Abstract
Introduction and hypothesis
Our purpose was to establish the incidence of anal and urinary incontinence 4 years following vaginal delivery in women with and without obstetric anal sphincter injuries (OASIS).
Methods
This was a prospective study of 241 having their first vaginal delivery who had independent verification and repair of OASIS by trained obstetricians. All obstetricians performing OASIS repairs had undergone structured hands-on training and were then directly supervised while repairing OASIS until they were deemed competent to repair independently. Patients were followed up for 4 years with validated bowel and urinary questionnaires. In order to minimise nonresponders, contact details were verified and obtained from their general practitioners, the local primary care trust and electoral roll.
Results
Two hundred and fifty-four women were invited, and 241 (95 %) participated. Fifty-nine (25 %) women sustained OASIS. One hundred and forty-nine were contactable 4 years later, and 86 (58 %) agreed to participate in the study at 4 years. No woman had faecal incontinence, and there was no difference in rates of flatus incontinence prior to delivery up to 4 years postpartum, regardless of whether OASIS occurred or not. Urinary incontinence was more than four times more common after vaginal birth, and this was not affected by whether OASIS occurred and resulted in a significant deterioration in quality of life.
Conclusions
The previously reported higher rates of anal incontinence following OASIS can be minimised up to 4 years after delivery if repaired by trained doctors. There is a significant increase in urinary incontinence following vaginal delivery, and the mechanism for this is not linked to anal sphincter disruption.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anal (AI) and urinary (UI) incontinence are debilitating conditions that affect many women following childbirth. Twenty-one per cent of women are known to have UI within 10 weeks of delivery [1]. The prevalence of stress (SUI) and urge (UUI) incontinence 5 years after first vaginal delivery has been shown to be 30 % and 15 %, respectively [2]. A prospective study comparing women with and without obstetric anal sphincter injuries (OASIS) showed that when there was damage to the anal sphincter, women were significantly more likely to have UI (38 % vs 21.2 %, p = 0.005) [1] up to 3 months following vaginal birth. Five percent of women who have a vaginal delivery have AI [3], and this appears to be higher up to 4 years after vaginal delivery in women who sustain OASIS [4]. Women often avoid seeking professional help due to embarrassment, and therefore, representative data regarding the long-term outcome of these women is lacking [5, 6].
The aim of this study was to establish the incidence of AI and UI four years after childbirth, following accurate diagnosis of perineal trauma.
Materials and methods
Women having their first vaginal delivery between January 2003 and January 2004 at Croydon University Hospital were recruited prospectively. The Manchester Health Questionnaire (MHQ) [7] and the short form of the International Consultation on Incontinence Questionnaire (ICIQ-SF) [8] were completed by participants after recruitment in to the study regarding symptoms prior to having their first vaginal delivery. The MHQ is a validated questionnaire to assess bowel symptoms and was the only available tool at the time the study was conducted. The ICIQ-SF is also a validated questionnaire that assesses urinary symptoms.
Immediately after delivery, all women had a vaginal and rectal examination by a trained research doctor (VA). Perineal trauma was categorised using the Royal College of Obstetricians and Gynaecologists (RCOG) classification [9]. All identified OASIS were repaired by a specialist registrar who had undergone hands-on training in OASIS repair [10] or under the direct supervision of a consultant obstetrician using an evidence-based protocol [11]. Details of this study, including the methodology and demographic data, were previously published [12]. Women were followed up 7 weeks post partum and completed the MHQ and the ICIQ-SF. The same questionnaires were posted to all women 4 years later, and where possible, these women were also contacted by telephone. Nonresponders were sent a second questionnaire 2 weeks later. In order to minimise nonresponders, people who did not respond to the first questionnaire had their contact details verified from their general practitioners, the local primary care trust and electoral roll, where possible. Ethical approval for the study was granted by the Croydon Ethics and Research Committee. Written informed consent was obtained from all participants.
Statistics
Data were analysed using the Statistical Packages for Social Sciences (SPSS, Chicago, IL, USA, version 14.0). To investigate changes in dependent and independent proportions, McNemar and chi-square tests were used, respectively. Unpaired and paired Student’s t tests were used to compare independent and dependent continuous data.
Results
Two hundred and fifty-four women having their first vaginal delivery were invited to participate in the study, and 241 (95 %) agreed. Four years later, 149 women were contactable, of whom 86 (58 %) responded to the questionnaire (see Fig. 1).
There was no difference in demographics, labour characteristics, and symptoms between responders and nonresponders (Table 1). Twenty-five (29 %) of the 86 responders at 4 years sustained OASIS during their first vaginal delivery; 46 of the 86 (53 %) had a subsequent delivery. Of these 46, 15 had an OASIS during their first vaginal delivery, and four were delivered by caesarean section. Of the 31 who had not previously sustained OASIS, two were delivered by caesarean section.
There were no changes in symptoms of AI and quality of life (QoL) at 4 years compared with before delivery or at 7 weeks postpartum in women who did or did not sustain OASIS (Table 2), except for general health perception and emotional impact in women who did not have an OASIS. In addition, sustaining OASIS was not associated with more symptoms of AI or worse QoL when compared with women who had a lesser degree of perineal trauma, except for social and physical limitation scores (Table 3). Four women who had OASIS had subsequent deliveries, only one being delivered by caesarean section.
Symptoms of UI and QoL deteriorated significantly with duration of time following delivery (Table 4), and this was not influenced by sustaining an OASIS (Table 5).
Discussion and conclusion
In this study, symptoms of AI did not change from first vaginal delivery to 4 years, irrespective of whether there was damage to the anal sphincter or not. In addition, there was a fivefold increase in UI 4 years after first vaginal delivery, regardless of whether an OASIS occurred or not, and this also significantly interfered with daily living. Despite anal sphincter rupture being previously described as a major risk factor for subsequent AI, both in the short term (at 1 month) and at >10 years [13, 14], this study did not demonstrate significantly higher rates of AI in women with OASIS than without. In addition, the incidence of AI in women with OASIS (3.6 % at 7 weeks, 16 % at 4 years) was lower than that found in previous studies, which reported symptoms occurred in up to 53 % [15] of women at 3 months and up to 61 % at 4 years [16]. All obstetricians in our study who repaired OASIS had undergone a structured hands-on training course [10], which has been shown to be effective both in imparting knowledge about anal sphincter anatomy and evidence-based methods of OASIS repair (www.perineum.net). In addition to attending the mandatory hands-on course, all trainee obstetricians were directly supervised in OASIS repair until it was felt that they were able to perform them independently.
Previously published studies on OASIS focused mainly on anal symptoms [17, 18]; only a few studies [1, 4, 19, 20] investigated UI. The relationship between UI and OASIS has been conflicting. In a retrospective study using a nonvalidated questionnaire, Wagenius and Lauren [4] reported no difference in urinary symptoms 4 years after OASIS compared with a control group. These findings were confirmed in another study by Otero et al. [21] using a validated questionnaire, which also found no difference in urinary symptoms 18 years after OASIS compared with parity-matched controls. In contrast, Tetzschner et al. [20], in a prospective study of 72 women, reported urinary symptoms in 32 % and demonstrated a relationship with the degree of anal sphincter rupture and UI 4 years after OASIS. In their study, women with a total rupture of the anal sphincter were at greater risk of developing UI. However, symptoms were not evaluated using a validated questionnaire, and there was no control group. Borello-France et al. [22] performed a large prospective short-term study investigating the relationship between anal sphincter injury and postpartum faecal incontinence and UI. They also found no significant difference in the prevalence of UI between the OASIS and control groups. However, there were considerable differences between groups in terms of episiotomy rates, instrumental deliveries, birth weight, and length of labour. Our group previously investigated the relationship between OASIS and UI among 100 women with OASIS and 104 women without OASIS but who had a second-degree perineal tear or episiotomy [1]. Women who had a second-degree tear or episiotomy are included in this study. The two groups were evaluated at 10 weeks post partum, and women with OASIS were significantly more likely to have UI (21.2 vs 38 %, p < 0.01). In addition, women with OASIS were more likely to have stress UI 4 years after delivery (33 % vs 14 %, p < 0.01),and that OASIS was an independent risk factor for developing stress UI.
Our study suggests that UI increases fivefold by 4 years postpartum, regardless of whether there is damage to the anal sphincter or not. An explanation for the difference between our study and that of Scheer et al. [1] and Borello-France et al. [22] may be due to the length of follow-up. Women sustaining OASIS probably have greater damage to the pelvic floor than those with first- and second-degree tears, and this may account for their worse urinary symptoms in the short term. However, with tissue healing and remodelling, OASIS per se may not be an important contributory factor in the development of UI 4 years after delivery.
QoL domains following OASIS were evaluated in this study. Apart from social and physical limitations, none of the other domains was statistically different. Such isolated statistically significant domains are unlikely to be clinically important, we mention it but elaborated no further. This study emphasises that with appropriate repair OASIS repair, QoL is not different to that of other women delivering vaginally.
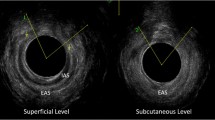
The strengths of our study are that validated questionnaires were used to evaluate bowel and urinary symptoms and QoL measures. The study was prospective, and accurate diagnosis of OASIS was ensured by independent verification. Our study also had a representative control group who could be compared with women who sustained OASIS. In addition, all women had an endoanal scan immediately after delivery and at 3 months postpartum, thus ensuring that none of the control group had occult or unrecognised anal sphincter injuries [12, 23].
The main limitation of our study is that only 36 % of the initial cohort was contactable and willing to participate 4 years after recruitment. This may be in part due to the fact that the population studied were mobile, and many lived in temporary accommodation. Every effort was made to contact nonresponders, many of whom had moved away without updating their hospital or personal records with their general practitioner.
This study demonstrates that AI is not associated with OASIS when doctors who repair anal sphincter injuries receive structured training. The previously high rates of AI following OASIS can be minimised following supervised doctor training. UI increases dramatically following at least one delivery, and the mechanism for this is not associated with damage to the anal sphincter complex 4 years post partum. Further research into the aetiology of UI following vaginal delivery is needed to increase our understanding of the mechanism of the problem so we can attempt to minimise this debilitating condition for women.
References
Scheer I, Andrews V, Thakar R, Sultan AH (2008) Urinary incontinence after Obstetric Anal Sphincter Injuries (OASIS) - Is there a relationship? Int Urogynecol J Pelvic Floor Dysfunct 19:179–183
Viktrup L (2002) The risk of lower urinary tract sypmptoms five years after the first delivery. Neurourol Urodyn 21(1):2–29
Fernando R, Sultan AH, Radley S, Jones PW, Johanson RB (2002) Management of obstetric anal sphincter injury: a systematic review and national practice survey. BMC Health Serv Res 2:9
Wagenius J, Laurin J (2003) Clinical symptoms after anal sphincter rupture: a retrospective study. Acta Obstet Gynecol Scand 82:246–250
Johanson JF, Lafferty J (1996) Epidemiology of fecal incontinence: the silent affliction. Am J Gastroenterol 91:33–36
Hagglund D, Wadensten B (2007) Fear of humiliation inhibits women’s care-seeking behaviour for long-term urinary incontinence. Scand J Caring Sci 21:305–312
Bugg GJ, Kiff ES, Hosker G (2001) A new condition-specific health-related quality of life questionnaire for the assessment of women with anal incontinence. Br J Obstet Gynecol 108:1057–1067
Avery K, Donovan JL, Abrams P (2001) Validation of a new questionnaire for incontinence: the international consultation on incontinence questionnaire (ICI-Q). Neurourol Urodyn 20:86
Royal College of Obstetricians and Gynaecologists (2007) Third- and fourth-degree perineal tears - management. RCOG Press, London, RCOG Guideline No. 29
Andrews V, Thakar R, Sultan AH (2009) Structured hands-on training in repair of obstetric anal sphincter injuries (OASIS): an audit of clinical practice. Int Urogynaecol J 20:193–199
Thakar R, Sultan AH (2003) Management of obstetric anal sphincter injury. Obstet Gynaecol 5(2):72–78
Andrews V, Sultan AH, Thakar R, Jones PW (2006) Occult anal sphincter injuries – myth or reality. Br J Obstet Gynecol 113:195–200
Sander P, Bjarnesen J, Mouritsen L, Fuglsang-Frederiksen A (1999) Anal incontinence after obstetric third-/fourth-degree laceration. One-year follow-up after pelvic floor exercises. Int Urogynecol J 10:177–181
Pinta TM, Kylanpaa ML, Salmi TK et al (2004) Sphincter rupture and anal incontinence after first delivery. Acta Obstet Gynecol Scand 83:917–922
Fitzpatrick M, Cassidy M, O’Connell R, O’Herlihy C (2002) Experience with an obstetric perineal clinic. Eur Jour Obstet Gynecol Reprod Biol 100:199–203
Starck M, Bohe M, Valentin L (2006) The extent of endosonographic anal sphincter defects after primary repair of obstetric sphincter tears increases over time and is related to anal incontinence. Ultrasound Obstet Gynecol 27:188–197
Zetterstrom J, Lopez A, Anzen B, Norman M, Holmstrom B, Mellgren A (1999) Anal sphincter tears at vaginal delivery: risk factors and clinical outcome of primary repair. Obstet Gynecol 94(1):21–28
Uustal Fornell EK, Berg G, Hallbook O, Matthiesen LS, Sjodahl R (1996) Clinical consequences of anal sphincter rupture during childbirth. J Am Coll Surg 183:553–558
Nazir M, Stein R, Carlsen E et al (2003) Early evaluation of bowel symptoms after primary repair of obstetric perineal rupture misleading. Dis Colon Rectum 46(9):1245–1250
Tetzschner T, Sorensen M, Ge L et al (1996) Anal and urinary incontinence in women with obstetric anal sphincter rupture. Br J Obstet Gynecol 103:1034–1040
Otero M, Boulvain M, Bianchi-Demicheli F et al (2006) Women’s health 18 years after rupture of the anal sphincter during childbirth. Urinary incontinence, sexual function, and physical and mental health. Am J Obstet Gynecol 194(5):1260–1265
Borello-France D, Burgio KL, Richter HE et al (2006) Fecal and urinary incontinence in primiparous women. Obstet Gynecol 108:863–872
Sultan AH, Kamm MA, Hudson CN, Thomas JM, Bartram CI (1993) Anal sphincter disruption during vaginal delivery. New Eng J Med 329:1905–1911
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Andrews, V., Shelmeridine, S., Sultan, A.H. et al. Anal and urinary incontinence 4 years after a vaginal delivery. Int Urogynecol J 24, 55–60 (2013). https://doi.org/10.1007/s00192-012-1835-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-012-1835-7