Abstract
Purpose
The aim was to validate a new MRI method to measure the buckling phenomenon of the PCL, representative of anterior tibial translation, by comparing its reliability and accuracy to identify anterior cruciate ligament (ACL)-deficient knees with existing methods.
Methods
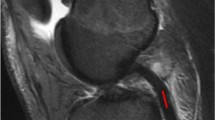
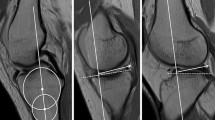
Patients were selected retrospectively and separated into a group of primary ACL injuries and ACL-intact knees. Exclusion criteria were: skeletal immaturity, PCL or a concomitant collateral ligament injury, signs of osteoarthritis (> 1 Kellgren and Lawrence score), tibial plateau fracture, previous ACL reconstruction or displaced meniscal bucket handle tear. The assessment of the curvature of the anterolateral bundle of the PCL was performed on T2 sagittal MRI slices according to 3 methods: (1) the PCL angle (PCLA), (2) the PCL inclination angle (PCLIA) and (3) a new method: the PCL-posterior cortex angle (PCL–PCA), representing the angle between the vertical part of the PCL-ALB and the posterior diaphyseal cortex of the femur. For each method, the inter- and intra-observer reliability was measured. The ability to discriminate both ACL-deficient and ACL-intact knees was evaluated using ROC curves.
Results
Twenty-four patients were included in each group. Intra-observer reliability was excellent for all 3 methods (ICCs > 0.90). Inter-observer reliability was excellent for the PCL–PCA (ICC > 0.90) and good for the PCLA and the PCLIA (ICCs between 0.75 and 0.90). The PCL–PCA had the highest precision (lowest standard error of measurement: 2.7°). It yielded an excellent discrimination between the ACL and CTL groups (AUC 0.80 [0.67–0.93]) with the highest sensitivity (71% [52.8–89.2]) and specificity (88% [75–100]) for a positive threshold when the angle was ≤ 22.7°. The PCLA and PCLIA methods led to acceptable discrimination and lower sensitivities and specificities (PCLA: AUC 0.71, sensitivity 63%, specificity 79%, threshold ≤ 117.9°; PCLIA: AUC 0.62, sensitivity 50%, specificity 83%, threshold ≤ 21.4°).
Conclusion
In comparison with previously described methods, the PCL–PCA was the most reliable and accurate method to measure the PCL buckling phenomenon on MRI in anterior cruciate ligament (ACL)-deficient knees. It offers an easy and objective method for the follow-up of ACL-injured patients and can therefore be recommended for routine use.
Level of evidence
IV.




Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.References
Boeree NR, Ackroyd CE (1992) Magnetic resonance imaging of anterior cruciate ligament rupture. A new diagnostic sign. J Bone Jt Surg Br 74:614–616
Celikyay F, Yuksekkaya R, Bilgic E (2020) A retrospective comparison of ACL tear and mucoid degeneration MRI findings and an emphasis on evaluating of ACL, blumensaat, and PCL angles. J Belg Soc Radiol 104:36
Fluss R, Faraggi D, Reiser B (2005) Estimation of the Youden Index and its associated cutoff point. Biom J 47:458–472
Gali JC, Almeida TA, de Moraes Miguel DC, Nassar SA, Filho JCG, Drain NP, Fu FF (2022) The posterior cruciate ligament inclination angle is higher in anterior cruciate ligament insufficiency. Knee Surg Sports Traumatol Arthrosc 30:124–130
Gentili A, Seeger LL, Yao L, Do HM (1994) Anterior cruciate ligament tear: indirect signs at MR imaging. Radiology 193:835–840
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16:494–502
Koo TK, Li MY (2016) A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med 15:155–163
Lee JK, Yao L, Phelps CT, Wirth CR, Czajka J, Lozman J (1988) Anterior cruciate ligament tears: MR imaging compared with arthroscopy and clinical tests. Radiology 166:861–864
Lee K, Siegel MJ, Lau DM, Hildebolt CF, Matava MJ (1999) Anterior cruciate ligament tears: MR imaging-based diagnosis in a pediatric population. Radiology 213:697–704
Macchiarola L, Jacquet C, Dor J, Zaffagnini S, Mouton C, Seil R (2022) Side-to-side anterior tibial translation on monopodal weightbearing radiographs as a sign of knee decompensation in ACL-deficient knees. Knee Surg Sports Traumatol Arthrosc 30:1691–1699
Mandrekar JN (2010) Receiver operating characteristic curve in diagnostic test assessment. J Thorac Oncol 5:1315–1316
McCauley TR, Moses M, Kier R, Lynch JK, Barton JW, Jokl P (1994) MR diagnosis of tears of anterior cruciate ligament of the knee: importance of ancillary findings. Am J Roentgenol 162:115–119
Mehl J, Otto A, Baldino JB, Achtnich A, Akoto R, Imhoff AB, Scheffler S, Petersen W (2019) The ACL-deficient knee and the prevalence of meniscus and cartilage lesions: a systematic review and meta-analysis (CRD42017076897). Arch Orthop Trauma Surg 139:819–841
Mellado JM, Calmet J, Olona M, Giné J, Saurí A (2004) Magnetic resonance imaging of anterior cruciate ligament tears: reevaluation of quantitative parameters and imaging findings including a simplified method for measuring the anterior cruciate ligament angle. Knee Surg Sports Traumatol Arthrosc 12:217–224
Mink JH, Levy T, Crues JV (1988) Tears of the anterior cruciate ligament and menisci of the knee: MR imaging evaluation. Radiology 167:769–774
Polat A, Acar N, Aybar A, Fidan F, Özden E, Gürkan O (2021) The correlation between posterior cruciate ligament buckling sign and meniscofemoral ligaments: a radiological study. Jt Dis Relat Surg 32:371–376
Robertson PL, Schweitzer ME, Bartolozzi AR, Ugoni A (1994) Anterior cruciate ligament tears: evaluation of multiple signs with MR imaging. Radiology 193:829–834
Sawilowsky S (2009) New effect size rules of thumb. J Mod Appl Stat Methods 8:597–599
Schweitzer ME, Cervilla V, Kursunoglu-Brahme S, Resnick D (1992) The PCL line: an indirect sign of anterior cruciate ligament injury. Clin Imaging 16:43–48
Seil R, Cucchi D, Ninulescu C, Dor J, Mouton C (2019) Anatomic anterior cruciate ligament reconstruction for adolescent patients with open physis. Ann Jt 4:31
Tung GA, Davis LM, Wiggins ME, Fadale PD (1993) Tears of the anterior cruciate ligament: primary and secondary signs at MR imaging. Radiology 188:661–667
Van Dyck P, Gielen JL, Vanhoenacker FM, Wouters K, Dossche L, Parizel PM (2012) Stable or unstable tear of the anterior cruciate ligament of the knee: an MR diagnosis? Skelet Radiol 41:273–280
Yoo JD, Lim HM (2012) Morphologic changes of the posterior cruciate ligament on magnetic resonance imaging before and after reconstruction of chronic anterior cruciate ligament ruptures. Knee Surg Relat Res 24:241–244
Yoon JP, Chang CB, Yoo JH, Kim SJ, Choi JY, Choi J-A, Seong SC, Kim TK (2010) Correlation of magnetic resonance imaging findings with the chronicity of an anterior cruciate ligament tear. J Bone Jt Surg Am 92:353–360
Yoon JP, Yoo JH, Chang CB, Kim SJ, Choi JY, Yi JH, Kim TK (2013) Prediction of chronicity of anterior cruciate ligament tear using MRI findings. Clin Orthop Surg 5:19–25
Funding
No benefits in any form have been received or will be received related directly or indirectly to the subject of this article.
Author information
Authors and Affiliations
Contributions
RSi and CP have made substantial contributions to conception, study design, acquisition/interpretation of data, and in drafting the manuscript. CM and RSe have been involved in the conception, study design, interpretation of data, and critical revision of the manuscript. Each author has given final approval of the version to be published and agrees to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
As the study was performed in accordance with ethical standards of the institutional and national research committees, it did not require prior approval.
Informed consent
The data for this retrospective study were collected from the medical records of patients which were obtained for routine clinical purposes. All data were exported anonymously by the team of clinicians taking care of the included patients who therefore were granted access to their medical records.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Siboni, R., Pioger, C., Mouton, C. et al. The posterior cruciate ligament–posterior femoral cortex angle: a reliable and accurate MRI method to quantify the buckling phenomenon of the PCL in ACL-deficient knees. Knee Surg Sports Traumatol Arthrosc 31, 332–339 (2023). https://doi.org/10.1007/s00167-022-07145-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-022-07145-6