Abstract
This article reviews sexual function questionnaires used in urogynecology, impact of pelvic floor dysfunction (PFD) on sexual function, and impact of surgical treatment of PFD on sexual function, with a focus on the experience and publications of validated sexual function questionnaires in the urogynecologic literature. A review of the literature was performed to obtain data on sexual function and PFD focusing on those studies that utilized validated sexual function questionnaires. Validated questionnaires assure data that are reliable, quantifiable, and reproducible. Quality-of-life questionnaires, such as The King’s Health Questionnaire and the Incontinence Impact Questionnaire, include a few questions addressing sexual function but really deal with the overall impact of incontinence and/or prolapse on the patient’s QOL or well-being and do not focus on sexual function. General questionnaires focused on sexual function include the Female Sexual Function Index and the Sexual History Form 12, which were designed to evaluate sexual function and have undergone validation and reliability testing in a general population. General questionnaires are not condition-specific and may not be sensitive enough to detect differences due to PFD. The Pelvic Organ Prolapse Urinary Incontinence Sexual Questionnaire (PISQ) is a condition-specific questionnaire focused on sexual function for use in women with PFD and has undergone rigorous validation and reliability testing. Many recent publications examining the impact of urinary incontinence (UI), fecal incontinence, and pelvic organ prolapse (POP) using validated generalized and disease-specific questionnaires have reported poorer sexual function in women with PFD. The PISQ has been used most commonly to evaluate sexual function after surgery for PFD, with increased PISQ scores in approximately 70%. Significant improvement is noted for sexual function related to physical and partner-related factors, with no changes for orgasm, desire, or arousal after surgical repair of PFD. Studies which used generalized sexual function questionnaires mainly found no change in sexual function following surgical treatment of POP and/or UI. In summary, the use of validated questionnaires shows that PFD is associated with a negative impact on sexual functions. Surgical correction of POP and/or UI improves sexual function in approximately 70% of patients, although some studies show no change with the use of non-condition-specific questionnaires.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
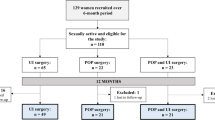
Pelvic floor dysfunction (PFD), including pelvic organ prolapse (POP) and urinary and fecal incontinence (UI, FI), is quite common, effecting approximately 50% of women, with 11% undergoing surgical treatment for these disorders [1–3]. Sexual function may be adversely effected by these problems, although the data regarding this association are conflicting [4, 5]. Older publications examining the relationship between pelvic floor dysfunction, as well as the effects of its treatment on female sexual function, have been limited by the use of nonvalidated and non-condition-specific questionnaires or not controlling for confounding variables including age and menopausal status. This article will review questionnaires utilized to assess sexual function in urogynecology, the impact of PFD on sexual function, and the impact of surgery for PFD on sexual function.
Questionnaires to assess sexual function in women with pelvic floor disorders
Validated questionnaires utilized to assess sexual function in women with PFD may be generalized or condition-specific. Generalized questionnaires focusing on sexual function were designed to evaluate sexual function in a general population and not specifically in women with PFD. These types of questionnaires may not be sensitive enough to detect differences due to the disease process of UI, FI, and/or POP in this specialized population. Two general questionnaires focused on sexual function that have been utilized in the urogynecologic literature include the Sexual History Form 12 (SHF-12) and the Female Sexual Function Index (FSFI). The SHF-12 is a shortened version of a 24-item questionnaire that was developed by telephone survey of married couples in New York [6]. The FSFI was developed by a multidisciplinary group of experts in female sexual dysfunction (FSD) with question selection and domain categories based on the American Foundation for Urologic Disease classification of FSD (female sexual arousal disorder, hypoactive sexual desire disorder, female sexual orgasmic disorder, and female sexual pain disorder) [7]. The FSFI consists of a 19-item survey assessing six domains of FSD and emphasizes the domain of Female Sexual Arousal Disorder which was divided into two separate domains of lubrication and arousal to assess both the peripheral (lubrication) and central (subjective arousal and desire) components. Scores range from 2 to 36.0, with a total score of 26 or less suggestive of FSD and individual domain scores of less than 3.6 abnormal [8]. The FSFI has been validated based on Diagnostic and Statistical Manual of Mental Disorders IV (DSM-IV) diagnoses of female sexual dysfunctions including hypoactive sexual desire disorder, female sexual arousal disorder, and female sexual orgasmic disorder [9].
Other questionnaires such as the King’s Health Questionnaire and the Incontinence Impact Questionnaire have a few questions addressing sexual function but really deal with the overall impact of incontinence and/or prolapse on the patient’s quality of life and well being [10, 11]. These questionnaires are condition-specific and were developed, validated, and tested for use in women with PFD but do not focus on sexual function. They have undergone extensive validation and reliability testing.
There are two condition specific questionnaires focused on sexual function for use in women with PFD, the Pelvic Organ Prolapse Urinary Incontinence Sexual Questionnaire (PISQ), and the International Consultation on Incontinence Questionnaire Vaginal Symptoms (ICIQ-VS) [12, 13]. The ICIQ-VS has undergone construct validity and reliability testing to establish internal validity but has not undergone external validation. Besides the original publication, the ICIQ-VS has only been utilized in a recent publication for validation in Portuguese [14].
The original long form of the PISQ has 31 questions and contains three domains: behavioral-emotive, physical, and partner-related. The behavioral-emotive domain measures the frequency of sexual activity, the desired frequency, orgasm rates, and satisfaction with one’s sexual relationship. The physical domain examines episodes of pain, incontinence, sensation of prolapse, and fear of fecal and/or urinary incontinence during sexual activity. The partner-related domain includes any difficulty with erectile dysfunction, premature ejaculation, vaginal attenuation, vaginal tightness, or the patient’s perception of a partner’s avoidance of intercourse. The PISQ has undergone criterion or construct validity and external validation, with high correlation between PISQ and SHF-12 and Incontinence Impact Questionnaire-7 scores. Additionally, the PISQ was able to distinguish between women with and without high depression scores on the Symptom Questionnaire, with depression associated with, and an alternative of, poor sexual function. Reliability testing and internal consistency is good to excellent, with Chronbach’s α ≥ 0.85 and test–retest reliability κ = 0.56–0.93. The PISQ utilizes a Likert scale with 0 = never and 4 = always, with reverse scoring used on some questions to consistently reflect that higher scores equal better sexual function with a maximal score of 124 possible. Normative scores were not established in the original questionnaire development, but the mean score in a healthy population used to validate the questionnaire was 94 [12]. A short form of the PISQ has also been validated and contains 12 questions (PISQ-12) [15]. The PISQ-12 has a maximal score of 48 and can be converted to PISQ Long Form scores when multiplied by 2.58.
The PISQ has also been validated Portuguese and Spanish, both in America and Spain [16, 17]. A recent Medline search noted 27 publications utilizing the PISQ not including abstracts or other citations, furthering the validation process. The PISQ was recently utilized in a general population of twins to evaluate for sexual dysfunction and establish normative values [18]. The PISQ-12 scores highly correlated with scores of a general sexual-function questionnaire and were significantly lower in women with depressive symptoms or pain of bladder origin. These findings suggest that PISQ-12 may be reliably used in a general population without PFD. The mean PISQ-12 score in their population of sexually active women without bothersome POP or UI was 40.
The impact of pelvic floor dysfunction on sexual function
In order to thoroughly assess the effects of prolapse and incontinence on sexual function, it is important to consider possible confounding variables as well as type of questionnaire utilized. Older age and postmenopausal status, common in women with PFD, are also associated with sexual dysfunction [19] and may alter the association between prolapse and sexual function. Studies which did not use validated and/or disease-specific questionnaires may not be reliable or sensitive enough to detect differences that are due to the disease process(es) of UI, FI, and/or POP or be unable to detect subtle changes in sexual function following treatments for PFD.
Many recent publications examining the impact of UI, FI, and POP using validated generalized and disease-specific questionnaires have reported poorer sexual function in women with PFD. Total PISQ scores were significantly lower in women with UI and/or prolapse as compared to those without, with the largest difference noted in the physical domain [4]. Reported frequency of intercourse was less, and restriction of sexual activity for fear of leakage greater, in those women with PFD as compared to those without. In a population of women with UI and lower urinary tract complaints including interstitial cystitis and recurrent urinary tract infections, the prevalence of female sexual dysfunction utilizing the FSFI was 46%, with low scores for desire, lubrication, and satisfaction, and increase for pain, with no differences in arousal or orgasm [20]. About one third of women attending urogynecology clinics report that UI has an impact on their sexual function and approximately 50% experience leakage with vaginal intercourse or orgasm [21, 22]. Coital incontinence is independently related to higher King’s Health Questionnaire scores, suggesting poorer quality of life as compared to women with UI who do not leak with intercourse [23].
The PISQ scores were significantly less in women with POP as compared to an asymptomatic group similar in age, race, parity, and HRT (mean 81 vs. 106, respectively) [24]. An evaluation of women with UI stratified between ≥Stage 2 prolapse as compared to minimal or no prolapse reported poorer sexual function in those with prolapse, decreased libido, sexual excitement, and orgasm using the PISQ long form [25]. Additionally, women with advanced prolapse (Stage III or IV) complained of a greater impairment of their sex life and were more likely to be abstinent as a result of their prolapse than women with stress urinary incontinence (SUI) [26]. Although these authors utilized a nonvalidated condition-specific questionnaire, 81% of their cohort rated their sexual relations as “somewhat” or “very” satisfactory [26]. This finding reinforces the complexity of female sexual function and an earlier publication which noted that sexual activity was not correlated with vaginal length or introital caliber and no association between vaginal anatomy and complaints of dyspareunia or vaginal dryness [27].
The effect of PFD on sexual function has recently been evaluated using validated quality-of-life PFD dysfunction and sexual function questionnaires [28]. Handa et al. [28] utilized the Pelvic Floor Disorders Inventory 20 (PFDI-20) as well as the Personal Experience Questionnaire, a non-condition-specific validated generalized sexual function questionnaire, and found that higher PFDI-20 scores were associated with decreased arousal, infrequent orgasm, and increased dyspareunia, with similar findings noted for the urinary, colorectal-anal, and prolapse scales of the PFDI-20 [28]. The only sexual problem associated with increasing prolapse was infrequent orgasm. A recent community-based survey assessed the relationship between PFD and sexual activity and satisfaction using the Epidemiology of Prolapse and Incontinence Questionnaire (EPIQ) [29]. The EPIQ was specifically designed to ascertain the prevalence of and risk factors for PFD in an undiagnosed population and includes questions that are related specifically to sexual activity and satisfaction. After controlling for confounding variables, PFD was not significantly associated with sexual activity or satisfaction, but only 43% of the women who had PFD based on EPIQ had sought care for their conditions.
Effects of gynecologic surgeries on sexual function
The effects of gynecologic surgery on sexual function have historically received little attention. Due to the use of different and mainly nonvalidated, self-made questionnaires, lack of definition of sexual function and dysfunction, and non-assessment of impact on QOL, it is difficult to compare older studies and draw conclusions. A recent comprehensive review of the literature found 36 articles involving 4,500 patients, and only 12 used validated questionnaires to assess sexual function after surgery for PFD [30]. Conflicting results were noted with some studies suggesting that surgery for POP and UI deteriorates sexual function, some demonstrating no change and others, improvement in sexual function. The authors concluded that there was a “paucity of properly validated data about sexual function after gynecologic operations” and urged further prospective studies using validated questionnaires. Since this publication, there have been several more well-designed studies assessing the outcomes of surgery for PFD with respect to sexual function.
The PISQ long form was used to assess sexual function before and 3 to 6 months after surgery for prolapse and/or UI in 75 women who underwent a variety of vaginal and abdominal anti-incontinence and pelvic reconstructive surgeries [31]. Postoperatively, 70% of women had higher PISQ scores, while 30% reported lower scores. When analyzed by domain, both the physical and partner-related domains showed significant improvement pre- to postoperatively, while the behavior-emotive did not change. Complaints of pain with intercourse did not increase postoperatively. These data were also analyzed to compare sexual function in those who underwent posterior repair compared to those who had not [32]. PISQ scores demonstrated a significant similar improvement in both groups postoperatively. Women without posterior repair had decreased dyspareunia postoperatively compared to no improvement in this symptom in the posterior repair group.
Similar findings of significant improvement in overall PISQ scores and in the physical and partner-related domains was recently reported in a study from the UK evaluating sexual function prospectively after surgery for PFD [33]. The PISQ’s psychometric properties for use in the UK were also evaluated by correlation with the Sheffield Prolapse Symptoms Questionnaire and the King’s Health Questionnaire preoperatively and 4 months postoperatively. Cronbach α values for the full scale and each of the three domains were similar to the original PISQ validation study [12, 33]. The PISQ did correlate well with some domains of the Sheffield Prolapse Symptoms Questionnaire and the King’s Health Questionnaire (r = .42–.66) [33].
The PISQ-12 has also been used to prospectively evaluate sexual function after surgical treatment for PFD. One year after abdominal sacrocolpopexy, a significant improvement was reported in sexual function, including total PISQ-12 scores, as well as many factors, including increase in percentage of women sexually active and decrease in limitation of intercourse secondary to pain and problems from prolapse and/or UI [34].
Evaluation of surgical treatment of SUI also demonstrates significant improvement on sexual function. Coital incontinence is cured with surgery in 70–90%, and this is associated with improvements in sexual function, with significant increases in PISQ-12 scores both after mid-urethral sling procedures and Burch retropubic urethropexy [34–37]. Once again, improvements were reported in the physical and partner-related domains, but not the behavior-emotive.
The other questionnaire utilized to assess sexual function after surgical treatment of PFD is the FSFI, which is validated, but generalized or non-condition-specific. Pauls et al. [5] utilized the FSFI to assess sexual function prospectively 6 months after vaginal surgery for POP and/or UI and found no differences in FSFI domain or total scores between the pre- and postoperative period. Patients also reported similar degrees of bother due to sexual symptoms on a visual analog scale, and sexual frequency was not significantly changed. Barriers to sexual function were also assessed. Before surgery, vaginal bulging was the most bothersome, which changed to pain after surgery. However, FSFI pain domain scores were not significantly different pre- to postoperative. These authors concluded that there were no overall changes in sexual function because of the exchange of one sexual problem for another.
Interestingly, a significant improvement in sexual function was newly published following anterior and/or posterior repair in a group of 60 women with a mean age of 36 ± 5.4 years from Iran [38]. Mean FSFI scores improved from 15.9 ± 10.7 before surgery to 21.9 ± 11.1 3–4 months after surgery, but the postoperative score is still abnormal, with <26 consistent with sexual dysfunction [8, 38]. Additionally, there were significant increases in the desire, arousal, lubrication, orgasm, and satisfaction domains, but domain scores for satisfaction and pain were still low (<3.7). Pain scores showed a significant deterioration with this very short follow-up after surgery. This is the first report utilizing a validated questionnaire to show an improvement in sexual function related to desire, orgasm, and arousal following surgery for PFD and may be due to the young mean age of the cohort.
Many pelvic floor surgeons are utilizing vaginal mesh to augment anterior and posterior repairs. The use of polypropylene mesh with anterior and post repairs was associated with a marked increase in postoperative dyspareunia and a 12% decrease in sexual activity among those who underwent posterior repair with mesh using the King’s Health Questionnaire [39]. A small sample of 26 women followed for 2 years after posterior repair noted an improvement in sexual function in 95% and only 8% with de novo dyspareunia using the PISQ-12 [40]. The Cleveland Clinic prospectively evaluated three techniques, traditional, site-specific, and porcine graft augmentation, for posterior repair in a randomized controlled trial [41]. With 1.5 years of follow up, there was a significant increase in the PISQ-12 scores and no increase in dyspareunia overall as well as no differences between the three groups. In a separate evaluation, sexual function was compared prospectively before and after posterior repair using porcine dermis graft augmentation or site-specific repair in a nonrandomized fashion using the PISQ long form [42]. A greater improvement in PISQ scores was reported in the porcine graft as compared to the site-specific group (101.3± 6.4 versus 89.7 ± 7.1, respectively), with a significant improvement in the physical domain only. Since the graft group underwent more surgeries for SUI, and one surgeon performed all of the graft augmented and a different surgeon performed all of the site-specific repairs, the improvement in sexual function may have been due to these confounding differences between the two groups.
Two studies have addressed sexual function after surgical repair of fecal incontinence remote from delivery. Retrospective evaluation of sexual function after anal sphincteroplasty noted no correlation between total PISQ-12 scores or any of the PISQ-12 questions and fecal incontinence scores at a mean of 5.6 years postoperatively [43]. More dyspareunia was found with the overlap as compared to the end-to-end technique. Another retrospective study reported improved sensation, satisfaction, and libido in about 33%, and 25% less avoidance of intercourse secondary to fears of fecal incontinence using a nonvalidated questionnaire [44]. However, 6% were “physically” unable to have intercourse.
Summary
The use of validated questionnaires assures data that are reliable, quantifiable, and reproducible. Quality-of-life questionnaires, such as The King’s Health Questionnaire and the Incontinence Impact Questionnaire, have a few questions addressing sexual function but really deal with the overall impact of incontinence and/or prolapse on the patient’s QOL or well being and do not focus on sexual function. General questionnaires focused on sexual function such as the FSFI that underwent validation and reliability testing in a general population may not be sensitive enough to detect differences that are due to PFD. The PISQ is a condition-specific questionnaire focused on sexual function for use in women with PFD and has undergone rigorous validation and reliability testing. Many recent publications examining the impact of UI, FI, and POP using the FSFI and PISQ have reported poorer sexual function in women with PFD. The PISQ has been used most commonly to evaluate sexual function after surgery for PFD, with increased PISQ scores in about 70%. Significant improvement is noted for sexual function related to physical and partner-related factors, with no changes for orgasm, desire, or arousal after surgical repair of PFD. Studies which used generalized sexual function questionnaires mostly found no change in sexual function following surgical treatment of POP and/or UI. When evaluated with validated questionnaires, PFD is associated with a negative impact on sexual function. Surgical correction of POP and/or UI improves sexual function in about 70%, although some studies show no change with the use of non-condition-specific questionnaires.
References
Jolleys JV (1988) Reported prevalence of urinary incontinence in women in a general practice. Br Med J 296:1300–1302
Nygaard I, Bradley C, Brandt D (2004) Pelvic organ prolapse in older women: prevalence and risk factors. Obstet Gynecol 104:489–97
Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL (1997) Epidemiology of surgically managed pelvic organ prolpase and urinary incontinence. Obstet Gynecol 89:501–6
Rogers RG, Villarreal A, Kammerer-Doak D, Qualls C (2001) Sexual function in women with and without urinary incontinence and/or pelvic organ prolapse. Int Urogynecol J 12:361–365
Pauls RN, Silva WA, Rooney CM, Siddighi S, Kleeman SD, Dryfhout V, Karram MM (2008) Sexual function after vaginal surgery for pelvic organ prolapse and urinary incontinence. Am J Obstet Gynecol 97:622e1–622.e7
Creti L, Fichten CS, Libman E, Amsel R, Brender W (1988) Female sexual functioning: a global score for Nowinski and Lopiccolo’s sexual history form. Paper presented at the convention of Canadian Psychological Association, Montreal, Quebec
Rosen RC, Brown C, Heiman J, Leiblum S, Meston CM, Sabsigh R, Ferguson D, D’Agostino R (2000) The Female Sexual Function Index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther 26:191–208
Wiegal M, Meston C, Rosen R (2005) The Female Sexual Function Index (FSFI): cross-validation and development of clinical cutoff scores. J Sex Marital Ther 31:1–20
Meston CM (2003) Validation of the Female Sexual Function Index (FSFI) in women with female orgasmic disorder and in women with hypoactive sexual desire disorder. J Sex Marital Ther 29:39–46
Kelleher CJ, Cardozo LD, Khuller V, Salvatore S (1997) A new questionnaire to assess the quality of life of urinary incontinent women. Br J Obstet Gynecol 104:1374–1379
Wyman JF, Harkins SW, Choi SC, Taylor JR, Fantl JA (1987) Psychosocial impact of urinary incontinence in women. Obstet Gynecol 70:378–381
Rogers RG, Kammerer-Doak DN, Villarreal A, Coates K, Qualls C (2001) A new instrument to measure sexual function in women with urinary incontinence or pelvic organ prolapse. Am J Obstet Gynecol 184:552–558
Price N, Jackson SR, Avery K, Brookes ST, Abrams P (2006) Development and psychometric evaluation of the ICIQ Vaginal Symptoms Questionnaire: the ICIQ-VS. BJOG 113:700–712
Tamanini JT, Almeida FG, Girotti ME, Riccetto CL, Palma PC, Rios LA (2008) The Portuguese validation of the International Consultation on Incontinence Questionnaire-Vaginal Symptoms (ICIQ-VS) for Brazilian women with pelvic organ prolapse. Int Urogynecol J Pelvic Floor Dysfunct 19(10):1385–1391
Rogers RG, Coates KW, Kammerer-Doak DN, Khalsa S, Qualls C (2003) A short form of the pelvic organ prolapse/urinary incontinence sexual questionnaire (PISQ-12). Int Urogyn JPFD 14:164–168
Pons EM, Clota PM, Aguilon GM, Zardain PC, Alvarez RP (2008) Questionnaire for evaluation of sexual function in women with genital prolapse and/or incontinence. Validation of the Spanish version of “Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire (PISQ-12)”. Actas Urol Esp 32:211–219
Romero AA, Hardart A, Rogers R, Kobak B (2003) Validation of a Spanish version of the Pelvic Organ Prolapse Incontinence Sexual Questionnaire (PISQ). Obstet Gynecol 102:1000–1005
Aschkenzi SO, Botros SM, Beaumont J, Miller JJ, Gamble T, Sand PK, Goldberg RP (2008) Use of the Short Pelvic Organ Prolapse/Urinary Incontinence Sexual Questionnaire for Female Sexual Dysfunction in a general population. Obstet Gynecol 111(4S):10S
Dennerstein L, Alexander JL, Kotz K (2003) The menopause and sexual functioning: a review of the population-based studies. Annu Rev Sex Res 14:64–82
Salonia A, Zanni G, Nappi RE, Briganti A, Deho F, Fabbri F, Colombo R, Guazzoni G, Di Girolamo V, Rigatti P, Montorsi F (2004) Sexual dysfunction is common in women with lower urinary tract symptoms and urinary incontinence: results of a cross-sectional study. Eur Urol 45:642–648
Vierhout ME, Gianotten WL (1993) Mechanisms of urine loss during sexual activity. Eur J Obstet Gynecol Repro Biol 52:45–47
Temml C, Haidinger G, Schmidbauer J, Schatzl G, Madersbacher S (2000) Urinary incontinence in both sexes: prevalence rates and impact on quality of life and sexual life. Neurourol Urodyn 19:259–271
Pons ME, Clota MP (2008) Coital urinary incontinence: impact on quality of life as measured by the King’s Health Questionnaire. Int Urogynecol J 19:621–625
Novi JM, Leronis S, Morgan MA, Arya LA (2005) Sexual function in women with pelvic organ prolapse compared to women without pelvic organ prolapse. J Urol 173:1669–1672
Ozel B, White T, Urwitx-Lane R, Minaglia S (2005) The impact of pelvic organ prolapse on sexual function in women with urinary incontinence. Int Urogyn J 17:14–17
Barber MD, Visco AG, Wyman JF, Fantl JA, Bump RC (2002) Sexual function in women with urinary incontinence and pelvic organ prolapse. Obstet Gynecol 99:281–289
Weber AM, Walters MD, Schover LR, Mitchinson A (1995) Vaginal anatomy and sexual function. Obstet Gynecol 86:946–949
Handa VL, Cundif G, Chang HH, Helzlsouer KJ (2008) Female sexual function and pelvic floor disorders. Obset Gynecol 111:1045–1052
Lukacz ES, Whitcomb EL, Lawrence JM, Nager CW, Contreras R, Luber KM (2007) Are sexual activity and satisfaction affected by pelvic floor disorders? Analysis of a community-based survey. Am J Obstet Gynecol 197:e1–88.e6
Ghielmetti T, Kuhn P, Dreher EF, Kuhn A (2006) Gynaecological operations: do they improve sexual life? Eur J Obstet Gynecol Reprod Biol 129:104–110
Rogers RG, Kammerer-Doak D, Darrow A, Murray K, Qualls C, Olsen A, Barber M (2006) Does sexual function change after surgery for stress urinary incontinence and/or pelvic organ prolapse? A multicenter prospective study. Am J Obstet Gynecol 195(5):e1–e4
Komesu YM, Rogers RG, Kammerer-Doak DN, Barber MD, Olsen AL (2007) Posterior repair and sexual function. Am J Obstet Gynecol 197:101.e1–6
Thakar R, Chawla S, Scheer I, Barrett G, Sultan AH (2008) Sexual function following pelvic floor surgery. Int J Gynaecol Obstet 102:110–114
Handa VL, Zyczynski HM, Brubaker L, Nygaard I, Janz NK, Richter HE (2007) Sexual function before and after abdominosacrocolpopexy. Am J Obstet Gynecol 197:629.e1–629.e6 for the Pelvic Floor Disorders Network
Salonia A, Briganti A, Deho F, Zanni G, Rigatti P, Montorsi F (2006) Women’s sexual dysfunction: a review of the “surgical landscape”. E Urol 50:44–52
Ghezzi F, Serati M, Cromi A, Uccella S, Triacca P, Bolis P (2006) Impact of tension-free vaginal tape on sexual function: Results of a prospective study. Int Urogynecol J Pelvic Floor Dysfunct 17:54–59
Jha S, Moran P, Greenham H, Ford C (2007) Sexual function following surgery for urodynamic stress incontinence. Int Urogynecol J Pelvic Floor Dysfunct 18:845–850
Azar M, Noohi S, Radfar S, Radfar MH (2008) Sexual function in women after surgery for pelvic organ prolapse. Int Urogyn J 19:53–57
Milani R, Salvatore S, Soligo M, Pifarotti P, Meschia M, Cortese (2005) Functional and anatomical outcome of anterior and posterior vaginal prolapse repair with prolene mesh. BJOG 112:107–111
de Tayrac R, Picone O, Chauveaud-Lambling A, Fernandez H (2006) A 2-year anatomical and functional assessment of transvaginal rectocele repair using a polypropylene mesh. Int Urogyn J Pelvic Floor Dysfunct 17:100–105
Paraiso MF, Barber MD, Muir TW, Walters MD (2006) Rectocele repair: a randomized trial of three surgical techniques including graft augmentation. Am J Ob Gyn 195:1762–1771
Novi JM, Bradley CS, Mahmoud NN, Morgan MA, Arya LA (2007) Sexual function in women after rectocele repair with acellular porcine demis graft vs site-specific rectovaginal fascia repair. Int Urogyn J Pelvic Floor Dysfunct 18:1163–1169
Trowbridge ER, Morgan D, Trowbridge JJ, Delancey JO, Fenner D (2006) Sexual function, quality of life and severity of anal incontinence after anal sphincteroplasty. Am J Obstet Gynecol 195:1753–1757
Lewicky CE, Valentin C, Saclarides TJ (2004) Sexual function following sphincteroplasty for women with third-and fourth-degree perineal repairs. Dis Colon Rectum 47:1650–1654
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kammerer-Doak, D. Assessment of sexual function in women with pelvic floor dysfunction. Int Urogynecol J 20 (Suppl 1), 45–50 (2009). https://doi.org/10.1007/s00192-009-0832-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-009-0832-y