloDerm graft: long-term outcomes. Am J Obstet Gynecol 197(6):670e1–670e5
Behnia-Willison F, Seman EI, Cook JR, O’Shea RT, Keirse MJ (2007) Laparoscopic paravaginal repair of anterior compartment prolapse. J Minim Invasive Gynecol 14(4):475–480
Simonds RJ, Homberg SD, Hurwitz RL (1992) Transmission of human immunodeficiency virus type 1 from seronegative organ tissue donor. N Engl J Med 326:726–730
Hathaway JK, Choe JM (2002) Intact genetic material is present in commercially processed cadaver allografts used for pubovaginal slings. J Urol 168(3):1040–1043
Leboeuf L, Miles RA, Kim SS, Gousse AE (2004) Grade 4 cystocele repair using four-defect repair and porcine xenograft acellular matrix (Pelvicol): outcome measures using SEAPI. Urology 64(2):282–286
Salomon LJ, Detchev R, Barranger E, Cortez A, Callard P, Darai E (2004) Treatment of anterior vaginal wall prolapse with porcine skin collagen implant by the transobturator route: preliminary results. Eur Urol 45(2):219–225
Gomelsky A, Rudy DC, Dmochowski RR (2004) Porcine dermis interposition graft for repair of high grade anterior compartment defects with or without concomitant pelvic organ prolapse procedures. J Urol 171(4):1581–1584
Wheeler TL 2nd, Richter HE, Duke AG, Burgio KL, Redden DT, Varner RE (2006) Outcomes with porcine graft placement in the anterior vaginal compartment in patients who undergo high vaginal uterosacral suspension and cystocele repair. Am J Obstet Gynecol 194(5):1486–1491
Meschia M, Pifarotti P, Bernasconi F, Magatti F, Riva D, Kocjancic E (2007) Porcine skin collagen implants to prevent anterior vaginal wall prolapse recurrence: a multicenter, randomized study. J Urol 177(1):192–195
Handel LN, Frenkl TL, Kim YH (2007) Results of cystocele repair: a comparison of traditional anterior colporrhaphy, polypropylene mesh and porcine dermis. J Urol 178(1):153–156
Simsiman AJ, Luber KM, Menefee SA (2006) Vaginal paravaginal repair with porcine dermal reinforcement: correction of advanced anterior vaginal prolapse. Am J Obstet Gynecol 195(6):1832–1836
Robles JE, Rioja J, Saiz A et al (2007) Anterior compartment prolapse repair with a hybrid biosynthetic mesh implant technique. Int Urogynecol J Pelvic Floor Dysfunct 18(10):1191–1196
Guerette NL, Peterson TV, Aguirre OA, Vandrie DM, Biller DH, Davila GW (2009) Anterior repair with or without collagen matrix reinforcement: a randomized controlled trial. Obstet Gynecol 114(1):59–65
Hviid U, Hviid TV, Rudnicki M (2010) Porcine skin collagen implants for anterior vaginal wall prolapse: a randomised prospective controlled study. Int Urogynecol J Pelvic Floor Dysfunct 21(5):529–534
Feldner PC Jr, Castro RA, Cipolotti LA, Delroy CA, Sartori MG, Girao MJ (2010) Anterior vaginal wall prolapse: a randomized controlled trial of SIS graft versus traditional colporrhaphy. Int Urogynecol J Pelvic Floor Dysfunct 21(9):1057–1063
Natale F, La Penna C, Padoa A, Agostini M, De Simone E, Cervigni M (2009) A prospective, randomized, controlled study comparing Gynemesh, a synthetic mesh, and Pelvicol, a biologic graft, in the surgical treatment of recurrent cystocele. Int Urogynecol J Pelvic Floor Dysfunct 20(1):75–81
Menefee SA, Dyer KY, Lukacz ES, Simsiman AJ, Luber KM, Nguyen JN (2011) Colporrhaphy compared with mesh or graft-reinforced vaginal paravaginal repair for anterior vaginal wall prolapse: a randomized controlled trial. Obstet Gynecol 118:1337–1344
Fayyad AM, North C, Reid FM, Smith AR (2011) Prospective study of anterior transobturator mesh kit (Prolift) for the management of recurrent anterior vaginal wall prolapse. Int Urogynecol J Pelvic Floor Dysfunct 22(2):157–163
Withagen MI, Milani AL, den Boon J, Vervest HA, Vierhout ME (2011) Trocar-guided mesh compared with conventional vaginal repair in recurrent prolapse: a randomized controlled trial. Obstet Gynecol 117(2 Pt 1):242–250
Colombo M, Vitobello D, Proietti F, Milani R (2000) Randomised comparison of Burch colposuspension versus anterior colporrhaphy in women with stress urinary incontinence and anterior vaginal wall prolapse. BJOG 107(4):544–551
Morse AN, O'Dell KK, Howard AE, Baker SP, Aronson MP, Young SB (2007) Midline anterior repair alone vs anterior repair plus vaginal paravaginal repair: a comparison of anatomic and quality of life outcomes. Int Urogynecol J Pelvic Floor Dysfunct 18(3):245–249
Acknowledgements
This publication results from the work of the Committee on Pelvic Organ Prolapse Surgery, part of the 5th International Consultation on Incontinence, held in Paris in February 2012, under the auspices of the International Consultation on Urological Diseases, and enabled by the support of the European Association of Urology.
The author wishes to acknowledge the fine work of previous consultations led by Professor Linda Brubaker.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
On behalf of Committee 15 “Surgical Management of Pelvic Organ Prolapse” from the 5th International Consultation on Incontinence held in Paris, February 2012
This work has been previously published as: Maher C, Baessler K, Barber M, Cheon C, Deitz V, DeTayrac R, Gutman R, Karram M, Sentilhes L (2013) Surgical management of pelvic organ prolapse. In: Abrams, Cardozo, Khoury, Wein (eds) 5th International Consultation on Incontinence. Health Publication Ltd, Paris, Chapter 15 and modified for publication in International Urogynaecology Journal.
Rights and permissions
About this article
Cite this article
Maher, C. Anterior vaginal compartment surgery. Int Urogynecol J 24, 1791–1802 (2013). https://doi.org/10.1007/s00192-013-2170-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-013-2170-3