Abstract
Introduction and hypothesis
The aim of this prospective randomized multicenter study was to compare retropubic tension-free vaginal tape (TVT) with TVT Secur in terms of efficacy and safety.
Methods
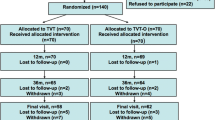
We set out to enrol 280 stress urinary incontinent (SUI) women with a half-time interim analysis of short-term cure and adverse events. The short-term results have previously been published. Of the133 randomized women, 125 underwent surgery, and 121 (TVT n = 61, TVT Secur n = 60) were available for follow-up 1 year postsurgery.
Results
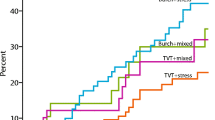
No significant differences were found between groups regarding demographics or incontinence grade. One year after surgery, both subjective and objective cure rates were significantly lower for TVT Secur than for TVT (subjective cure: TVT 98 %, TVT Secur 80 %, p = 0.03; objective cure: TVT 94 %, TVT Secur 71 % for cough test, p = 0.01; TVT 76 %, TVT Secur 58 % for pad test, p = 0.05 ). Three major complications occurred in the TVT Secur group: one tape erosion into the urethra, one tape inadvertently placed into the bladder, and one immediate postoperative bleeding due to injury to the corona mortis. No major complications occurred in the TVT group. No significant differences were found between groups regarding peroperative bleeding, hospital stay, urge symptoms, residual urinary volume, subjective bladder emptying problems, postoperative urinary tract infections, and minor complications. The TVT Secur group used more antimuscarine medication after surgery than the TVT group (p = 0.03). Median time for surgery was 13 and 22 min for TVT Secur and TVT, respectively (p < 0.0001).
Conclusion
The TVT Secur procedure had significantly inferior subjective and objective cure rates compared with the retropubic TVT procedure. Three serious adverse events occurred in the TVT Secur group. We therefore discourage further use of TVT Secur.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Stress urinary incontinence (SUI) affects up to 40 % of women in the Western world, and its prevalence is likely to increase as the population ages [1–3]. Women have a 4 % risk of needing SUI surgery during their lifetime, with nearly one third of surgeries performed due to recurrence [4]. The Burch colposuspension, once the standard technique, has gradually been set aside for less invasive procedures, such as retropubic suburethral polypropylene slings placed under the midurethra [i.e. tension-free vaginal tape (TVT®, Gynecare, Ethicon Inc., Somerville, MA, USA] introduced in 1996 [5]. A transobturator passage of the sling was described by Delorme in 2001 [6]. Subsequently, variations of these methods have been introduced. The efficacy of midurethral slings (MUS) is at least comparable with that of the Burch colposuspension [7]. A 2009 Cochrane Review shows the retropubic route to be slightly more efficacious than the transobturator route but also associated with more complications [8]. However, a large multicenter study by Richter et al. found both routes equally successful for treating SUI [9]. A recent review reports a total complication rate of between 4.3 % and 75.1 % for TVT and between 10.5 % and 31.3 % for transobturator procedures [10]. To reduce the complications associated with blind passage of the needle, the TVT Secur (a single-incision sling device) was introduced in Europe in 2006.
The aim of this study (Suburetral Slings in Southern Sweden, SSISS) was to compare TVT Secur with the retropubic TVT procedure in terms of efficacy and safety in a prospective, randomized setting. According to study protocol, an interim analysis was planned halfway through the study or in case of serious adverse events. Based on interim analysis of the 2-month follow-up data and the reported adverse events [11, 12], we decided to stop further enrolment. We now present the 1-year follow-up data.
Material and methods
Between 2007 and 2009, patients with primary SUI or mixed urinary incontinence (MUI) with predominant SUI symptoms were asked to participate in the study. All women underwent a standardized preoperative investigation, including a 2-day voiding diary, the King’s Health Questionnaire (KHQ), a visual analog scale (VAS) regarding bother due to incontinence, a demographic and contraceptive history, and a detailed incontinence history. Furthermore, a gynecological examination, measurement of residual urine, a cystoscopy, stress test in the upright position, and a standardized short-term pad test, were performed [13]. Inclusion criteria were history of SUI, desire for surgical treatment, no desire for future pregnancy, age ≥18 years, ≥3 ml leakage at a standardized pad-test, cough-synchronous leakage at stress test (up to ten coughs in standing position) the latter two with a bladder volume of 300 ml. The main exclusion criteria were need for concomitant surgery for genital-organ prolapse, regular pelvic floor training begun <3months before inclusion, previous surgery for urinary incontinence, bladder capacity <300 ml, residual urinary volume >100 ml, and known detrusor instability [11].
Consenting women who fulfilled all inclusion criteria were randomized to either retropubic TVT or TVT Secur in a proportion of 1:1. For randomization, an equal proportion of assignments for TVT or TVT Secur were mixed and placed in opaque envelopes, which were then sealed, mixed again, and numbered. They were kept at a central study secretariat that also managed the central study log. Each patient was assigned a research file containing all study protocols marked with an individual file number. All patients gave their written informed consent, and the study was approved by the Regional Institutional Review Board, including approval for all participating centers [11].
A restricted number of surgeons (n = 6), all with previous experience of at least 100 suburethral sling operations and confident with both retropubic and transobturator techniques, was involved. Prestudy training was supervised by one of the authors and consisted pf at least five TVT Secur procedures [11]. All patients were operated on an ambulatory basis following the standard techniques for retropubic TVT and TVT Secur (hammock approach) [11, 14, 15]. Patients were operated on under local anesthesia using a blend of 60 ml 5 % carbocaine–adrenaline and 60 ml saline solution, combined with sedation with fentanyl and propofol i.v.
Postoperative counselling and length of sick leave were standardized and the same for both groups. Patients were discharged within 12 h after surgery if they were able to void spontaneously with residual urine of <100 ml at one measurement or <150 ml at two consecutive measurements. Patients not fulfilling these criteria were discharged with either an indwelling catheter or taught to perform self-catheterization. Residual urine was measured the following day and every second day thereafter until voiding according to the above was achieved.
Follow-up consisted of a standardized telephone interview 2 months postsurgery and an outpatient examination 1 year postsurgery, including pad and stress test in the same manner as presurgery. Patients were encouraged to contact the operating center earlier in case of complications. The follow-up was performed by an independent evaluator, usually a continence nurse. Evaluator blinding was achieved by placing the patient’s operative file and results of randomization in a sealed envelope immediately after surgery and by instructing the patient not to reveal the operative technique at any subsequent follow-up.
Database and statistical analysis
According to the power analysis, the study was designed to detect a 10 % difference in cure rate at an estimated 85 % level of cure and aimed to include 280 patients, with an additional 28 patients to compensate for an estimated 10 % dropout. An interim analysis of cure and complications was planned after 140 included patients or earlier if serious adverse events occurred. Initially, we estimated an approximate equal enrolment among the four participating centers, and therefore, no individual power analysis was undertaken. Two centers were not able to provide sufficient enrolment over time due to change of staff. They were therefore disengaged from further enrolment but continued with follow-up as planned. Thus, the majority of procedures was performed by the remaining two centers. Data were consecutively entered and stored in a central separate computer-based registry (StatView database, SAS Institute Inc., Cary, NC, USA) approved by the Data Registry Board of Skåne University Hospital, Lund. All study files and protocols were collected centrally, and data were entered into the database before the operative technique was revealed during analysis. For the statistical analysis, χ2 test, Wilcoxon’s, Mann–Whitney’ or Kruskal–Wallis test was used, as appropriate. A p value ≤ 0.05 was considered statistically significant.
Results
A total of 133 women were randomized (retropubic TVT n = 69, TVT Secur n = 64) by either of four gynecology departments (A-D) in southern Sweden (A = 71, B = 48, C = 7, D = 7). Of these women, four were excluded due to protocol violations, and another four declined surgery after randomization due to personal reasons. Therefore, 125 women remained and were operated according to the randomization protocol (retropubic TVT n = 63, TVT Secur n = 62). Demographic data showed no statistical difference between groups regarding age, parity ,or body mass index (BMI) (Table 1).
All but two patients (n = 122) underwent surgery with local anesthesia. Median time from patient entry to depart from the operating theater was 58 (range 42–94) min for TVT and 50 (range 27–95) min for TVT Secur (p = 0.0001). Median time for surgery (from beginning of administration of local anesthesia to last suture) and including cystoscopy for TVT patients was 22 (range 13–36) min for TVT and 13 (range 7–25) min for TVT Secur (p < 0.0001). Peroperative bleeding was <25 ml in 63 % and 52 % of TVT and TVT Secur patients, respectively.(p = 0.41). The TVT Secur sling did not need to be reinserted in any patient, and no more than one device was used per procedure. Most patients (78 %) were discharged within 6 h after surgery, with an almost identical distribution between groups. One patient in each group was discharged >24 h after surgery [one due to reoperation because of bleeding from the corona mortis (TVT Secur) and one for social reasons (TVT)]. Two patients in the TVT group had voiding difficulties (>24 h). Both fulfilled voiding criteria within 48 h after surgery. Two patients in the TVT Secur group needed intermittent catheterization for >24 h (2 and 7 days, respectively). No patient experienced permanently obstructed voiding. No tapes needed to be loosened or cut postoperatively.
Six minor peroperative complications were reported: two bladder perforations, both with TVT, two accidental perforations of the vaginal wall beside the incision (one with TVT Secur and one with TVT), and one venous bleeding of about 200 ml with TVT and one between 100 and 200 ml with TVT Secur, both of which were solved with compression . Three major complications occurred, all following the TVT Secur procedure. One patient had an injury of the corona mortis (blood vessel variant, running behind the pubic bone, anastomosing the obturator and external iliac systems), which required immediate surgical reintervention with evacuation of a 1-l retropubic hematoma and vessel ligature [15]. In another patient, tape erosion into the urethra was diagnosed 70 days after surgery. Peroperative cystoscopy was normal in spite of slight hematuria. The patient complained shortly after surgery of intense urgency. After an initial “wait-and-see” period, the sling, which subsequently had eroded further into the urethra, was removed by urethrocystoscopy 22 months after surgery, after which SUI recurred. A retropubic TVT procedure was performed after further 4 months. Two months after the second surgery, the patient was satisfied and had no symptoms of SUI or urge. A third patient presented soon after surgery with recurrent bacteriuria and urgency symptoms. Cystoscopy revealed the distal end of the TVT Secur sling inside the bladder at one side. The intracystic part of the sling was removed by a combined endoscopic and cystoscopic procedure.
Of 125 patients who underwent surgery, 121 were available for long-term follow-up (TVT n = 63, TVT Secur n = 62). Although we aimed for follow-up 12 months after surgery, five women (TVT n = 1, TVT Secur n = 4) were evaluated <6 months after surgery due to self-reported complications or early recurrence; 13 patients (TVT n = 9, TVT Secur n = 4) were evaluated later than 20 months postsurgery due to logistical reasons. Four women were lost to follow-up. At the postoperative follow-up examination [TVT group median 13 months (range 5–29 months), TVT Secur group median 12 months (range 1–27 months, p = 0.20] the subjective cure rate, defined as cured or improved, for SUI symptoms was 98 % for TVT and 80 % for TVT Secur (p = 0.03) (Table 2). The objective cure rates were 94 % for TVT and 71 % for TVT Secur (p = 0.01) according to the no leakage at cough test, and 76 % for TVT and 58 % for TVT S (p = 0.05) according to the no leakage at standardized pad test [13]) (Table 3). Data regarding postoperative urinary tract infections and overactive bladder/de novo urgency are presented in Table 4. No significant differences were found between groups. However, women in the TVT Secur group used more anticholinergics than those in the TVT group (p = 0.03). Neither the residual urinary volume (p = 0.13), nor the subjective sensation of incomplete voiding (p = 0.41) were statistically different between groups. The overall rate for minor complications (dyspareunia, pain, or discomfort; abnormal vaginal discharge) was similar for both groups (TVT = 11 %, TVT Secure 13 %, p = 0.9) (Table 5). Mesh exposure occurred in five patients: two in the TVT and three in the TVT Secur group.
Discussion
In our series, subjective and objective cure of SUI was significantly inferior following TVT Secur than retropubic TVT when evaluated 1 year postsurgery. This association might have even been stronger with study completion, as originally planned. However, due to the interim analysis of cure and the occurrence of three serious adverse events in the TVT Secur group [11], we felt compelled to stop the study prematurely.
We do not believe that the difference in cure rate—in particular, the proportion of uncured and early recurrence patients in the TVT Secur group—can be explained by insufficient surgical skills, as the basics of both procedures are similar. Participating surgeons had broad experience in sling surgery, having performed at least 100 procedures each. Moreover, prestudy training was supervised by one of the authors and aimed to standardize the operative technique before enrolling patients into the study. Different surgical approaches may be more or less “forgiving,” and technique deviations may result in more or less serious adverse events. Increased knowledge of possible differences between methods concerning this matter is one of the reasons for performing this clinical study. Most uncured women in the TVT Secur group reported either a very short or no postoperative effect on their incontinence symptoms, suggesting insufficient sling anchoring. Moreover, our results correspond with previous randomized and nonrandomized publications evaluating the efficacy of TVT Secur. Most of them report lower cure rates for TVT Secur than for retropubic TVT, with rates between 67 % and 80 % [16–33].
Possible causes for the seemingly inferior results of TVT Secur have previously been investigated. Following two studies on cadavers, one showed an anatomically incorrect position of the TVT Secur sling in most cases, regardless of the surgeon’s previous experience [34]. The second showed that the hole in the obturator membrane tended to widen when the inserter was twisted, thus hampering fixation of the distal fleece part of the sling [35]. Martan et al. evaluated 85 SUI patients using perineal ultrasound 1 week and 3 months after a TVT Secur procedure. They concluded that decreased restriction of midurethral mobility 3 months after surgery was a possible cause for the lower cure rate following TVT Secur [26].
A weakness in our study is that some women were not assessed at the postoperative time period originally planned: 11 % were examined later than 20 months postoperatively instead of after 12 months. However, we do not believe this delay to be a major bias, as all these women belonged to the cured group (regardless the device used), and results of the assessment would have been the same had we had the chance to examine/interview them as was intended. Five women were examined much earlier than 12 months postsurgery: four belonged to the TVT Secur group and presented with either serious complications and/or early recurrence, which demanded reoperation. A potential weakness of our study is that we chose not to contemplate the use of validated questionnaires on urinary incontinence, pelvic floor dysfunction, quality of life, or sexual function for postoperative assessment. However, this would have been a main drawback only if the two studied methods had turned out to be equally effective in terms of objective cure of SUI. As TVT Secure was associated with both a significantly lower objective cure rate and three rare, serious complications, we do not believe that additional information provided by those questionnaires would have changed the conclusion of this study.
The main reason, as stated by the manufacturer, for developing TVT Secur was to further reduce complications associated with traditional retropubic or transobturator slings. In our series, three major complications occurred in the TVT Secur group, and other authors have reported bladder perforation, bleeding from the corona mortis, severe bleeding from the internal obturator muscle, injury of the internal pudendal artery, and even male dyspareunia [12, 36–39]. Our results indicate that despite the manufacturer’s recommendation not to perform a urethrocystoscopy following an obturator-membrane-anchored TVT Secur procedure, peroperative bladder and urethral perforation should be ruled out. The fact that one TVT Secur sling inadvertently perforated the bladder, in spite of performing a lateral (hammock) anchoring (as prescribed by study protocol ), indicates that there is no absolute difference between retropubic and obturator anchoring. Therefore, we believe urethrocystoscopy should be routinely performed following placement of TVT Secur slings regardless of the anchoring method chosen. Even minor complications, such as mesh exposure and dyspareunia that is not self-limiting, seem to be more common for TVT Secur [40, 41]. In our series, the occurrence of dyspareunia was low and not significantly different between groups.
In our study, mean time for surgery was 9 min shorter for TVT Secur compared with retropubic TVT patients. We do not believe this compensates for the lower cure rate and complication pattern of the TVT Secur.
Sick leave was prescribed solely based on the patient’s occupation. This study indicates that the TVT Secur procedure may provide weaker anchoring or/and need a longer healing time. Should this demand a longer sick leave in order to achieve similar cure rates to those of retropubic TVT, we believe this disadvantage, by itself, is enough to disqualify TVT Secur.
Conclusion
The main arguments for choosing TVT Secur over TVT (less complications and no need for urethrocystoscopy) are not supported by our data, and would only be valid in a noninferiority situation when compared with TVT. In our study, the subjective cure rate for TVT Secur was significantly lower than for retropubic TVT 1-year postsurgery. This confirms our previous short-term results. Therefore, there is no reason for choosing TVT Secur over TVT, and we think it is important to discourage its further use.
Traditional retropubic and transobturator approaches are well studied, easy to perform, proven to be safe, and have excellent cure rates. Therefore, we believe that suburethral (mini) slings with alternative anchoring techniques should not be introduced to the market without solid evidence ensuring that they bring an actual benefit to the patient.
References
Norton P, Brubaker L (2006) Urinary incontinence in women. Lancet 367:57–67
Hunskaar S, Lose G, Sykes D, Voss S (2004) The prevalence of urinary incontinence in women in four European countries. BJU Int 93:324–330
Hunskaar S, Burgio K, Diokno A, Herzog AR, Hjälmås K, Lapitain MC (2003) Epidemiology and natural history of urinary incontinence in women. Urology 62(Suppl 4):16–23
de Leval J (2003) Novel surgical technique for the treatment of female stress urinary incontinence: transobturator vaginal tape inside-out. Eur Urol 44:724–730
Ulmsten U, Henriksson L, Johnson P, Varhos G (1996) An ambulatory surgical procedure under local anesthesia for treatment of female urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 7:81–86
Delorme E (2001) Transobturator urethral suspension: mini-invasive procedure in the treatment of stress urinary incontinence in women. Prog Urol 11:1306–1313
Ward KL, Hilton P, UK and Ireland TVT Trial Group (2004) A prospective multicenter randomized trial of tension-free vaginal tape and colposuspension for primary urodynamic stress incontinence: two-year follow-up. Am J Obstet Gynecol 190:324–331
Ogah J, Cody JD, Rogerson L (2009) Minimally invasive synthetic suburethral sling operations for stress urinary incontinence in women. Cochrane Database Syst Rev.CD006375
Richter HE, Albo ME, Zyczynski HM, Kenton K, Norton PA, Sirls LT et al (2010) Retropubic versus transobturator midurethral slings for stress incontinence. N Engl J Med 362:2066–2076
Daneshgari F, Kong W, Swartz M (2008) Complications of mid urethral slings: important outcomes for future clinical trials. J Urol 180:1890–1897
Andrada Hamer M, Larsson PG, Teleman P, Etén-Bergqvist C, Persson J (2011) Short-term results of a prospective randomized evaluator blinded multicenter study comparing TVT and TVT Secur. Int Urogunecol J 22:781–787
Larsson PG, Teleman P, Persson J (2010) A serious bleeding complication with injury of the corona mortis with the TVT Secur procedure. Int Urogynecol J 21:1175–1177
Persson J, Eten Bergqvist C, Wølner-Hanssen P (2001) An ultra- short perineal pad-test for evaluation of female stress urinary incontinence treatment. Neurourol Urodyn 20:277–285
Neuman M (2007) TVT Secur: 100 teaching operations with a novel anti-incontinence procedure. Pelviperineology 26:121–127
Molden SM, Lucente VR (2008) New minimally invasive slings: TVT Secur. Curr Urol Rep 9:358–361
Wang Y, Li F, Wang Q, Yang S, Cai X, Chen Y (2011) Comparison of three mid-urethral tension-free tapes (TVT, TVT-O, and TVT Secur) in the treatment of female stress urinary incontinence: 1-year follow-up. Int Urogynecol J 22:1369–1374
Lee KS, Lee YS, Seo JT, Na YG, Choo MS, Kim JC et al (2010) A prospective multicenter randomized comparative study between the U- and H-type methods of the TVT Secur procedure for the treatment of female stress urinary incontinence: 1-Year follow-up. Eur Urol 57:973–979
Khandwala S, Jayachandran C, Sengstock D (2010) Experience with TVT SECUR sling for stress urinary incontinence: a 141-case analysis. Int Urogynecol J Pelvic Floor Dysfunct 21:767–772
Neuman M (2008) Perioperative complications and early follow-up with 100 TVT SECUR procedures. J Minim Invasive Gynecol 15:480–484
Sola V, Ricci P, Pardo J (2009) Third generation sub-mid urethral mesh: experience with 110 TVT Secur. Arch Esp Urol 62:376–388
Tartaglia E, Delicato G, Baffigo G, Signore S, Corvese F, Perla A et al (2009) Third generation tension-free tape for female stress incontinence. J Urol 182:612–615
Oliveira R, Silva A, Pinto R, Silva J, Silva C, Guimarães M et al (2009) Short-term assessment of a tension-free vaginal tape for treating female stress urinary incontinence. BJU Int 104:225–228
Jiménez Calvo J, Hualde Alfaro A, Raigoso Ortega O, Cebrian Lostal JL, Alvarez Bandres S, Jiménez Parra J et al (2008) Our experience with mini tapes (TVT Secur and MiniArc) in the surgery for stress urinary incontinence. Actas Urol Esp 32:1013–1018
Martan A, Svabík K, Masata J, Koleska T, El-Haddad R, Pavlikova M (2008) The solution of stress urinary incontinence in women by the TVT S surgical method. Correlation between the curative effect of this method and changes in ultrasound findings. Ceska Gynekol 73:271–277
Debodinance P, Amblard J, Lucot JP, Cosson M, Villet R, Jacquetin B (2009) TVT Secur: prospective study and follow-up at 1 year about 154 patients. J Gynecol Obstet Biol Reprod 38:299–303
Martan A, Svabík K, Masata J, Koleska T, El-Haddad R, Pavlikova M (2009) Correlation between changes in ultrasound measurements and clinical curative effect of tension-free vaginal tape-SECUR procedure. Int Urogynecol J Pelvic Floor Dysfunct. [DOI 19219379]
Meschia M, Barbacini P, Ambrogi V, Pifarotti P, Ricci L, Spreafico L (2009) TVT-secur: a minimally invasive procedure for the treatment of primary stress urinary incontinence. 1 yeardata from a multi-centre prospective trial. Int Urogynecol J Pelvic Floor Dysfunct 20:313–317
Cornu JN, Sèbe P, Peyrat L, Ciofu C, Cussenot O, Haab F (2010) Midterm Prospective Evaluation of TVT Secur Reveals High Failure Rate. Eur Urol 58:157–161
Lim JL, de Cuyper EM, Cornish A, Frazer M (2010) Short-term clinical and quality-of-life outcomes in women treated by the TVT Secur procedure. Aust N Z J Obstet Gynaecol 50:168–172
Krofta L, Feyereisl J, Velebil P, Otcenásek M, Kasíková E, Krcmár M (2010) TVT S for surgical treatment of stress urinary incontinence: prospective trial, 1-year follow-up. Int Urogynecol J Pelvic Floor Dysfunct 21:779–785
Walsh C (2011) TVT Secur mini-sling for stress urinary incontinence: a review of outcomes at 12 months. BJUI 108:652–657
Chen Y, Wang Y, Li F, Wang Q (2011) Efficacy and postoperative complication of tension-free vaginal tape-Secur for female urinary incontinence. Chin Med J 124:1296–1299
Shin YS, Cha JS, Cheon MW, KimYG KMK (2011) Efficacy and safety of the TVT Secur and impact on the quality of life in women with stress urinary incontinence: a 2-year follow-up. Korean J Urol 52:335–339
Delmas V, Villet R, Debodinance P, Fernandez H, Jacquetin B, Haab F (2008) Where are the extremities of the TVT Secur? Eur Urol Suppl 7:148
Hubka P, Masata J, Nanka O, Grim M, Martan A, Zvarova J (2009) Anatomical relationship and fixation of tension-free vaginal tape Secur. Int Urogynecol J Pelvic Floor Dysfunct 20:681–688
Hubka P, Svabik K, Martan A, Masata J (2010) A serious bleeding complication with injury of the corona mortis with the TVT Secur procedure: two cases of contact of TVT S with the corona mortis during cadaver study. Int Urogynecol J Pelvic Floor Dysfunct 21:1179–1180
Masata J, Martan A, Svabík K (2008) Severe bleeding from internal obturator muscle following tension-free vaginal tape Secur hammock approach procedure. Int Urogynecol J Pelvic Floor Dysfunct 19:1581–1583
Jung YS, Lee JH, Shin TS, Han CH, Kang SH, Lee SY (2010) Arterial injury associated with tension-free vaginal tapes-Secur procedure successfully treated by radiological embolization. Int Neurourol J 14:271–277
Roth TM (2009) An unexpected case of dyspareunia and partner dyspareunia following TVT Secur. Int Urogynecol J Pelvic Floor Dysfunct 20:1391–1392
Álvarez-Bandrés S, Hualde-Alfaro A, Jiménez-Calvo J, Cebrián-Lostal JL, Jiménez-Parra JD, García-García D et al (2010) Complicaciones de la cirugía de incontinencia urinaria femenina con minicintas. Actas Urol Esp 34:893–897
Neuman M, Sosnovsky V, Kais M, Ophir E, Bornstein J (2011) Transobturator vs. single-incision suburethral mini-slings for treatment of female stress urinary incontinence: early postoperative pain and 3-year follow-up. J Minim Invasive Gynecol 18:769–773
Conflicts of interest
This study was performed with economic support from Gynecare Scandinavia. Gynecare had no influence on study design, data interpretation, or content of the article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Andrada Hamer, M., Larsson, PG., Teleman, P. et al. One-year results of a prospective randomized, evaluator-blinded, multicenter study comparing TVT and TVT Secur. Int Urogynecol J 24, 223–229 (2013). https://doi.org/10.1007/s00192-012-1840-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-012-1840-x