Abstract
Our objective was to evaluate the outcome of laparoscopic Burch colposuspension in women with recurrent stress urinary incontinence after failed primary sub-urethral tape procedures. A total of 16 patients were identified, and their data from symptom-specific questionnaires, urodynamic studies and urogynaecological assessment were collected. At a median follow-up of 24.5 months, objective and subjective cure rates were 54.5% and 92.9%, respectively. Average satisfaction score regarding outcome after surgery was 9.3 on a rating scale from 0 to 10. All but one patient had symptoms of urge incontinence pre-operatively with 64.3% experiencing cure or improvement post-operatively. Voiding difficulties were observed in one patient, and post-operative urodynamics revealed a significant decrease in urinary flow rate (p < 0.05) but with no difference in urinary residuals or maximum urethral closure pressure. Severe peri-urethral fibrosis was identified in 62.5% of the patients. Laparoscopic Burch colposuspension is an effective and safe surgical option.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Polypropylene sub-urethral tape procedures are well established in the treatment of female stress urinary incontinence [1]. Long-term success rates are equal to the ‘gold standard’ open Burch colposuspension [1, 2]. With the increasing popularity of synthetic sub-urethral tapes, it is inevitable that we will see women presenting with recurrent stress urinary incontinence after failed surgery.
Colposuspension after previous failed incontinence surgery has been reported to be a feasible choice to treat patients with recurrent stress urinary incontinence [3–6], although it is believed more likely to fail with increasing number of previous procedures [7, 8]. It has a higher complication rate [3, 9] and can be technically difficult, especially after previous retropubic surgery [6].
A recent meta-analysis comparing laparoscopic and open Burch colposuspension has shown low peri-operative complication rates, shorter hospital stay and faster return to daily activities in favour for the laparoscopic approach and with objective cure equal for both techniques at 5-year follow-up [10].
Two studies have reported on efficacy of laparoscopic colposuspension for recurrent urinary stress incontinence [11, 12]. The authors summarised a wide variety of primary procedures including anterior repairs, colposuspensions, Manchester repairs, needle suspensions, pubovaginal slings and sub-urethral tapes, which make assessment of outcome rates difficult as they may vary with the type of previous surgery. To date, little is known about secondary colposuspension after previous sub-urethral tape procedures. The aim of this study is to report on the cure rates and complications of laparoscopic Burch colposuspension after failed sub-urethral tapes.
Materials and methods
In our clinic, patients who present with recurrent stress urinary incontinence after previous sub-urethral tape procedure are routinely offered a laparoscopic Burch colposuspension. Sixteen women who underwent surgery between January 2002 and August 2006 were identified and contacted for assessment in the clinic. Data collected from pre- and post-operative workup included a urogynaecological examination, a validated symptom-specific questionnaire [13] and urodynamic studies including cystomanometry, urethral profile, flowmetry and measurement of post-void urinary residual. Urethral mobility was measured by perineal ultrasound. Peri-operative and short-term post-operative characteristics were subsequently collected. At review, women were asked to score their satisfaction on an 11-point rating scale from 0 (not satisfied at all) till 10 (very satisfied). Prolapse was evaluated by assessing women in the left lateral position with a Sims speculum and using the pelvic organ prolapse quantification system [14].
This study was approved by the Human Research Ethics Committee of the Royal Brisbane and Women’s Health Service District (approval number 2005/017) and followed the Declaration of Helsinki. Informed consent was obtained from all patients.
Surgical technique
Three trocar entrance sites were used to perform a Burch colposuspension laparoscopically. The cave of Retzius was exposed through careful sharp dissection close to the pubic bone to minimise bladder or urethral injury. Once identified, tape arms were divided bilaterally at the level of the pubic bone and mobilised with sharp dissection from the peri-urethral and vesical region. The tapes were not removed, and the bladder was reflected medially. Two non-absorbable sutures (no. 1 ethibond; Ethicon) were placed bilaterally at the level of the bladder neck and used to suspend the vaginal fornices to the ipsilateral iliopectineal ligament without undue tension. The surgeon’s fingers were in the vagina while inserting sutures to ensure the placement was accurate. All patients received prophylactic antibiotic cover at induction of anaesthesia. An indwelling urethral catheter was inserted at the beginning of surgery and left in situ for 24 h post-operatively.
Statistical analysis
Surgical outcomes were assessed using data from urodynamic results, urinary symptom questionnaires and a patient-determined satisfaction score. Subjective cure was defined as none or rare stress urinary incontinence, and objective cure was defined as an inability to demonstrate urinary incontinence on provocative urodynamics. A patient satisfaction score of 8 or more was considered successful.
Diagnosis of urethral obstruction was defined as maximum flow (Q max) less than 15 mL/s with a voided volume greater than 150 mL and/or post void residuals of more than 20% of the volume voided. Data were analysed using SPSS software (SPSS, Chicago, IL, USA).
For analysis of binary data from symptom-specific questionnaires, the McNemar test was employed, and non-parametric skewed variables were compared with the Wilcoxon matched-pairs signed-rank test. p < 0.05 was considered to be significant.
Results
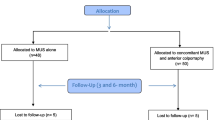
We identified 16 cases by retrospective chart review. Two patients could not be contacted and were excluded. Fourteen women were subsequently reviewed in the clinic, and 11 underwent post-operative urodynamic studies. Median follow-up was 24.5 months (range 3–58). Three patients (27.3%) were diagnosed with a co-existing overactive bladder pre-operatively. Demographic characteristics are summarised in Table 1.
Intra-operatively, one laparoscopic colposuspension needed conversion to an open approach because of dense abdominal adhesions. One inadvertent cystotomy was identified and repaired laparoscopically and with an indwelling catheter for 7 days. No woman suffered significant haemorrhage (>500 mL). Peri-urethral fibrosis was seen in 10 of 16 patients (62.5%) who had a previous tension-free vaginal tape (TVT) or intra-vaginal slingplasty and which was divided before performing the Burch colposuspension. One patient developed short-term urinary retention post-operatively, which was treated with intermittent self-catheterisation for 3 days. Table 2 features intra- operative and early post-operative data whilst in hospital.
At index of review in the clinic, 54.6% (6 of 11) of the patients had no evidence of urodynamic stress urinary incontinence, and one patient developed de novo urge incontinence (9.1%). Detrusor overactivity could not be demonstrated on repeat urodynamic studies post-operatively in two out of three patients with co-existing detrusor overactivity before surgery. Urinary flow rates were significantly reduced (p = 0.03) but without change in bladder volume, urinary residuals or maximum urethral closure pressure (MUCP). See Table 3 for pre- and post-operative urodynamic parameters.
Subjectively, 64.3% (9 of 14) of the patients denied symptoms of stress urinary incontinence, and 92.9% (13 of 14) reported improvement (cured or occasional incontinence) after surgery. All but one patient (92.3%) had symptoms of urge incontinence pre-operatively with 64.3% (9 of 14) reporting improvement post-operatively, 3 of 14 (21.4%) patients noticed no difference and 2 of 14 (14.3%) felt that symptoms got worse. There was no subjective difference in feeling of incomplete emptying or weak urinary stream post-operatively compared to prior to surgery. Table 4 summarises pre- and post-operative subjective outcome measures obtained from symptom-specific questionnaires.
If we consider patients that could not be contacted for follow-up as failures, adjusted objective and subjective cure rates are 46.1% (6 of 13) and 56.2% (9 of 16), respectively.
Three patients (21.4%) reported recurrent urinary tract infections since the surgery. No increased incidence of pelvic organ prolapse was found during post-operative review. Mean patients satisfaction score was 9.36 ± 1.08 (mean ± SD; range 6–10).
Discussion
Advances in surgical techniques have led to an availability of a number of minimal invasive surgeries to treat stress urinary incontinence, with one of them being the TVT (Gynecare, Ethicon). The TVT is one of the most thoroughly investigated and documented minimal-invasive procedures [15], with an objective and subjective success rate of 81.3% at 7 years for treatment of primary stress urinary incontinence [1] and with equal results when performed for treatment of recurrent stress incontinence at 4 years follow-up [16]. Probably because of this high success, little is known about the treatment of recurrent stress urinary incontinence after synthetic sub-urethral tape procedures. Repeat TVT appears to be successful; but, so far, there have been only two reported case series with seven women in total [17, 18]. Depending on the probable underlying pathology of recurrent stress incontinence, previous performed surgery, patients’ condition and preference, a variety of treatment options are available. This retrospective study has demonstrated that laparoscopic colposuspension after failed sub-urethral synthetic tape surgery is a feasible choice, given the objective and subjective improvement of urinary symptoms and with very few complications. A traditional autologous fascia lata sling could be an alternative option to treat recurrent stress urinary incontinence but with a much higher reported complication and morbidity rate [19]. One can imagine that autologous sling surgery might become technically difficult especially after previous synthetic sling surgery, and, currently, no data are available for this particular case scenario. Patients with recurrent stress urinary incontinence who are compromised by medical conditions, age or personal concerns may benefit from the injection of a peri-urethral bulking agent. Cure or improvement rates are reported to be approximately 40–60% [20, 21] in case of recurrent stress urinary incontinence, which is lower than a repeat colposuspension or sling procedure. Safety and low impact of these procedures are characteristics favourable for those desiring less invasive surgery. The currently used bulking agents are associated with acceptable low rates of acute local complications, including transient haematuria, urinary retention, uncomplicated urinary tract infections and de novo urge incontinence. The crux with bulking agents is their durability defining long-term efficacy and satisfaction. However, injecting a peri-urethral bulking agent may easily be repeated and is cost effective because of the possibility of a daycare setting.
We identified 16 patients in our study that underwent a laparoscopic Burch colposuspension for recurrent stress urinary incontinence after failed sub-urethral tape procedures and reported an objective and subjective success rate of 54.5% and 92.9%, respectively. We did not exclude patients with a low-pressure urethra and intrinsic urethral sphincter deficiency, which is thought to be an important factor in failure of continence surgery [22, 23]. This could be a possible explanation for our low objective success rate compared with other reports in literature [3, 5, 6, 12]. We measured an MUCP < 20 mmH2O in 37.5% (n = 6 of 16) of the women included in this study. Comparison with other studies is difficult as there is a wide variety of inclusion criteria and no studies are available that include only patients with recurrent stress urinary incontinence after one type of primary incontinence surgery.
The subjective cure rate based on the sum of patients with no urinary leakage or less than once a week was higher than the objective cure rate that is in line with reports from others [8, 24]. One may question which measure is most important in practice as we cannot consider urinary leakage significant until patients are reporting so. Furthermore, situations similar to a urodynamic stress test where women are asked to cough with a bladder at maximum capacity are not often present during daily activity.
In our study population, symptoms of urge incontinence were common (92.3%) before surgery with 64.3% of the patients reporting significant improvement post-operatively (p = 0.05). A possible explanation for this finding could be the presence of dense peri-urethral fibrosis because of foreign body reaction found in 56.3% of the patients and divided at the time of the surgery. Analysing this group of women with dense urethral fibrosis separately, all women were found to be reporting irritative voiding symptoms before surgery and with five of nine patients (55.6%) suffering urge incontinence on a daily base. Post-operatively, seven patients (77.8%) reported cure or improvement. Considering the division of fibrosis seems to be worthwhile, but a larger study population would be needed to draw a reliable conclusion.
Scarring, fibrosis and distorted anatomy in the cave of Retzius have been described especially after previous retropubic surgery, which can increase the risk of surgical complications and make secondary colposuspension difficult [6]. Nevertheless, at time of pre-operative clinical assessment, all women had a normal vaginal length and no evidence of a rigid urethra on ultrasound or cough test.
Short-term post-operative voiding difficulties occurred only in one patient (6.25%). However, urodynamic studies performed at time of post-operative review revealed a significant decrease in flow rate, which may reflect an element of outflow obstruction, although urinary residuals were low. These findings are in line with that of other authors [3, 5, 6, 25, 26].
Two limitations of this study are its very small case numbers and a potential selection bias in favour of one surgical treatment for recurrent stress urinary incontinence. A formal comparison between treatment options such as laparoscopic Burch colposuspension, sub-urethral tape procedure or bulking agents for the treatment of recurrent incontinence has not been made. Nevertheless, the present study would appear to be the only one of its kind so far reported.
Conclusion
Laparoscopic Burch colposuspension appears to be a valid option for treatment of recurrent stress urinary incontinence after failed sub-urethral tape procedures with a very high overall patient satisfaction rate. Randomised controlled trials comparing surgical procedures available for treatment of recurrent stress urinary incontinence are needed.
References
Nilsson CG, Falconer C, Rezapour M (2004) Seven-year follow-up of the tension-free vaginal tape procedure for treatment of urinary incontinence. Obstet Gynecol 104:1259–1262
Ward KL, Hilton P, UK and Ireland TVT Trial Group (2004) A prospective multicenter randomized trial of tension-free vaginal tape and colposuspension for primary urodynamic stress incontinence: two-year follow-up. Am J Obstet Gynecol 190:324–331
Cardozo L, Hextall A, Bailey J et al (1999) Colposuspension after previous failed incontinence surgery: a prospective observational study. Br J Obstet Gynaecol 106:340–344
Amaye-Obu FA, Drutz HP (1999) Surgical management of recurrent stress urinary incontinence: a 12-year experience. Am J Obstet Gynecol 181:1296–1307
Thakar R, Stanton S, Prodigalidad L et al (2002) Secondary colposuspension: results of a prospective study from a tertiary referral centre. BJOG 109:1115–1120
Maher C, Dwyer P, Carey M et al (1999) The Burch colposuspension for recurrent urinary stress incontinence following retropubic continence surgery. Br J Obstet Gynaecol 106:719–724
Alcalay M, Monga A, Stanton SL (1995) Burch colposuspension: a 10–20 year follow up. Br J Obstet Gynaecol 102:740–745
Jarvis GJ (1994) Surgery for genuine stress incontinence. Br J Obstet Gynaecol 101:371–374
Kjolhede P, Ryden G (1997) Clinical and urodynamic characteristics of women with recurrent urinary incontinence after Burch colposuspension. Acta Obstet Gynecol Scand 76:461–467
Dean N, Ellis G, Wilson P et al (2006) Laparoscopic colposuspension for urinary incontinence in women. Cochrane Database Syst Rev 3:CD002239
Maher C, Qatawneh A, Baessler K et al (2004) Laparoscopic colposuspension or tension-free vaginal tape for recurrent stress urinary incontinence and/or intrinsic sphincter deficiency—a randomised controlled trial. Neurourol Urodyn 23:433–434
Moore RD, Speights SE, Miklos JR (2001) Laparoscopic Burch colposuspension for recurrent stress urinary incontinence. J Am Assoc Gynecol Laparosc 8:389–392
Baessler K, O’Neill S, Maher C et al (2004) A validated female pelvic floor questionnaire for clinicians and researchers. Neurourol Urodyn 23:398–399
Bump RC, Mattiasson A, Bo K et al (1996) The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol 175:10–17
Valpas A, Nilsson CG (2004) Tension-free vaginal tape procedure and laparoscopic colposuspension in the treatment of stress urinary incontinence. Curr Opin Obstet Gynecol 16:319–323
Rezapour M, Ulmsten U (2001) Tension-free vaginal tape (TVT) in women with recurrent stress urinary incontinence—a long-term follow up. Int Urogynecol J 12(Suppl 2):S9–S11
Riachi L, Kohli N, Miklos J (2002) Repeat tension-free transvaginal tape (TVT) sling for the treatment of recurrent stress urinary incontinence. Int Urogynecol J 13:133–135, discussion 135
Moore RD, Gamble K, Miklos JR (2007) Tension-free vaginal tape sling for recurrent stress incontinence after transobturator tape sling failure. Int Urogynecol J 18:309–313
Flynn BJ, Yap WT (2002) Pubovaginal sling using allograft fascia lata versus autograft fascia for all types of stress urinary incontinence: 2-year minimum followup. J Urol 167:608–612
Monga AK, Robinson D, Stanton SL (1995) Periurethral collagen injections for genuine stress incontinence: a 2-year follow-up. Br J Urol 76:156–160
Khullar V, Cardozo LD, Abbott D et al (1997) GAX collagen in the treatment of urinary incontinence in elderly women: a two year follow up. Br J Obstet Gynaecol 104:96–99
Sand PK, Bowen LW, Panganiban R et al (1987) The low pressure urethra as a factor in failed retropubic urethropexy. Obstet Gynecol 69:399–402
Koonings PP, Bergman A, Ballard CA (1990) Low urethral pressure and stress urinary incontinence in women: risk factor for failed retropubic surgical procedure. Urology 36:245–248
Bidmead J, Cardozo L, McLellan A et al (2001) A comparison of the objective and subjective outcomes of colposuspension for stress incontinence in women. Br J Obstet Gynaecol 108:408–413
Stanton SL (1985) Stress incontinence: why and how operations work. Clin Obstet Gynaecol 12:369–377
Bombieri L, Freeman RM, Perkins EP et al (2002) Why do women have voiding dysfunction and de novo detrusor instability after colposuspension? Br J Obstet Gynaecol 109:402–412
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
De Cuyper, E.M., Ismail, R. & Maher, C.F. Laparoscopic Burch colposuspension after failed sub-urethral tape procedures: a retrospective audit. Int Urogynecol J 19, 681–685 (2008). https://doi.org/10.1007/s00192-007-0506-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-007-0506-6