Abstract
Introduction and hypothesis
Levator avulsion is associated with prolapse and prolapse recurrence after reconstructive surgery. We set out to determine whether clinical measurement of the genital hiatus and the perineal body (gh + pb) on maximum Valsalva can predict levator avulsion.
Methods
A total of 295 women attending a tertiary referral service underwent 4D translabial ultrasound imaging and clinical examination using the International Continence Society (ICS) Pelvic Organ Prolapse Quantification system (POP-Q). Analysis of ultrasound data sets for levator avulsion was performed using tomographic ultrasound imaging. The predictive performance of gh + pb for avulsion was tested using receiver-operating characteristic curves.
Results
Optimal sensitivity [70 %, 95 % confidence interval (CI) 59–79 %] and specificity (70 %, 95 % CI 66–72 %) were achieved with a cut-off of 8.5 cm for gh + pb.
Conclusions
A gh + pb measurement ≥ 8.5 cm may help to identify women with levator avulsion who are at increased risk of prolapse recurrence.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
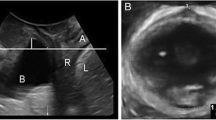
The levator ani plays an important role in supporting the pelvic organs. The part of the levator ani that forms the levator hiatus, the puborectalis muscle, is of particular significance as it defines a potential hernial portal and constitutes a sphincteric mechanism around the urethra, vagina and anorectum [1]. The puborectalis muscle runs from the inferior pubic ramus towards the anorectal junction, surrounding it posteriorly, and back towards the inferior pubic ramus on the contralateral side forming a V-shaped muscle sling (Fig. 1a). Levator avulsion (Fig. 1b), the traumatic disconnection of the puborectalis muscle from its insertion during vaginal childbirth [2–6], is common and has been found to be associated with pelvic organ prolapse (POP) [7, 8] as well as prolapse recurrence, increasing the risk of recurrence by a factor of 2–4 [9, 10]. It has been reported that up to 30 % of all prolapse procedures are performed on recurrent cases [11] highlighting the need to identify predictors of recurrence which can be useful both in preoperative counselling and surgical planning, e.g. concerning the use of mesh for prolapse repair [12]
Several different diagnostic methods have been developed to diagnose levator avulsion. In a study comparing digital palpation, 3D translabial ultrasound imaging using rendered volume and tomographic ultrasound imaging (TUI), the three methods seem to have moderate reproducibility and validity and it was claimed that any of the three methods may be used clinically to diagnose avulsion [13]. However, while digital palpation is simple, it requires substantial training [14]. On the other hand, 3D/4D pelvic floor ultrasound may not be readily available to some clinicians. As we know that levator avulsion is a risk factor for prolapse recurrence [9, 10], it is highly likely that, in future, the indication for certain pelvic reconstructive procedures will require data on the state of the levator ani.
Since the introduction of the Pelvic Organ Prolapse Quantification system (POP-Q) of the International Continence Society (ICS) [15] many clinicians have started to use this method for the description and quantification of POP. The measurements of genital hiatus (gh) and perineal body (pb) on maximal Valsalva are part of this quantification system. The combined measurement of gh + pb has been shown to be associated with ‘ballooning’, i.e. abnormal hiatal distensibility [16]. It is plausible that the same parameter may also be useful to predict levator avulsion as avulsion has been shown to be associated with ballooning [17].
In this study we set out to determine whether levator avulsion can be diagnosed using the measurements of gh + pb using receiver-operating characteristic (ROC) curves. In order to allow comparison with the predictive performance of the sonographic determination of hiatal area on Valsalva, we also measured this sonographic parameter by offline analysis of archived ultrasound data sets.
Methods
All patients seen at a tertiary urogynaecology referral centre for urodynamic testing and 4D transperineal ultrasound imaging between September 2010 and October 2011 were included. A subset of this population (188 of 295) was previously used to test a different hypothesis. Findings have been published elsewhere [16]. All had undergone a standardized interview (local, non-validated), a clinical examination using the ICS POP-Q including measurement of gh + pb on maximal Valsalva [15] (Fig. 2a) as well as transperineal ultrasound with a GE Voluson 730 Expert system (GE Medical Systems, Zipf, Austria) in the supine position after bladder emptying, using an 8-4 MHz curved array transducer. Ultrasound volume data sets were obtained at rest, on maximal Valsalva and on maximal pelvic floor muscle contraction (PFMC) as previously described [18].
Offline analysis of the ultrasound data sets was undertaken by the first author, blinded to clinical data, using proprietary software (4D View, version 5.0, GE Medical Systems). At least three Valsalva manoeuvres were performed by each patient, and the ultrasound volume data set showing the greatest displacement of pelvic organs was used for analysis. Integrity of the puborectalis muscle was assessed using previously validated minimal criteria for the diagnosis of avulsion on TUI using volumes obtained on PFMC, or at rest in patients who were unable to contract. A levator avulsion was rated positive if avulsion of the muscle in the plane of minimal hiatal dimensions as well as 2.5 and 5 mm cranial to this reference plane showed an abnormal insertion or in equivocal cases a levator urethra gap (LUG) of >25 mm [19]. Hiatal area was obtained on maximal Valsalva using a previously described methodology [20] (see Fig. 2 for an illustration).
A test-retest series of 20 assessments was performed by IV and HPD. The results were analysed using Cohen’s kappa and the intraclass correlation coefficient (ICC).
Statistical analysis was undertaken using Minitab V13 (Minitab Inc., State College, PA, USA) for descriptive statistics. Hiatal area on Valsalva and the measurement of gh + pb were tested for normality using histogram analysis. The predictive performance of those parameters for the diagnosis of avulsion was analysed with ROC curves using SPSS V17 (SPSS Inc., Chicago IL, USA). A two-way contingency table analysis (http://statpages.org/ctab2x2.html) was used for relative risks (RR) and odds ratios (OR). The study was approved by the local Human Research Ethics Committee (Sydney West Area Health Service Human Research Ethics Committee reference 11/46).
Results
The data of 295 patients seen between September 2010 and October 2011 were analysed. The mean age was 56.6 years (range 18.6–85.6), median parity was 3 (range 0–10) and mean body mass index (BMI) 29.2 kg/m2 (range 17.3–59.5). The measurement of gh + pb was missing for two patients due to surgical absence of the anus. Patients presented with stress incontinence (75 %, n = 222), urge incontinence (73 %, n = 215), voiding dysfunction such as poor stream, straining to void and/or hesitancy (29 %, n = 87) as well as symptoms of prolapse such as vaginal lump or dragging sensation (53 %, n = 156). Ninety-one per cent (n = 268) had delivered vaginally, and 30 % (n = 89) had one or more deliveries assisted by forceps or ventouse. Twenty-one per cent (n = 62) had undergone previous incontinence or prolapse surgery, and 30 % (n = 90) had a previous hysterectomy. On clinical examination, significant prolapse (ICS POP-Q ≥ stage II) was found in 77 % (n = 227). It was a cystocele in 61 % (n = 171), uterine prolapse in 14 % (n = 25), enterocele in 5 % (n = 16) and rectocele in 56 % (n = 165).
In the test-retest series of 20 patients, the interobserver ICC was 0.903 [95 % confidence interval (CI) 0.696–0.961] for hiatal area on Valsalva. The Cohen’s kappa was 0.892 (95 % CI 0.733–0.961) for the diagnosis of avulsion on tomographic ultrasound, indicating excellent repeatability for both measurement of hiatal area and determination of levator avulsion. The measurements of gh + pb and of hiatal area on Valsalva were normally distributed. Mean gh + pb on Valsalva was 7.9 cm (range 4.2–13). The mean hiatal area on Valsalva was 28.3 cm2 (range 9.7–59.5). Seventy women (24 %) were diagnosed with an avulsion, either unilateral or bilateral, on tomographic ultrasound.
ROC curve analysis showed an area under the curve of 0.769 (95 % CI 0.706–0.833) for the association between gh + pb and the diagnosis of levator avulsion, suggesting that gh + pb is associated with avulsion and can be a useful predictor of this diagnosis. On using ROC curves to describe the predictive performance of gh + pb for avulsion, the optimal sensitivity of 70 % (95 % CI 59–79) and specificity of 70 % (95 % CI 66–72) was achieved with a cut-off of 8.5 cm. The area under the curve for the relationship between hiatal area and avulsion was 0.849 (95 % CI 0.802–0.897), suggesting a stronger relationship. On using ROC curves the optimal sensitivity of 81 % (95 %CI 71–89) and specificity of 73 % (95 % CI 70–75) were obtained with a hiatal area of 30 cm2 as cut-off (see Fig. 3).
Avulsion was substantially more likely in women with gh + pb ≥ 8.5 cm with an OR of 5.32 (95 % CI 2.85–9.98) and RR of 3.51 (95 % CI 2.20–5.72). The corresponding values for a hiatal area on Valsalva ≥ 30 cm2 for the diagnosis of avulsion was 11.64 (95 % CI 5.70–24.15) and 6.5 (95 % CI 3.71–11.94), respectively.
Discussion
In this observational study we compared the predictive performance of clinical examination findings (gh + pb) and sonographic measurement of the levator hiatus on Valsalva for the tomographic diagnosis of levator avulsion. We have been able to show that the measurement of gh + pb on maximal Valsalva is a good predictor for this diagnosis. A cut-off of 8.5 cm has a sensitivity of 70 % and a specificity of 70 %, and an OR of 5.32 for avulsion. A stronger association was found between hiatal area on Valsalva and avulsion. The optimal cut-off is 30 cm2, which has a sensitivity of 81 % and a specificity of 73 %, and an OR of 11.64 for avulsion, confirming previous data showing an association between enlarged hiatal area and this condition [17].
Both ballooning of the hiatus, defined as hiatal area on Valsalva ≥25 cm2 [21], and levator avulsion are independent risk factors for prolapse recurrence [22]. It is therefore of particular interest to determine whether these risk factors can be determined clinically. It has recently been found that ballooning of the levator hiatus can be diagnosed on clinical examination by measuring the gh + pb on maximal Valsalva [16]. We have now been able to show that this clinical finding can also serve to alert the examiner to the likely presence of levator avulsion, which may then be diagnosed either on palpation, if possible, or by using ultrasound or magnetic resonance imaging (MRI).
The diagnosis of avulsion as well as the determination of hiatal distensibility by clinical examination or imaging is likely to become of importance in the assessment of women with prolapse, especially if mesh use is contemplated. It has been shown that women with avulsion are at a greater risk of prolapse recurrence [9, 10], and this effect of avulsion may be partially compensated by mesh [12]. There is growing concern in regard to mesh use and its complications. Consequently, the identification of women at risk of recurrence may help patient selection for mesh repair, justifying the potential risk of mesh complications in a subgroup of women at high risk of prolapse recurrence.
There are a number of limitations of this study that need to be acknowledged. One of the limitations is that the women studied represent a cohort of patients seen in a urogynaecological clinic. The findings of this study therefore may not be generally applicable. However, we believe that it is in a urogynaecological setting that the measurement of gh + pb would be most useful for the prediction of levator avulsion, especially when surgery for prolapse is being considered. The retrospective study design is also a limitation. Clinical measurements and ultrasound volume data were obtained at the same consultation, unblinded to one another, and hence may have introduced bias to the measurement of gh + pb. However, the author who analysed the ultrasound data sets was blinded to all patients’ data, reassuring that the assessment of avulsion and the measurement of hiatal area was not biased by the knowledge of the value of gh + pb, degree of prolapse or other clinical data. It also should be pointed out that by using the measurement of gh + pb alone to diagnose avulsions, an unacceptably large number of patients would be misdiagnosed. On its own this particular test is clearly insufficient to provide an actual diagnosis, requiring confirmation by other means such as palpation or imaging.
In conclusion, the measurement of gh + pb on Valsalva can be used as a clinical predictor of avulsion injury. A measurement ≥ 8.5 cm implies a high risk of this abnormality and allows the identification of women at potentially increased risk of prolapse and prolapse recurrence after corrective surgery. While imaging evidence of hiatal overdistension is more predictive, the clinical measurement of gh + pb is simple and readily available to clinicians with limited access to imaging facilities. A high gh + pb provides an index of suspicion for the diagnosis of avulsion, suggesting either a digital examination or selective imaging to diagnose the condition.
Abbreviations
- MRI:
-
Magnetic resonance imaging
- 4D:
-
Four-dimensional
- ICS POP-Q:
-
International Continence Society Pelvic Organ Prolapse Quantification system
- PFMC:
-
Pelvic floor muscle contraction
- TUI:
-
Tomographic ultrasound imaging
- LUG:
-
Levator urethra gap
- ROC:
-
Receiver-operating characteristic curve
- OR:
-
Odds ratio
- RR:
-
Relative risk
- ICC:
-
Intraclass correlation coefficient
References
Singh K, Reid WM, Berger LA (2002) Magnetic resonance imaging of normal levator ani anatomy and function. Obstet Gynecol 99:433–438
Dietz HP, Lanzarone V (2005) Levator trauma after vaginal delivery. Obstet Gynecol 106:707–712
DeLancey JO, Kearney R, Chou Q, Speights S, Binno S (2003) The appearance of levator ani muscle abnormalities in magnetic resonance images after vaginal delivery. Obstet Gynecol 101:46–53
Lien KC, Mooney B, DeLancey JO, Ashton-Miller JA (2004) Levator ani muscle stretch induced by simulated vaginal birth. Obstet Gynecol 103:31–40
Dietz HP, Steensma AB (2006) The prevalence of major abnormalities of the levator ani in urogynaecological patients. BJOG 113:225–230
Shek KL, Dietz HP (2009) The effect of childbirth on hiatal dimensions. Obstet Gynecol 113:1272–1278
DeLancey JO, Morgan DM, Fenner DE et al (2007) Comparison of levator ani muscle defects and function in women with and without pelvic organ prolapse. Obstet Gynecol 109:295–302
Dietz HP, Simpson JM (2008) Levator trauma is associated with pelvic organ prolapse. BJOG 115:979–984
Weemhoff M, Vergeldt TF, Notten K, Serroyen J, Kampschoer PH, Roumen FJ (2012) Avulsion of puborectalis muscle and other risk factors for cystocele recurrence: a 2-year follow-up study. Int Urogynecol J 23:65–71
Dietz HP, Chantarasorn V, Shek KL (2010) Levator avulsion is a risk factor for cystocele recurrence. Ultrasound Obstet Gynecol 36:76–80
Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL (1997) Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol 89:501–506
Wong V, Shek KL, Goh J, Rane A, Dietz H (2011) Should mesh be used for cystocele repair? Long-term outcomes of a case–control series. Int Urogynecol J 22(Suppl 1):S91
Dietz H, Shek K, Moegni F (2012) Diagnosis of levator avulsion injury: a comparison of three methods. Ultrasound Obstet Gynecol. doi:10.1002/uog.11190
Kearney R, Miller JM, Delancey JO (2006) Interrater reliability and physical examination of the pubovisceral portion of the levator ani muscle, validity comparisons using MR imaging. Neurourol Urodyn 25:50–54
Bump RC, Mattiasson A, Bø K et al (1996) The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol 175:10–17
Khunda A, Shek KL (2012) Can ballooning of the levator hiatus be determined clinically? Am J Obstet Gynecol 206:246.e1–246.e4
Abdool Z, Shek K, Dietz H (2009) The effect of levator avulsion on hiatal dimension and function. Am J Obstet Gynecol 201:89.e1–89.e5
Dietz HP (2004) Ultrasound imaging of the pelvic floor. Part 1: two-dimensional aspects. Ultrasound Obstet Gynecol 23:80–92
Dietz HP, Bernardo MJ, Kirby A, Shek KL (2011) Minimal criteria for the diagnosis of avulsion of the puborectalis muscle by tomographic ultrasound. Int Urogynecol J 22:699–704
Dietz HP, Wong V, Shek KL (2011) A simplified method for determining hiatal biometry. Aust N Z J Obstet Gynaecol 51:540–543
Dietz H, Shek C, De Leon J, Steensma AB (2008) Ballooning of the levator hiatus. Ultrasound Obstet Gynecol 31:676–680
Dietz HP, Franco AV, Shek KL, Kirby A (2012) Avulsion injury and levator hiatal ballooning: two independent risk factors for prolapse? An observational study. Acta Obstet Gynecol Scand 91:211–214
Conflicts of interest
Dr. Volloyhaug has accepted speaker’s fees from Astellas and received travel and congress expenses from Pfizer, travel and course expenses from Johnson and Johnson. Dr. Dietz has, within the last 2 calendar years, acted as a consultant for American Medical Systems (Minnetonka, MN, USA) and Materna Medical Inc. (San Francisco, CA, USA) and has received an educational grant from GE Medical.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Volloyhaug, I., Wong, V., Shek, K.L. et al. Does levator avulsion cause distension of the genital hiatus and perineal body?. Int Urogynecol J 24, 1161–1165 (2013). https://doi.org/10.1007/s00192-012-1993-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-012-1993-7