Abstract
Introduction and hypothesis
This study aims to analyze comparatively the efficacy and safety of synthetic transobturatory and aponeurotic retropubic slings, in the treatment of stress urinary incontinence (SUI) in women.
Methods
Patients were separated in a randomized way. Twenty-one patients were submitted to the operatory correction by the transobturatory sling technique, whereas 20 patients were operated by the retropubic sling technique. All patients were submitted to complete physical exam and urodynamic test. The “T” test and the Mann–Whitney U test were applied to establish comparisons between the two groups. Patients were followed-up for 12 months.
Results
Healing rate was 90.5% (19/21) and 95% (19/20), respectively after 12 months. The transobturatory group presented lesser complications rate than the retropubic group.
Conclusions
The transobturatory and the aponeurotic slings techniques were equally effective for the treatment of SUI. The transobturatory sling has shown fewer complications and lesser surgical time than the aponeurotic sling technique.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The treatment of stress urinary incontinence (SUI) has been, over the last years, stirring up a great interest from health professionals who work in this area, particularly gynecologists and urologists. This condition affects 15% to 30% of women older than 60 years old. Its incidence is high, turning it into a public health problem, comprising a high socioeconomic cost [1]. Diokno et al. [2] found in 15 to 64 year-old women a prevalence of 25%.
Among several treatments performed over the last decades, the sling technique, mainly the one that is implanted in the mid-urethral region, seems to be the best to correct urinary incontinence and its physiopathological alterations.
The first procedures with aponeurotic slings have their origin in 1907 with Giordano [3], but, only in 1977, McGuire [4] proposed the tension-free slings. Almost two decades after that, in 1995, Petros and Ulmsten [5] revolutionized the surgical treatment of SUI, carrying out the procedures with tension-free slings. In 2001, Delorme [6] proposed a transobturator sling with a bilateral obturator foramen bypass. Finally, Palma [7], in 2002, used the readjustable minimally invasive sling, which is a feasible technique in patients with previous surgeries to urinary stress incontinence treatment and in obese patients.
In obese patients, we know there are inherent problems associated with the patient herself, like sedentary life style, age, hormonal stage, obesity, and concurrent gynecological pathologies [8].
The effects of parity in the pelvic support system have been motivating several studies, mainly regarding the number of pregnancies and the type of delivery [8].
Bezerra [9] systematically reviewed the literature up to December 2004, including quasi-randomized and randomized trials, aiming to determine the consequences of traditional suburethral sling surgeries in patients with stress urodynamic incontinence or mixed incontinence, when compared to other surgical techniques or any other treatment. Only 13 studies were identified as methodologically sound, providing there is no reliable evidence to evaluate if suburethral sling operations are better or worse than other surgery techniques or conservative treatment.
Palma et al. [7], in a multicentric study, compared the self-fixable and adjustable sling under different approaches: vaginal-suprapubical, suprapubical-vaginal, and transobturatory, determining that the last one is effective, simple, and presents no major complications, like vascular and vesical lesions.
Provided that several studies point the adequate efficacy of transobturatory technique but, at the same time, there are few randomized and controlled trials available, more comparative studies are required.
The aim of this work was to analyze comparatively the efficacy and complications of surgery techniques for urinary incontinence correction, using both synthetic transobturator sling and abdominal sling with aponeurotic material.
Materials and methods
Forty-one patients were selected for inclusion from the Centro de Atenção Integral à Saude da Mulher—CAISM (Center for Women’s Health) outpatient clinic in the city of São Bernardo do Campo and from Mario Covas Hospital, in the city of Santo André. The inclusion criteria were stress urinary incontinence (SUI), confirmed through medical history, physical exam, and urodynamic investigation, between April 2004 and October 2005.
The study protocol has been previously submitted to the Institutional Review Board of Faculdade de Medicina do ABC, which approved it with no restrictions.
The physical examination specifically evaluated urinary loss through Valsalva maneuver and the presence of other concurrent dystopias of pelvic floor (anterior, posterior, and apical), using POP-Q classification [10].
The urodynamic study was performed in every patient included in the study according to recommendations from the International Continence Society [11]; Valsalva leak point pressure (VLPP), standardized in this study at 200 mL of vesical repletion. VLPP equal to or lower than 60 cmH20 was compatible with intrinsic sphincter deficiency. Urethral hypermobility was defined as a Q-tip test >30º and VLPP value higher than 60 cmH20.
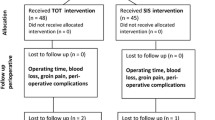
The 41 patients had been randomly distributed in two groups, A and B.
Group A: 21 patients who underwent transobturator sling technique with synthetic material. The material used to this procedure was Safyre-t® (Promedon®, Cordoba, Argentina), consisting of a macroporous and monofilamentous polypropylene mesh, supported by two columns of polydimethylsiloxane.
Group B: 20 patients submitted to abdominal retropubic sling. We used aponeurosis of abdominal rectus muscles of the patient.
In Group A, long-term bladder catheter has been removed in the first postoperatory day. In Group B, it has been removed in the second postoperatory day, due to local trauma and vesical handling resulting from the surgical procedure involving aponeurotic sling.
The discharge from hospital took into account patient’s clinical condition and had been standardized regarding the volume of residual urine in the second or third spontaneous urination. In both groups, this volume has been deemed with a long-term bladder catheter. A volume of residual urine of less than 100 mL or more than 20% of maximum cystometric capacity, based upon previous urodynamic testing, had been used as discharge criteria, dispensing the use of vesical catheterization. In case the residual urinary volume was higher than these settled levels, patients had been discharged with vesical catheter and had been asked to come back in 5 days for a re-evaluation.
Patients had been clinically re-evaluated in the tenth and 30th postoperatory days and 3, 6, and 12 months after surgery to register immediate and late complications. Efficacy analysis was accomplished 1 year after surgery.
The study categorized the results according to efficacy data on the operatory techniques, obtained 1 year after the procedure, as following: cured, improved, failure, and with problems during SUI corrective surgery.
We regarded as cured the patient that, during the 12-month follow-up re-evaluation, reported absence of urinary stress incontinence and that, at the same time, presented no urinary loss during effort maneuvers.
To organize data, the complications had been separated in intraoperatory and postoperatory. Among the first ones, we rated bleeding and urethral or vesical lesions, when demonstrated by cystoscopic examination.
Results
Table 1 shows preoperatory clinical characteristics of patients who underwent SUI surgical correction, using the synthetic transobturator sling or the aponeurotic sling.
Differences between groups´ mean age were not statistically significant. Group A showed an average age of 47 years old, ranging from 31 to 71 years old. The same values for Group B were 52, 31, and 73 years old, respectively.
In addition, there have been no statistically significant differences between groups regarding body mass index (BMI), postmenopause conditions, use of hormone replacement therapy, incidence of genital prolapses, and previous surgeries, particularly hysterectomy.
The mean value for time since onset of SUI was not statistically different between groups. Group A presented an average time of 54 months, varying between 12 and 144 months. Group B values were 45 months in average, ranging from 12 and 120 months.
It is worthy to note there have been two patients in Group A and just one in Group B, who had underwent no previous vaginal births. All study patients have had at least two pregnancies, with an average of 2.5. In Group A, two women had been submitted to surgical treatment for urinary incontinence correction, both using Kelly–Kennedy technique. Moreover, four patients had a history of total abdominal hysterectomy. On the other hand, Group B had three patients who had undergone surgical treatment for urinary incontinence and two with total abdominal hysterectomy.
As seen in Table 2, Group A had 13 patients with urethral hypermobility (UH) and eight with intrinsic sphincter deficiency (ISD). We observed VLPP between 27 and 125 cmH20, using a 200 mL vesical capacity to evaluate urinary loss due to effort maneuvers. Group B had eight patients with UH and 12 with ISD (VLPP between 30 and 139 cmH2O). Vesical instability were absent in both groups. The variables from urodynamic examination were not statistically different in both groups.
The mean value for duration of surgery in Group A corresponded to 13 min, varying from 9 and 20 min, whereas in Group B the mean value was 60 min, ranging from 40 and 80 min (Table 3).
There have been no intraoperatory events in Group A. In Group B, there has been one case of vesical lesion due to passing the needle carrier through the retropubic space. The patient presented a satisfactory clinical evolution and hospital discharge occurred in 48 h. The urinary catheter was removed in the tenth postoperatory day.
No patient presented excessive intraoperatory bleeding. Length of in-hospital stay was 24 and 48 h in Groups A and B, respectively. Mean time of indwelling urinary catheter use and of recovery of spontaneous urination corresponded to 24 h in Group A and to 48 h in Group B.
None of the patients presented fever, postoperatory vaginal bleeding, or intense pelvic pain. One patient from Group B had complete dehiscence of abdominal wall in the ninth postoperatory day, which has been resutured without compromising the suburethral aponeurotic sling.
In Group B, five patients presented serous secretion from the subcutaneous tissue, which had been drained for complete clinical involution. One patient had a skin burn of approximately 5.0 cm resulting from local treatment with hot compresses, with complete involution 3 months after surgery. Abdominal wall hematoma occurred in one patient, with satisfactory clinical evolution only with local treatment. There was one case of abdominal wall infection, treated with antibiotic therapy and presenting complete cure. Two other patients received antibiotic therapy because of urinary infection in the seventh and tenth postoperatory days.
The differences between groups did emerge from the total number of postoperatory complications, with statistically significant predominance of events among patients from Group B.
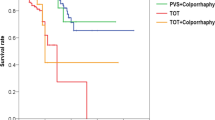
Table 4 indicates the efficacy of methods in Groups A and B.
As we can see, there were no differences regarding the efficacy of both surgical methods for correction of USI. The cure and failure rates of surgical treatment for urinary incontinence were not statistically significant between patients treated with transobturator technique with synthetic material or with abdominal technique with aponeurotic sling.
Discussion
The transobturator approach, as introduced by Delorme [6], proves to have the best cost-benefit ratio to the treatment of UI. Meantime, there are few comparative studies on the other existing techniques to UI correction [9, 12]. The great amount of surgical variables turns this comparison rather unviable. This was one of the reasons to develop this randomized controlled trial of transobturator and retropubic approaches.
The verification of aponeurotic technique was demonstrated by Jarvis [14]. Haab et al. [15] found, in metanalysis studies, cure rates from 73% to 100%.
In our study, the cure rate of patients submitted to aponeurotic sling surgery was 95%, although the follow-up time was 12 months. The follow-up was based on anamnesis and specific physical exam, with Valsalva and cough maneuvers. Patients were considered cured when they reported total dryness.
Tayrac [16] compared, in a prospective and randomized trial, 31 patients who underwent retropubic sling technique and 30 who had the transobturator approach. The author demonstrated that transobturator technique could be as efficient as retropubic technique to the treatment of urinary incontinence in women.
These results are similar to our outcomes, which showed a cure rate of 90.5% in 12 months, without major complications to patients.
Mellier et al. [17], Mansoor [18], and Ansquer et al. [19] retrospectively compared patients submitted to transobturator or retropubic techniques. The authors proved that transobturator approach is effective, safe, and presents less obstructive characteristics than retropubic sling.
In the present study, we tried to show the success characteristics, as well as the events of both surgery techniques. In the aponeurotic sling group, three patients (15%) presented urinary retention in the postoperatory period. One of them (5%) had a vesical perforation and two (10%) had urinary tract infection. The abdominal incision and the need for aponeurotic flap in retropubic technique resulted in seromas (serous secretion), hematomas and suture dehiscence of abdominal wall. In the readjustable transobturator sling participants, there has not been any vesical perforation or urinary tract infection, but two patients (9.5%) presented temporary urinary retention. The rate of complications was significantly lower in the transobturator technique that is corroborated in the literature.
In our study, the inclusion criteria, as well as the previous diagnosis of SUI based on clinical history, physical exam, and complete urodynamic evaluation are in accordance with a relevant multicentric study carried out by Boccon et al. [20], in nine different places. This prospective study assessed 441 patients with SUI, who used non-elastic polypropylene sling. The inclusion criteria were the presence of SUI, urethral hypermobility with or without previous surgery, and presence or absence of associated genital prolapse. Among the 441 patients submitted to transobturator technique, there has been no vascular involvement or nerve or intestinal damages during intra- and postoperatory periods. Thirteen patients (2.9%) presented minor complications as follows: vaginal mucosa perforation due to passing the needle carrier, four urethral perforations, and two vesical perforations. Urinary retention rate was 2%. Authors proved that transobturator sling technique is simple and safe, with a minimally invasive approach. Nevertheless, they emphasized the necessity of randomized controlled trials and longer follow-up periods to determine the real efficacy of the method.
It is worth mentioning that the use of synthetic suburethral slings, the incidence of vagina erosion of polypropylene mesh ranges from 0.2% to 22%, depending on the type of synthetic material utilized [21]. Among the 21 patients who underwent transobturator technique, we noted just one case of erosion in the third postoperatory month (4.76%) in agreement with literature that evaluates monofilamentous polypropylene mesh [13, 20, 22].
Roumeguére et al. [23] and Fisher et al. [24] also observed that transobturator technique is a safe and efficient approach, with low rates of complications. They point out the need for long follow-up periods and bigger samples to make this approach attractive.
Laurikainen et al. [25] compared intra- and postoperatory immediate characteristics of both retropubic and transobturator techniques. The study was randomized and controlled and involved the participation of 273 patients with SUI. It proved that there were no significant differences regarding objective and subjective cure rates. The complications were significantly more common in retropubic approach, what can be explained by the trauma from abdominal and vaginal incisions, as well as by the major risk of vascular, intestinal, and vesical damages resulted by passing the needle carrier.
Although sling readjustment technique is controversial, the use of a self-fixable and readjustable monofilamentous polypropylene mesh make its readjustment possible in two patients who presented recurrent UI. Their clinical history did not involve irritating urinary symptoms or urinary incontinence in postoperatory period. During physical examination, both showed urinary loss induced by Valsalva maneuver, so there was no need to revaluate them with urodynamic tests [26].
This study is in agreement with literature data. The used techniques were safe and efficient and we verified a shorter duration of surgery with transobturator approach, as well as lower complications rate. Thus, transobturator technique, up to now, demonstrated favorable features, which could bring it to gold standard to the treatment of patients with UI, as follows: low complications rate, easy learning and achievement, and good acceptability from doctors and patients.
Conclusion
Self-fixable and readjustable sling technique is efficient in treating stress urinary incontinence and its concurrent accomplishment with other pelvic surgery to correct dystopias is feasible.
When compared to aponeurotic slings, transobturator approach demands significant shorter durations of surgery, besides the fact that a cystoscopy is not necessary and that it results in fewer intra- and postoperatory complications.
References
Thomas TM, Plymat KR, Blannin J et al (1980) Prevalence of urinary incontinence. Br Med J 281:1243–1245
Diokno AC, Brock BM, Brown MB et al (1986) Prevalence of urinary incontinence and other urological symptoms in the noninstitutionalized elderly. J Urol 136(5):1022–1025
Giordano D (1907) In: Twentieth Congress Franc de Chir, Paris.
Mc Guire EJ, Lytton B (1978) Pubovaginal sling procedure for stress incontinence. J Urol 119(1):82–84
Petros P, Ulmsten U (1993) An integral theory and its method for the diagnosis and management of female urinary incontinence. Scand J Urol Nephrol 153:1–93
Delorme E (2001) Transobturator urethral suspension: mini-invasive procedure in the treatment of urinary stress incontinence in women [in French]. Prog Urol 1:1306–1313
Palma PCR, Ricetto CZL, Dambrós M et al (2002) Sling transobturatório: uma nova opção minimamente invasiva para o tratamento da incontinência urinária de esforço. Urodin Uroginecol 5:109–113
Rortveit G, Daltveit AK, Hannestad YS et al (2003) Norwegian EPINCONT Study. Urinary incontinence after vaginal delivery or cesarean section. N Engl J Med 348:900–907
Bezerra CA, Bruschini H (2001) Suburethral sling operations for urinary incontinence in women. Update of: Cochrane Database Syst Rev; 3: CD001754.
Bump RC, Mattiasson A, Bo K, Brubaker LP, DeLancey JOL et al (1996) The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol 175:10–11
Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U et al (2002) The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-Committee of the International Continence Society. Neurourol Urodyn 21:167–178
Kassardjian ZG (2004) Sling procedures for incontinence in women. Brit J Urol 93(5):665–670
Latthe PM, Foon R, Toozs-Hobson P (2007) Transobturator and retropubic tape procedures in stress urinary incontinence: a systematic review and meta-analysis of effectiveness and complications. BJOG 114:522–531
Jarvis GJ (1994) Surgery for genuine stress incontinence. Br J Obstet Gynaecol 101(5):371–374
Haab F, Zimmern PE, Leach GE (1996) Female stress urinary incontinence due to intrinsic sphincteric deficiency: recognition and management. J Urol 156(1):3–17
de Tayrac R, Deffieux X, Droupy S et al (2004) A prospective randomized trial comparing tension-free vaginal tape and transobturator suburethral tape for surgical treatment of stress urinary incontinence. Am J Obstet Gynecol 190(3):602–608
Mellier G, Benayed B, Bretones S et al (2004) Suburethral tape via the obturator route: is the sling transobturator a simplification of the sling retropubic? Int Urogynecol J 15:227–232
Mansoor A et al. (2003) 33rd Annual Meeting of the International Continence Society—Conference Abstract 88.
Ansquer Y, Marcollet A, Yazbeck C, Salomon L, Poncelet C et al (2004) The suburethral sling for female stress urinary incontinence: a retropubic or obturator approach? J Am Assoc Gynecol Laparosc 11(3):353–358
Boccon GL, Grise P, de tayrac R, Costa P, Monneins F et al. (2004) Trans-Obturator Tape (TOT) for the treatment of female stress urinary incontinence: a multicentric prospective study. Program and abstracts of the International Continence Society and IUGA Annual Meeting, Paris, France. Abstract 311
Deval B, Haab F (2006) Management of the complications of the synthetic slings. Curr Opin Urol 16(4):240–243
Mellier G, Moore R, Jacquetin B (2004) A meta-analysis of the intra-operative safety and effectiveness of the transobturator hammock seen in results of two prospective studies in 9 countries with 204 patients. Program and abstracts of the International Continence Society Annual Meeting Aug 25-27, Paris, France. Abstract 113.
Roumeguere T, Quackels T, Bollens R, de Groote A, Zlotta A, Bossche MV et al (2005) Trans-obturator vaginal tape (TOT) for female stress incontinence: one year follow-up in 120 patients. Eur Urol 48(5):805–809
Fisher A, Fink T, Zachmann S, Eickenbusch U (2005) Comparison of retropubic and outside-in transobturator sling systems for the cure of female genuine stress urinary incontinence. Eur Urol 48:799–804
Laurikainen E, Valpas A, Kivela A, Kalliola T, Rinne K, Takala T et al (2007) Retropubic compared with transobturator tape placement in treatment of urinary incontinence: a randomized controlled trial. [Comparative Study—Journal Article. Multicenter Study. Randomized Controlled Trial]. Obstet Gynecol 109(1):4–11
Tcherniakovsky M, Del Roy CA, Paramo GL et al (2006) Surgical Treatment for Stress Urinary Incontinence of Transobturator Approuch: Outcomes with Safyre-t ™. Femina 7(34):477–482
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tcherniakovsky, M., Fernandes, C.E., Bezerra, C.A. et al. Comparative results of two techniques to treat stress urinary incontinence: synthetic transobturator and aponeurotic slings. Int Urogynecol J 20, 961–966 (2009). https://doi.org/10.1007/s00192-009-0880-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-009-0880-3