Abstract
Objective
The objective is to describe the anatomical localisation of tension-free vaginal tape Secur (TVT-S) in the H-position regarding possible injury of vessels and fixation site.
Methods
We placed TVT-S inserters bilaterally in 14 embalmed and five fresh frozen female bodies. After dissection, we measured distances from the obturator bundle (obturator nerve and obturator vessels).
Results
In embalmed bodies, the mean distance of TVT-S from the obturator bundle was 3.05 cm (standard deviation (SD) 1.18 cm) on the left, 3.07 cm (SD 1.17 cm) on the right. Perforation of the fascia of obturator internus muscle occurred in 46.4%. In fresh frozen bodies, results were fundamentally similar. Injury of variable vessels can occur.
Conclusion
There is a minimal risk of injury to the obturator bundle during TVT-S; however, there is a significant risk of inserting the TVT-S inserter into the obturator fossa. The position of TVT-S does not change significantly after legs mal-positioning.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since its invention by Ulmsten [1] in 1995, the tension-free vaginal tape (TVT) has gained great popularity due to its efficacy [2, 3] and safety, becoming the standard treatment of stress urine incontinence. Nevertheless, complications such as bowel injury [4, 5] and haemorrhage [6, 7] prompted the search for various modifications. It was Delorme [8] who first introduced TVT trans-obturator tape (TOT), which avoided the retro-pubic space and hence minimised the risk of perforation of the urinary bladder. In 2003, de Leval [9] introduced TVT trans-obturator inside-out tape (TVT-O) to further minimise the risk associated with this procedure. The differences between TOT and TVT-O have been described [10–13]. However, TVT-O entails the risk of haemorrhage [14] and damage to the anterior or posterior branch of the obturator nerve, especially when hip joints are in insufficient flexion [15]. A new method of TVT, known as tension-free vaginal tape Secur (TVT-S), aimed to reduce complications and was introduced in 2006. Our first experiences were described by Martan [16–18], showing lower efficacy in comparison with previous TVT procedures.
TVT-S is intended to provide sufficient fixation with less foreign material, reducing the risk of nerve and vessel injury [19, 20]. The surgeon can choose between trans-obturator (hammock) and retro-pubic position (U-shaped). In the hammock position, the tape points with the tip towards to the content of the obturator canal (obturator bundle containing obturator nerve, obturator artery and obturator vein). So far, there has not been any anatomical study focussed on TVT-S, so we decided to investigate anatomical localisation, assess the safety of this method and examine the fixation site of the TVT-S tape in the light of reported haemorrhagic complication during TVT-S [21, 22].
To obtain higher quality photos, we used formalin-embalmed female bodies, and in order to simulate more accurately real-life surgery and decide whether the position of TVT-S changes with the position of the legs during insertion of the tape, we also used fresh frozen bodies.
Materials and methods
We performed TVT-S on 14 formalin-embalmed female bodies at the Institute of Anatomy, First Faculty of Medicine, Charles University in Prague, and on five fresh frozen female bodies at the Institute of Pathology, First Faculty of Medicine, Charles University in Prague. The study complied with Czech and International laws on science and research, and the study was approved by the local ethics committee. The terminology used hereinafter is based on current anatomical terminology (Terminologia Anatomica by FCAT [23]). We have used standard measures derived from the SI measures—centimetres—cm (1/100 m), millimetres—mm (1/1,000 m).
In order to evaluate the risks associated with TVT-S, the surgeon bilaterally inserted TVT-S in the “hammock” position, as described in the standard operation procedure in procedural steps. This means a sagittal incision about 1–1.5 cm was made approximately 1 cm below external urethral meatus, and with a small pair of scissors, two small paraurethral dissections were made approximately 1 cm in length. Using the needle driver, the inserter is inserted into previously dissected paraurethral incisions. The tip is oriented at an angle of 45° from the midline, towards the ischiopubic ramus, while holding the needle driver and inserter so that they are parallel to the floor. The inserter tip will be approximately in the 9 o’clock position. The inserter is advanced, contacting the inferior edge of the pubic ramus. Whilst maintaining contact with the bone, further advance is made into the obturator internus muscle. The same procedure is carried out on the other side. The bodies were positioned as follows: formalin-embalmed bodies—due to the rigidity of the joints—lying on the back with legs in 30° abduction and 30° flexion of hips; fresh frozen bodies lying on the back with legs in gynaecological position (hips in 90° flexion). The surgeon is experienced in various tension-free vaginal tape methods, including TVT-S. During the insertion, he controlled the position of the inserters by palpation, as in standard surgery. The first author afterwards abdominally dissected the bodies. With fresh frozen bodies, we studied whether localisation depends on position of the legs. This was done as follows: After inserting the inserter with the legs in the position recommended by the manufacturer, abdominal dissection takes place. The tip of the inserter is localised and its position measured, and then the inserter is removed, the legs repositioned to 60° of flexion in the hip joint and the inserter inserted as it would be during normal procedure, apart from the position of the legs; the new location was then measured.
The dissector identified the following structures: obturator nerve (nervus obturatorius), obturator artery (arteria obturatoria), obturator vein (vena obturatoria), obturator internus muscle (musculus obturatorius internus), fascia of obturator internus muscle (fascia musculi obturatorii interni), urinary bladder (vesica urinaria). We identified anatomical anomalies that were present.
The position of the TVT-S inserter was described as follows. The shortest distance from the tip of the inserter to the obturator nerve was measured. The obturator bundle containing the obturator artery, vein and nerve is about 3 mm thick; we chose the obturator nerve because it is the most visible and constant structure in the obturator canal. Also, the shortest distance from the tip to the top of the superior ramus of the pubic bone was measured (Fig. 1). To describe localisation of the TVT-S tape in obturator fossa, we used three groups of placement. The first was intramuscular in the obturator muscle (i.e. the tip was deeper than 1 mm from the fascia of obturator internus muscle). This position was considered the correct position (Fig. 2). The distance of 1 mm was chosen because under this value, the inserter was covered by only a few fibres of muscle, which was spread apart, and the tip was already visible underneath the fascia of the obturator internus muscle. The second position was subfascial (i.e. the tip was just underneath the fascia of obturator internus muscle or covered by the muscle to a depth of less than 1 mm). We considered this position as acceptable (Fig. 3). The third position was in the small pelvis (i.e. the tip penetrated the fascia of obturator internus muscle into the small pelvis, the tip was mainly paravesical and subvesical in the obturator fossa—in between the fascia of obturator internus muscle and urinary bladder). We considered this position unacceptable due to possible damage to the bladder veins, bleeding during and after the surgery and damage to the urinary bladder, damage to varicose uterine veins.
Correct position of TVT-S. 1 Pubic symphysis (symphysis). 2 Urinary bladder (vesica urinaria). 3 Uterus (uterus). 4 Left obturator nerve (nervus obturatorius lateris sinistri). 5 Left obturator vein (vena obturatoria lateris sinistri). 6 Left obturator artery (arteria obturatoria lateris sinistri). 7 Left obturator internus muscle (musculus obturatorius internus lateris sinistri). 8 Anastomosis between left obturator vein and external iliac vein (corona mortis venarum). 9 Left internal iliac vein (vena iliaca externa lateris sinistri)
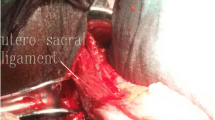
Subfascial placement of the TVT-S with present nutritive vessels for obturator internus muscle. 1 Nutritive vessels for obturator internus muscle (arteria et vena nutritia musculi obturatoris interni). 2 Obturator internus muscle (musculus obturator internus). 3 Obturator fascia (fascia musculi obturatoris interni). 4 Urinary bladder (vesica urinaria). 5 Anastomosis between right obturator artery and deep epigastric artery (corona mortis arteriarum). 6 Right obturatory artery and veins (arteria obturatoria lateris dextri cum venarum obturatoriarum lateris dextri)
The same investigator measured the distances in different stages of the dissection three times and calculated the mean distance. During the dissection, when the tip of inserter could be visualised, the shortest distance was measured to the top of superior ramus of pubic bone and to the obturator bundle. The distances are measured again a short time later, in the same way previously described, in order to lower the risk of personal error during measurement. If the tip was not visible right after exploration of the lesser pelvis, it was located by palpation of the obturator internus muscle and the urinary bladder. The thickness of the tissue covering the inserter was measured as follows: A straight cut through the tissue was made until the inserter was reached. After measuring the thickness of the tissue covering the tip during the cut, the tissue covering the inserter was gently dissected to investigate whether veins or nerves ran through the cut or around the inserter. We documented all the steps involved.
Statistical analysis of data was performed as follows: We calculated means from triples of measured distances. From these data, we estimated mean, variance and standard deviation for the measured distance from obturator bundle at the right and left sides in the group of embalmed bodies and in the group of fresh frozen bodies. Statistical analysis of distance to the obturator nerve was performed based on these factors: difference in position of TVT-S placed in fresh frozen bodies and embalmed bodies, difference in TVT-S placed in fresh frozen bodies with legs in proper position and with legs incorrectly positioned. Statistical comparisons were performed using two sample t test or Mann–Whitney test for differences between groups and Wilcoxon-paired test for differences between left and right side. All statistical tests were performed at the 5% level of significance alpha using statistical system R.
Due to the small number of bodies in both groups, we tried to estimate the number of bodies needed for comparison of mean differences between groups. We used two sample t test, where one group has three times more objects than the other group, approximately. We made a rough estimate of standard deviation SD from given data as 1.3 cm. At a 5% level of significance and with the power of the test 80%, the numbers of fresh frozen bodies and embalmed female bodies needed to detect the mean difference delta are given in Table 1. Therefore, we can see that with the required quality of test results and the number of bodies in our study, we would be able to detect a mean difference of approximately 2 cm. For detection of a mean difference of 0.5 cm, we would need 71 fresh frozen bodies and 214 embalmed female bodies.
Results
We studied 28 trajectories of TVT-S on embalmed bodies and 20 trajectories (ten trajectories of TVT-S with the legs in the proper position and ten trajectories of TVT-S with the legs incorrectly positioned) on fresh frozen bodies. Table 2 lists the distances from the tip of the TVT-S inserter to the obturator nerve, where the mean distance to the obturator nerve on the left side was 3.05 cm (SD 1.18 cm) and 3.07 cm (SD 1.17 cm) on the right on embalmed bodies. The mean position towards the top of ramus superior ossis pubis was 4.48 cm (SD 0.97 cm) on the left and 4.69 cm (SD 0.83 cm) on the right on embalmed bodies.
We obtained fundamentally similar results on fresh frozen bodies: The mean distance to the obturator nerve on the left side was 2.63 cm (SD 1.08 cm) and 2.97 cm (SD 1.43 cm) on the right. The mean position towards the top of ramus superior ossis pubis was 4.30 cm (SD 0.89 cm) on the left and 4.83 cm (SD 1.03 cm) on the right.
The position did not significantly change after incorrectly positioning the legs to 60° flexion in the hips: The mean distance to the obturator nerve on the left side was 2.87 cm (SD 0.91 cm) and 2.83 cm (SD 1.40 cm) on the right. The mean position towards the top of ramus superior ossis pubis was 4.37 cm (SD 0.79 cm) on the left and 4.87 cm (SD 0.91 cm) on the right. However, the distance to the obturator nerve is not the sole parameter according to which we consider the safety of TVT-S.
We measured the position of the TVT-S tape. The nutritive artery for the obturator internus muscle can be seen in Fig. 3, with the tip of the inserter within a very short distance (approximately 5 mm).
The correct position was achieved on embalmed bodies only in nine cases and the acceptable position in six cases (a total of 53.6%). The unacceptable position occurred in 13 cases—46.4%. Results on fresh frozen bodies were as follows: correct position twice, acceptable position also twice—a total of 40%. The unacceptable position occurred in six cases—60%. No change in position happened when the legs were incorrectly positioned and the inserter was reinserted. Injury to the urinary bladder by inserting the inserter into the wall of the bladder or by penetrating into the urinary bladder occurred in four cases from 38 insertions, which is more than 10% of cases.
Statistics showed that when applying the mean, there is no significant difference between fresh frozen bodies and embalmed bodies in the position of the TVT-S to the obturator nerve or to the top of the superior ramus of the pubic bone. Evaluation of the data of TVT-S on fresh frozen bodies with legs in proper position and legs incorrectly positioned only indicated a statistically significant factor (the distance of the inserter to the obturator nerve on the right side) when using t test; because of the small group of bodies, we preferred the Wilcoxon test, which did not prove statistical significance in any group.
Discussion
We have established that TVT-S minimally endangers the obturator bundle and that the position of fixation does not change significantly with changing the position of the legs from 90° to 60°. We also proved that the rate of correct placement is relatively poor in comparison with other TVT methods. The aim of this study was to describe the anatomical location of TVT-S in view of inserting into obturator internus muscle and possible risk of damage to the obturator bundle. We succeeded in indicating possible complications, such as severe bleeding, after this procedure when describing the variable nutritive vein for obturator internus muscle.
There have been some promising results of industry-led research with TVT-S [19], indicating that the short-term failure rate was only 3%, with no complications during 150 operations. On the other hand, there have also been indications from independent researchers that the failure rate can be much higher [17, 18, 24–30]. We recently experienced a case of haemorrhagic complication during TVT-S [22], and others have also reported severe haemorrhage [21]. Faced with the lack of anatomical studies of the location of TVT-S, we searched for a possible explanation of this relatively high failure rate. As we have documented, haemorrhagic complication can be caused by the nutritive artery of the obturator internus muscle (see Fig. 3).
The advantages of using embalmed bodies include better visualisation of the anatomical structures, easier anatomic dissection, more time for studying pelvic floor and steady relative position of the anatomical structures.
The disadvantages are rigidity of the body, with movement in the joints virtually impossible, and fixed position of the anatomical structures, which is more difficult preparation for insertion the tapes. Despite being unable to provide exactly the same conditions as during real surgery, we established on fresh frozen bodies that the trajectory of TVT-S does not significantly change with the position of the legs.
What could be disputed is the immobility of anatomical structures. During real surgery, mobility of structures is possible and therefore risk of injury to the important structures such as the nerves and veins, caused by the tip of TVT-S, could be lower. This also prompted us to use fresh frozen bodies.
In certain cases, where the TVT-S inserter penetrated the fascia of the obturator internus muscle, the operating surgeon sensed a loss of resistance. Although we cannot prove that loss of resistance means perforation of the fascia of the obturator internus muscle, in our opinion, this is the most probable explanation for this sensation.
Perforation of the fascia of the obturator internus muscle cannot really be evaluated in comparison with our clinical experience due to the low rate of severe complications. What we have witnessed several times on ultrasound is that the tape is not fixated and it folds (Fig. 4). This was always accompanied by recurrence of stress urine incontinence. We think that this happens when the fascia is perforated. The inserter was always pointing cranially and laterally, i.e. from the obturator internus muscle towards the fascia of obturator internus muscle, not very parallel with the fascia. Therefore, for the surgeon, it would be just a matter of pushing further (inserting the inserter more than necessary) to penetrate the fascia. It seems to us that using a different shaped inserter, perhaps with a slight bend at the end, could help to fixate the tape laterally back into the obturator internus muscle even in case of perforation of the fascia of obturator internus muscle.
Due to the size of the tip of TVT-S, we feel that the movement of the inserter should be as minimal as possible, so as not to damage the surrounding structures. Excessive movement, shaking or rotation of the tip in case of perforating the fascia would probably tear the crucial fixation point in this case, considering the thin tissue of muscle around it, the tape would probably not hold properly on site. Failure would be the logical outcome.
We cannot agree with the recommendation of the manufacturer to twist, shake or move the inserter tip after positioning it. In cases when the fascia of the obturator internus muscle is perforated, which happened in our study in 46.4% of embalmed bodies and 60% of fresh frozen bodies, excessive movement might enlarge the hole in the fascia, which could in turn reduce fixation; the tip could also tear or puncture veins, as we personally experienced and witnessed during the dissections. In case of perforation of the fascia of obturator internus muscle, haemorrhage from obturator internus muscle will be less likely to stop spontaneously by compression—together with the obturator membrane, the fascia of obturator muscle can be regarded as a compartment.
Perforation of urinary bladder, which occurred in more than 10% of cases in this study, is in striking contrast with our clinical experience, where with 160+ patients who underwent TVT-S in our department, we have had perforation of urinary bladder only once; in other clinical studies, this complication did not occur frequently either. The explanation for this may be that with formalin fixated bodies the urinary bladder, like other tissues, are in steady relative position. Also, during the sole perforation of the urinary bladder in case of fresh frozen bodies, the lesser pelvis was fibrotic and the dissection was difficult.
The success rate of fixation in the obturator internus muscle in this study is almost identical to our success rate of treatment in long-term follow-up after the TVT-S procedure (62%) [18].
The hand preference of the surgeon may explain the different results on the left and right side. We think that a well-experienced surgeon is trained to perform the surgery on both sides with virtually the same outcome. After many operations, the manner of insertion is stable on each side. Statistical analysis also failed to prove significant difference on the right or left side in any of the procedures.
The size of our sample could be questioned; as far as we know, common sizes of similar anatomical studies range from five to ten bodies. We used 14 embalmed bodies and five fresh frozen bodies. Despite using a sample two to four times bigger than usual, for truly valid statistical data, further research needs to be done. As stated under “Material and methods”, hundreds of bodies would be needed to be able to detect a mean difference of 0.5 cm.
Our group is still small, and we would like to investigate further in order to provide more precise statistical data. We would like to also focus in future more on the arterial and venous system in lesser pelvis.
In conclusion, we succeeded in providing an explanation for severe haemorrhagic complications during TVT-S surgery. The course of the inserter is less often confined within the body of the obturator internus muscle than anticipated by the manufacturer, and it often penetrates into the lesser pelvis, thus risking visceral injury. The course of the tape does not seem to change if hip flexion is changed between 60° and 90°.
References
Ulmsten U, Petros P (1995) Intravaginal slingplasty (IVS): an ambulatory surgical procedure for treatment of female urinary incontinence. Scand J Urol Nephrol 29:75–82
Ulmsten U, Johnson P, Rezapour M (1999) A three-year follow up of tension free vaginal tape for surgical treatment of female stress urinary incontinence. Br J Obstet Gynaecol 106:345–350
Nilsson CG, Kuuva N, Falconer C, Rezapour M, Ulmsten U (2001) Long-term results of the tension-free vaginal tape (TVT) procedure for surgical treatment of female stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 12(Suppl 2):S5–S8
Brink DM (2000) Bowel injury following insertion of tension-free vaginal tape. S Afr Med J 90:450, 452
Peyrat L, Boutin JM, Bruyere F, Haillot O, Fakfak H, Lanson Y (2001) Intestinal perforation as a complication of tension-free vaginal tape procedure for urinary incontinence. Eur Urol 39:603–605
Vierhout ME (2001) Severe hemorrhage complicating tension-free vaginal tape (TVT): a case report. Int Urogynecol J Pelvic Floor Dysfunct 12:139–140
Walters MD, Tulikangas PK, LaSala C, Muir TW (2001) Vascular injury during tension-free vaginal tape procedure for stress urinary incontinence. Obstet Gynecol 98:957–959
Delorme E (2001) Transobturator urethral suspension: mini-invasive procedure in the treatment of stress urinary incontinence in women. Prog Urol 11:1306–1313
de Leval J (2003) Novel surgical technique for the treatment of female stress urinary incontinence: transobturator vaginal tape inside-out. Eur Urol 44:724–730
Debodinance P (2007) Trans-obturator urethral sling for the surgical correction of female stress urinary incontinence: outside-in (Monarc) versus inside-out (TVT-O). Are the two ways reassuring? Eur J Obstet Gynecol Reprod Biol 133:232–238
Novara G, Ficarra V, Boscolo-Berto R, Secco S, Cavalleri S, Artibani W (2007) Tension-free midurethral slings in the treatment of female stress urinary incontinence: a systematic review and meta-analysis of randomized controlled trials of effectiveness. Eur Urol 52:663–678
Spinosa JP, Dubuis PY, Riederer BM (2007) Transobturator surgery for female stress incontinence: a comparative anatomical study of outside-in vs inside-out techniques. BJU Int 100:1097–1102
Zahn CM, Siddique S, Hernandez S, Lockrow EG (2007) Anatomic comparison of two transobturator tape procedures. Obstet Gynecol 109:701–706
Rajan S, Kohli N (2005) Retropubic hematoma after transobturator sling procedure. Obstet Gynecol 106:1199–1202
Hinoul P, Vanormelingen L, Roovers JP, de Jonge E, Smajda S (2007) Anatomical variability in the trajectory of the inside-out transobturator vaginal tape technique (TVT-O). Int Urogynecol J Pelvic Floor Dysfunct 18:1201–1206
Martan A, Masata J, Svabik K (2007) TVT SECUR System—tension-free support of the urethra in women suffering from stress urinary incontinence—technique and initial experience. Ceska Gynekol 72:42–49
Martan A, Masata J, Svabik K (2007) Initial experience with TVT-Secur system procedure and the reason for persistent stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 18(Suppl 1):S26–S27
Martan A, Svabik K, Masata J, El-Haddad R, Koleska T, Pavlikova M (2008) Initial experience with TVT-Secur system procedure. Int Urogynecol J Pelvic Floor Dysfunct 19(Suppl 1):S10–S11
Neuman M (2007) Training TVT Secur: the first 150 teaching operations. Int Urogynecol J Pelvic Floor Dysfunct 18(Suppl 1):S27
Rezapour M, Novara G, Meier PA, Holste J, Landgrebe S, Artibani W (2007) A 3-month preclinical trial to assess the performance of a new TVT-like mesh (TVTx) in a sheep model. Int Urogynecol J Pelvic Floor Dysfunct 18:183–187
Araco F, Gravante G, Sesti F, Piccione E (2009) Tension-free vaginal tape Secur hammock procedure: two additional cases of intraoperative bleeding. Int Urogynecol J Pelvic Floor Dysfunct 20:125
Masata J, Martan A, Svabik K (2008) Severe bleeding from internal obturator muscle following tension-free vaginal tape Secur hammock approach procedure. Int Urogynecol J Pelvic Floor Dysfunct 19:1581–1583
FCAT (1998) Terminologia anatomica: international anatomical terminology/FCAT. Thieme, Stuttgart
Albrich S, Naumann G, Skala C, Koelbl H (2007) TVT-SECUR: a novel approach for the treatment of female genuine stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 18(Suppl 1):S25–S26
Debodinance P, Lagrange E, Amblard J, Jacquetin B (2007) TVT SECUR: more and more minimal invasive-preliminary prospective study on 40 cases. Int Urogynecol J Pelvic Floor Dysfunct 18(Suppl 1):S136
Han H, Shukiman I, Lee L (2007) TVT SECUR in treating female stress urinary incontinence: early experience. Int Urogynecol J Pelvic Floor Dysfunct 18(Suppl 1):S184–S185
Karram M, Lucente V, Khandwala S, Nilsson C, Artibani W, Dmochowski R (2007) An evaluation of the Gynecare TVT Secur system (tension-free support for incontinence) for the treatment of stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 18(Suppl 1):S3
Marsh F, Assassa P (2007) An audit of the introduction of TVT Secur in clinical practice. Int Urogynecol J Pelvic Floor Dysfunct 18(Suppl 1):S26
Saltz S, Haff R, Lucente V (2007) Short-term assessment of patients undergoing the new tension free vaginal tape: Secur procedure for treatment of stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 18(Suppl 1):S27–S28
Debodinance P, Lagrange E, Amblard J, Lenoble C, Lucot JP, Villet R et al (2008) TVT Secur: more and more minimally invasive. Preliminary prospective study of 110 cases. J Gynecol Obstet Biol Reprod (Paris) 37:229–236
Acknowledgements
We would like to thank to I. Vítková MD, Chief of Institute of Pathology of the First Faculty of Medicine and General Teaching Hospital, for allowing us to perform research at the Institute of Pathology, for scheduling the dissections and coping with our demands. We would also like to thank to I. Helekal, academic artist of Institute of Anatomy of the First Faculty of Medicine, for drawing Fig. 1. This study was supported by the Internal Grant Agency of the Ministry of Health of the Czech Republic, grant NR/8815-3/2006, GIGH-0651-00-3-223.
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hubka, P., Masata, J., Nanka, O. et al. Anatomical relationship and fixation of tension-free vaginal tape Secur. Int Urogynecol J 20, 681–688 (2009). https://doi.org/10.1007/s00192-009-0815-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-009-0815-z