Abstract
Introduction and hypothesis
The objective of the study was to compare extrusion (vaginal mesh exposure) rates in patients undergoing transvaginal prolapse repair with the trocar-based Apogee and/or Perigee devices (American Medical Systems, Minnetonka, MN, USA) using either the original type I polypropylene mesh (IntePro, American Medical Systems, Minnetonka, MN, USA) or a newer generation lightweight type I mesh (IntePro Lite, American Medical Systems, Minnetonka, MN, USA).
Methods
Data were pooled from three similarly designed prospective multicenter studies evaluating the safety and efficacy of Perigee for correction of the anterior (AC) and/or Apogee to repair the posterior/apical (PC/A) compartments. The first two studies utilized IntePro (mesh density 50 g/m2) and the third utilized IntePro Lite (mesh density 25.2 g/m2). Data were pooled to form IntePro and IntePro Lite groups for comparison. Patient demographics were recorded. Risk factors for vaginal mesh exposure were also considered.
Results
Two hundred and sixty-three patients were implanted with Perigee and/or Apogee with IntePro for a total of 371 heavier mesh implants (174 Perigee, 197 Apogee) compared to 86 patients who underwent Perigee and/or Apogee with IntePro Lite for a total of 116 lightweight mesh implants (60 Perigee, 56 Apogee). Demographics and potential risk factors for extrusion were compared between the two groups. Mean follow-up was 2.0 years and similar between the two groups. In the AC, there were 234 implants, with mesh extrusion occurring in 8.0 % following IntePro compared to 5.0 % following IntePro Lite (p = 0.57). In the PA/C, there were 253 implants, with mesh extrusion occurring in 13.7 % following IntePro compared to 7.1 % following IntePro Lite (p = 0.25). Overall mesh extrusion rates in 487 implants in all compartments were found to be 11.1 % with IntePro versus 6.0 % with IntePro Lite with an estimated odds ratio of 1.93 (95 % confidence interval 0.84–4.44, p = 0.12).
Conclusions
No statistically significant difference in extrusion rates were seen following use of IntePro versus IntePro Lite; however, the 46 % reduction in rate of mesh exposure observed in those receiving the lighter weight mesh may represent clinical importance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pelvic organ prolapse (POP) is a significant health issue in females worldwide, with approximately 250,000 procedures performed annually in the USA for POP, with many women having to undergo repeat surgery for failure of previous procedures [1, 2]. Traditional transvaginal correction of vaginal wall defects through native tissue repair relies on the use of compromised connective tissue elements and is likely contributory to variable durability and reoperation rates approaching 30 % [3, 4].
In an attempt to improve outcomes, nonabsorbable synthetic mesh has been employed more commonly in the vagina, with data from the general surgery literature suggesting greater anatomic durability in abdominal wall hernia repairs employing permanent material [5]. The most commonly described permanent synthetic mesh in both the gynecologic and urologic literature is type I [6] polypropylene, which possesses the mechanical properties of durability, elasticity, and resistance [7] in addition to the in vivo characteristics of good tissue integration with minimal inflammatory response [8]. In a number of prospective randomized trials, higher cure rates have been seen in both the anterior and posterior compartments when compared to traditional repairs [9–13]. Additionally, a recent Cochrane review reported higher cure rates in the anterior compartment when mesh was utilized compared to traditional repair [14, 15].
One of the main concerns that has arisen with the common use of transvaginal mesh is that of extrusion (vaginal mesh exposure) and associated adverse events. These events occur in the form of vaginal bleeding, discharge, pain, and/or dyspareunia treated with or without reoperation [16, 17]. Extrusion rates have been reported in the range of 2–25 % in prospective trials [9–12], with a recent randomized clinical trial by Iglesia et al. halted prior to completion secondary to an unacceptably high rate of extrusion [18]. The incidence of vaginal mesh exposure may be impacted by the type of material utilized or the surgical technique employed for placement. Recently, lighter weight meshes have been developed in the hope of decreasing mesh-related complications associated with transvaginal placement.
Our objective was to compare the rate of vaginal mesh extrusion in a cohort of subjects receiving two different types of type I polypropylene in terms of mesh density. Data were pooled from three similarly designed multicenter prospective clinical studies evaluating the safety and efficacy of two trocar-based mesh kits to treat POP. A heavier weight mesh was employed in the first two trials and a lightweight mesh employed in the third. Risk factors for extrusion were also analyzed.
Materials and methods
Study design
Data were collected from three prospective multicenter clinical studies evaluating the safety and efficacy of Perigee and/or Apogee (American Medical Systems, Minnetonka, MN, USA) for correction of the anterior (AC) and the posterior/apical (PC/A) compartments. The PERIGEE Study enrolled subjects with anterior vaginal prolapse utilizing the Perigee® System with IntePro Mesh (study dates April 2005 through January 2009), and the PROPEL Study (Phase I) enrolled subjects with posterior vaginal prolapse and/or apical descent utilizing the Apogee® System with IntePro (July 2006 through October 2009). Phase IV of the PROPEL Study utilized Perigee and/or Apogee with IntePro Lite (April 2007 through May 2010). Concomitant repairs of non-study vaginal wall compartments with the same type of mesh were permitted in each trial allowing for the generation of evaluable data on both devices from all studies. Each had similar protocols, inclusion/exclusion criteria, and data collection such that pooling of data for purposes of examining mesh complications was deemed appropriate. Extrusions were attributed to the appropriate device based on the location of mesh exposure.
IntePro and IntePro Lite mesh are both type I, macroporous, monofilament synthetic grafts. They are made of the same material (polypropylene) and have the same weave (knitted) and large pore size (> 1,000 μm), however vary in density (50 g/m2 versus 25.2 g/m2) and weight secondary to a smaller diameter fiber utilized in IntePro Lite (3/1,000 of an in. versus 4/1,000 of an in.). IntePro Lite is thus softer and more flexible.
All sites received Institutional Review Board approval prior to enrollment. Each investigator was required to have performed a minimum of five Perigee and five Apogee implants prior to participation. Subjects were required to have a diagnosis of symptomatic prolapse ≥ stage II by the Pelvic Organ Prolapse Quantification System (POP-Q) in the compartment undergoing correction and were excluded with any of the following conditions: prior graft augmented repair; systemic or local conditions that would preclude surgery or affect healing such as coagulation disorders, infection, compromised immune response, vaginal bleeding, erosion, tissue necrosis, or uncontrolled diabetes mellitus; and restricted leg motion (inability to conform to the lithotomy position). Additional exclusion criteria included history of pelvic cancer in the previous 6 months, radiation to the pelvic area, pelvic surgery in the previous 6 months, or current participation in another clinical trial.
Data were collected at baseline, procedure, 3 months, 6 months, 12 months, and 24 months. Physical examination of the surgical site was conducted at each visit and mesh extrusions were recorded as to compartment, days to onset, intervention for resolution, and vaginal wall exposure site (PROPEL Study only). Prolapse stage was assessed at baseline, 6 months, 12 months, and 24 months by the same practitioner at each site.
Surgical procedures
Each subject underwent transvaginal placement of IntePro or IntePro Lite by means of bilateral double transobturator trocars for Perigee and bilateral transgluteal trocars for Apogee. Mesh is anchored to the pelvic sidewall via self-fixing appendages (four for Perigee and two for Apogee) and is customizable to the subject’s anatomy and repair requirements by means of mesh trimming. The appendages are constructed of a polypropylene monofilament that is precut to 1.1 cm in width × 23 cm in length and have properties that allow for tissue anchoring and ingrowth. A single polypropylene tensioning suture is prethreaded through the length of each appendage to allow tensioning after placement. Each mesh system is intended to remain in the body as a permanent implant and is not absorbed or degraded by the action of ingrowth or tissue enzymes.
Preoperatively, patients received intravenous antibiotic within 1 h of surgery. The operative technique for Perigee and Apogee was as previously described [19, 20]. In general, a vertical midline incision ≤5 cm in length was employed in both the anterior and posterior compartments. A full-thickness dissection was achieved following infiltration with local anesthetic for both hemostasis and dissection of planes. Little or no trimming of the vaginal muscularis was performed, and closure was with delayed absorbable suture employing a technique at the discretion of the surgeon. Vaginal packing was placed and removed within 12–24 h.
Analyses
Our analysis treated each implant in a different compartment as an independent subject under the assumption that mesh implanted in the anterior compartment (AC) did not interfere with mesh in the posterior/apical compartments (PC/A). The main analysis compared all heavier mesh (IP) implants to lighter softer mesh (IPL) implants. Subgroup analysis was done in two groups: (1) subjects with implants of IntePro mesh in either AC or PC/A and (2) subjects with implants of IntePro Lite mesh in either AC or PC/A.
Anatomic success at 24 months for each subject was calculated using the last failure carried forward (LFCF) method, which carries forward POP-Q failure at previous visits if the 24-month result is missing. The LFCF analysis also considers subjects to be failures if the corresponding compartments were reoperated for recurrent prolapse within 24 months from the initial implant, regardless of the POP-Q measurements. Efficacy for Apogee implant pertains to both posterior and apical compartments while efficacy for Perigee implant pertains to anterior compartment only.
Continuous data were summarized as mean ± standard deviation (SD). Categorical data were reported as count and percent. The two-sample t test was used to compare continuous data between groups. The chi-square or Fisher’s exact test were used to explore differences between groups for categorical data. The logistic regression model was used to estimate the odds ratio of mesh extrusion rate for mesh type and other potential risk factors. A p value < 0.05 was considered statistically significant. Data were analyzed using SAS version 9.2 (Cary, NC, USA).
Results
Three hundred and forty-seven patients were implanted with Apogee and/or Perigee with IntePro or IntePro Lite for a total of 487 implants pooled from the three aforementioned studies conducted at a total of 20 academic and community urogynecologic, urologic, and gynecologic practices in the USA. Two hundred and sixty-three patients were implanted with Perigee and/or Apogee with the original IntePro mesh for a total of 371 heavier mesh implants (174 AC-IP, 197 PC/A-IP) compared to 86 patients that underwent Apogee and/or Perigee with IntePro Lite mesh for a total of 116 lightweight mesh implants (60 AC-IPL, 56 PC/A-IPL).
Demographics and patient characteristics deemed as potential risk factors for extrusion including age, race, parity, body mass index (BMI), prior hysterectomy, prior repair, prolapse stage, estrogen use, and vaginal atrophy factors (vaginal secretion, integrity, thickness, color, and pH) were compared between the two mesh groups. Comparing the overall groups of IP vs IPL mesh, age, BMI, vaginal secretion, vaginal epithelial thickness, and overall prolapse stage were found different in IP vs IPL (Table 1). Age was older, BMI higher, overall prolapse stage greater, and vaginal atrophy factors (secretions and thickness) were more prevalent in the lighter weight IPL group vs the heavier IP. None of these potential risk factors, however, were found to be an independent predictor for vaginal mesh extrusion except for a higher overall baseline prolapse stage (stage III or IV versus II) (Table 2). Mesh extrusion rates can be seen in Table 3. The estimated odds ratio for extrusion for IP versus IPL was 1.93 [95 % confidence interval (CI) 0.84–4.44, p = 0.12] and overall there was a 46 % reduction in extrusion rates with IPL versus IP.
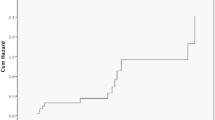
Mean follow-up was 2.0 ± 0.4 in the IP group and 2.0 ± 0.4 years in the IPL group. Extrusion rates and mean time to onset of mesh extrusion are detailed in Table 3 and were not found to be statistically significantly different between IP and IPL by compartment.
Of the 41 IP extrusions, 16 (39 %) were treated in an office setting and 25 of 41 (61.0 %) required intervention in the OR compared to 57.1 % (4/7) of IPL treated in the office and 42.9 % (3/7) requiring OR intervention (p = 0.43). Conservative therapy in the office consisted of estrogen and/or antibiotic therapy with or without trimming of exposed mesh edges. Of the 16 IP extrusions treated in the office, 3 were treated with estrogen cream and/or antibiotics alone and the remaining 13 underwent trimming in the office. All four of the IPL extrusions treated in the office underwent trimming. Intervention in the OR consisted of excising exposed mesh and closure of the epithelial defect. No extrusion or erosion required removal of the central mesh or the entire mesh system. One subject who received Apogee (0.5 %) experienced an erosion of IntePro into the rectum detected 401 days after implant by routine fecal occult blood testing. This event was successfully treated in the OR by transanal trimming of exposed mesh (3 mm) followed by a two-layer closure. Following repair, the subject maintained anatomic success and experienced no further sequelae. There were no other erosions of mesh into the bladder or rectum reported.
Anatomic efficacy at 24 months post surgery defined as POP-Q < stage II using the LFCF method was seen in 86.9 and 87.1 % of the IP and IPL groups, respectively (p = 0.951 chi-square test).
Discussion
The use of transvaginal mesh in the treatment of POP has become more popular in recent years in an effort to achieve greater anatomic success. A number of studies have confirmed higher cure rates in those receiving nonabsorbable synthetic mesh [9–13, 20] as compared to traditional repair; however, complications such as extrusion have led to concerns that such risks outweigh its potential benefit [14, 15, 21]. Sacrocolpopexy, completed abdominally via open incision or laparoscopically, has long been considered the gold standard repair for vaginal vault prolapse and also utilizes mesh placed on the vagina. The procedure is not immune to the same complication of mesh extrusion with rates reported in the range of 1–20 % [22]; however, this seems to be an accepted risk secondary to the benefit of excellent cure rates. Recent studies with the utilization of type I polypropylene mesh for abdominal sacrocolpopexy has shown lower extrusion rates in the range of 0.7–2.3 % [23].
Mesh placed transvaginally for the treatment of prolapse has the advantage of a less invasive approach compared to an abdominal approach, however may run a higher risk of extrusion secondary to having to place the mesh through a vaginal incision. A type I macroporous, monofilament polypropylene has been shown to be the best tolerated permanent material with the lowest rates of extrusion [7]. However, vaginal mesh exposure with first generation heavier type I polypropylene weaves has been as high as 15–20 % [9–13]. Lighter type I polypropylene meshes have been developed to decrease the incidence of such events.
In the current study of 487 mesh implants, the heavier IP extrusion rate of 8.0 % in the AC is consistent with other reports in the literature of similar weight type I meshes [10, 11] as is the 13.7 % observed in the PC/A. The observed lighter weight IPL extrusion rates in the AC and PC/A at 5.0 and 7.1 %, respectively, were lower, however were not found to show a statistically significant difference form those observed in the IP group. The overall rates of mesh extrusion of 11.1 and 6.0 % in the IP and IPL groups, respectively, were also not statistically different, however reasonably represent a clinically significant difference. We also found that the odds of extrusion occurring with the heavier IP mesh were almost twice (1.9 times) that of an occurrence with IPL mesh, again a clinically significant finding. The lighter weight IPL, possessing less density and a smaller fiber diameter, may have incited less of an inflammatory response and perhaps fewer associated extrusions as the resultant overall mesh load is less.
Regarding potential patient characteristics at baseline affecting rates of mesh extrusion, the IPL group was found to be statistically older, had less vaginal secretions and thinner vaginal epithelium (vaginal atrophy factors), and had a higher BMI than the IP group. Perhaps a statistically significant lower extrusion rate would have been observed in the IPL group if the two samples were the same at baseline in regard to such patient characteristics. Although none of these baseline characteristics were found to be independent risk factors for extrusion, we do feel that this provides a measure of credence to the argument that lighter weight mesh is tolerated equally or possibly better than heavier weight mesh given the lower extrusion seen in the IPL population. This also seems to be apparent on physical exam as the softer, lighter mesh is very difficult to feel on exam post-implantation
Extrusions were treated conservatively (vaginal estrogen cream, antibiotics, or trimming in the office) in 39.0 % for IP and 57.1 % for IPL. Those returning to the OR (61.0 % for IP and 42.9 % for IPL overall) for excision were treated by mesh trimming and closure of the wound without major revision or complete mesh explant. It may be that a mesh extrusion that occurs with a lighter, softer mesh (IPL) may have a greater chance of healing with less invasive office treatment compared to a heavier mesh; however, further study with larger numbers is necessary to delineate whether or not this is the case.
Despite the IPL mesh being lighter weight and less dense, there was no difference seen in anatomic efficacy at 24 months between the two groups. This is an important observation as there may be concern that a lighter weight mesh may have reduced strength and higher failure rates; however, we did not find this to be the case in the current comparison.
The strength of this study is the prospective enrollment and collection of data from a large number of subjects with a minimum follow-up of 24 months. Almost 500 mesh implants were evaluated (n = 487) which is one of the largest studies ever reported in the literature regarding vaginal mesh use. The design of the Apogee and Perigee were exactly the same among all three trials, with the only difference being the weight of the mesh utilized. This gave us a very large number of patients to analyze mesh extrusions between the two types of mesh grafts used in both the anterior and posterior compartment as well as overall extrusion rates. Surgical experience and technique undoubtedly has an impact on mesh complications such as extrusion, and this certainly is difficult to study; however, an advantage of this study is that most of the investigators were involved in placement of both types of mesh and therefore this variable should have been somewhat controlled.
Study limitations include the fact that this is a retrospective cohort comparison trial and not a randomized controlled trial, without a predetermined sample size, contributing to a likely underpowered scenario in regard to our primary outcome of relative extrusion rates. Other limitations include the potential biases of the authors and reviewers involved in the trial. Also, the large number of surgeons involved in device implantation, perhaps representing a range of techniques in regard to dissection, wound closure, and different levels of expertise, may affect extrusion rates. Since Perigee and Apogee used in this trial were among the first kits available on the market, enrollment early in the product life cycle versus later enrollment may affect complication rates as opposed to rates seen today in the clinical setting. The last trial evaluating IPL was the most recent; therefore, one could consider that the lower mesh extrusion rates seen may be secondary to surgeon experience and/or techniques. However, a recent trial with the utilization of the same mesh (IPL) in anterior prolapse confirmed low extrusion rates with a 0 % extrusion rate at a mean follow-up of 13.4 months [24]. We were also not able to evaluate possible economic impacts of lower extrusion rates or how much of a reduction would be needed to have a cost-effectiveness impact and therefore this should be studied further in the future.
Conclusion
Vaginal mesh use in POP surgery has become more common secondary to the lower objective cure rates seen with traditional repairs. However, its use must be balanced with complications such as mesh extrusions which may lead to further surgery. Lighter weight, softer type I meshes have been developed in hopes of increasing tolerance and decreasing morbidity, including mesh extrusion. The current study demonstrated improved clinical outcomes with lower rates of vaginal mesh extrusions encountered with the lighter weight IPL mesh compared to the original heavier IP mesh with no difference noted in anatomic efficacy. The reduction in extrusion rates did not meet statistical significance in the current trial; however, multiple factors such as age, weight, prolapse stage, and overall vaginal atrophy and/or the study being underpowered may have impacted the results. Given this, we do feel that the 46 % reduction in extrusion rates seen with the lighter weight mesh is clinically significant. Further studies regarding variable weight meshes and other factors such as surface coatings with antibiotics and/or anti-inflammatory agents need to be considered in the future to improve outcomes and further decrease complications such as extrusions.
Abbreviations
- AC:
-
Anterior compartment
- PC/A:
-
Posterior compartment/apex
- POP:
-
Pelvic organ prolapse
- RCT:
-
Randomized controlled trial
- POP-Q:
-
Pelvic Organ Prolapse Quantification System
- QOL:
-
Quality of life
- OR:
-
Operating room
- IP:
-
IntePro
- IPL:
-
IntePro Lite
References
Beer M, Kuhn A (2005) Surgical techniques for vault prolapse: a review of the literature. Eur J Obstet Gynecol Reprod Biol 119:144–155
Olsen AL, Smith VJ, Bergstrom JO et al (1997) Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol 89:501–506
Maher C, Baessler K (2006) Surgical management of anterior vaginal wall prolapse: an evidence based literature review. Int Urogynecol J Pelvic Floor Dysfunct 17:195–201
Weber AM, Walters MD, Piedmonte MR, Ballard LA (2001) Anterior colporrhaphy: a randomized trial of three surgical techniques. Am J Obstet Gynecol 185:1299–1304, discussion 1304–1306
Burger JW, Luijendijk RW, Hop WC, Halm JA, Verdaasdonk EG, Jeekel J (2004) Long-term follow-up of a randomized controlled trial of suture versus mesh repair of incisional hernia. Ann Surg 240:578–583; discussion 583–585
Amid PK, Lichtenstein IL (1997) Current assessment of Lichtenstein tension-free hernia repair. Chirurg 68:959–964
Cosson M, Debodinance P, Boukerrou M et al (2003) Mechanical properties of synthetic implants used in the repair of prolapse and urinary incontinence in women: which is the ideal material? Int Urogynecol J Pelvic Floor Dysfunct 14:169–178, discussion 178
Boulanger L, Boukerrou M, Lambaudie E et al (2006) Tissue integration and tolerance to meshes used in gynecologic surgery: an experimental study. Eur J Obstet Gynecol Reprod Biol 125:103–108
Hiltunen R, Nieminen K, Takala T et al (2007) Low-weight polypropylene mesh for anterior vaginal wall prolapse: a randomized controlled trial. Obstet Gynecol 110:455–462
Nguyen JN, Burchette RJ (2008) Outcome after anterior vaginal prolapse repair: a randomized controlled trial. Obstet Gynecol 111:891–898
Withagen MI, Milani AL, den Boon J et al (2011) Trocar-guided mesh compared with conventional vaginal repair in recurrent prolapse: a randomized controlled trial. Obstet Gynecol 117(2):242–250
Moore RD, Miklos JR (2009) Vaginal mesh kits for pelvic organ prolapse, friend or foe: a comprehensive review. ScientificWorldJournal 9:163–189
Nieminen K, Hiltunen R, Takala T et al (2010) Outcomes after anterior vaginal wall repair with mesh: a randomized, controlled trial with a 3 year follow-up. Am J Obstet Gynecol 203(3):235.e1–235.e8
Maher C, Baessler K, Glazener CM et al (2008) Surgical management of pelvic organ prolapse in women: a short version Cochrane review. Neurourol Urodyn 27(1):3–12
Maher C, Feiner B, Baessler K, Adams EJ, Hagen S, Glazener CMA (2010) Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev 4:CD004014. doi: 10.1002/14651858.CD004014.pub4
Margulies RU, Lewicky-Gaupp C, Fenner DE et al (2008) Complications requiring reoperation following vaginal mesh kit procedures for prolapse. Am J Obstet Gynecol 199:678e1–678e4
Ridgeway B, Walters MD, Paraiso MF et al (2008) Early experience with mesh excision for adverse outcomes after transvaginal mesh placement using prolapse kits. Am J Obstet Gynecol 199:703e1–703e7
Iglesia CB, Sokol AL, Sokol ER et al (2010) Vaginal mesh for prolapse: a randomized controlled trial. Obstet Gynecol 116(2 Pt 1):293–303
Moore R, Miklos J (2009) Vaginal repair of cystocele with anterior wall mesh via transobturator route: efficacy and complications with up to 3-year followup. Adv Urol 2009:743831
Gauruder-Burmester A, Koutouzidou P, Rohne J et al (2007) Follow-up after polypropylene mesh repair of anterior and posterior compartments in patients with recurrent prolapse. Int Urogynecol J Pelvic Floor Dysfunct 18:1059–1064
Altman D, Falconer C (2007) Perioperative morbidity using transvaginal mesh in pelvic organ prolapse repair. Obstet Gynecol 109(2 Pt 1):303–308
Nygaard IE, McCreery R, Brubaker L (2004) Abdominal sacrocolpopexy: a comprehensive review. Obstet Gynecol 104(4):805–823
Stepanian AA, Miklos JR, Moore RD, Mattox TF (2008) Risk of mesh extrusion and other mesh-related complications after laparoscopic sacral colpopexy with or without concurrent laparoscopic-assisted vaginal hysterectomy: experience of 402 patients. J Minim Invasive Gynecol 15(2):188–196
Moore RD, Mitchell GK, Miklos JR (2012) Single-incision vaginal approach to treat cystocele and vault prolapse with an anterior wall mesh anchored apically to the sacrospinous ligaments. Int Urogynecol J 23(1):85–91
Acknowledgments
The authors would like to thank the investigators for each of the studies reported in this manuscript as follows:
For the PERIGEE Study: Robert D. Moore (P.I.), Roger D. Beyer, Gopal H. Badlani, Karny Jacoby, Enrique G. Jacome, Sheldon J. Freedman, Michael T. Gambla, and Kurt A. McCammon.
For the PROPEL Study: James C. Lukban (P.I.), Ty B. Erickson, Moises A. Virelles, Seth J. Herbst, Manish Patel, Douglas M. Van Drie, Stuart A. Weprin, James Flaherty, Samuel Zylstra, Roger D. Beyer, Robert D. Moore, Robert W. Vera, John N. Nguyen, and Marc A. Hodroff.
Conflicts of interest
Funding for this clinical study was provided by American Medical Systems, Inc. (AMS). R.D. Moore has served as consultant, speaker, and preceptor for AMS. J.C. Lukban has served as consultant, preceptor, facilitator, and speaker for AMS; consultant and speaker for Novasys; and consultant for Coloplast.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Moore, R.D., Lukban, J.C. Comparison of vaginal mesh extrusion rates between a lightweight type I polypropylene mesh versus heavier mesh in the treatment of pelvic organ prolapse. Int Urogynecol J 23, 1379–1386 (2012). https://doi.org/10.1007/s00192-012-1744-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-012-1744-9