Abstract
We evaluated the diagnostic utility of magnetic resonance imaging (MRI) for predicting anterior cruciate ligament (ACL) tears using both quantitative parameters and nonquantitative imaging findings. MRI examinations were retrospectively evaluated in a group of patients with arthroscopically confirmed complete ACL tear and in a control group with arthroscopically confirmed intact ACL. We evaluated multiple MRI features to compare their sensitivity and specificity for detecting ACL tears. Particular emphasis is put on the evaluation of three different quantitative parameters, including a simplified method for measuring the ACL angle. With a threshold value of 45° the ACL angle reached a sensitivity and specificity of 100% for detecting ACL tears. With a threshold value of 0° the Blumensaat angle had a sensitivity of 90% and a specificity of 98%. Finally, a threshold value of 115° gave the posterior cruciate ligament angle a sensitivity of 70% and a specificity of 82%. Discontinuity was found to be the most useful of the ACL abnormalities. Of the secondary findings anterior tibial displacement was the best predictor of ligamentous injury. However, ACL abnormalities and secondary findings, alone or combined, failed to surpass the diagnostic value of the ACL angle for predicting ACL tears. Quantitative parameters are thus good predictors of ACL tears and may increase the overall sensitivity and specificity of MRI. The ACL angle may be confidently measured in a single MRI section and can be considered to be the most reliable quantitative parameter for detecting ACL tears.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Most anterior cruciate ligament (ACL) tears can and should be diagnosed from clinical history and physical examination [1]; however, magnetic resonance imaging (MRI) may provide useful information regarding the status of the ACL ligament and the extent of associated bone and soft-tissue derangements [2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20]. The sensitivity and specificity of multiple primary and secondary MRI features for diagnosing ACL tears have been extensively measured and compared, either independently [10, 15, 17, 18, 19] or combined [3, 6, 8, 12, 20]. The utility of MRI for diagnosing and distinguishing acute and chronic ACL tears has been addressed [3, 5, 11]. The independent value of conventional [4] and complementary [2, 7] MRI planes and the intrinsic importance of various MRI sequences [6] have been tested and discussed. The use of extremely thin MRI sections has also been described [7]. In addition, the feasibility of MRI for diagnosing ACL tears in a pediatric population has been investigated [8]. In both adult and pediatric populations the overall sensitivity of MRI for diagnosing ACL tears has been reported to be 93%–100% and specificity 85%–100%.
It has been suggested that MRI for detecting ACL tears should be quantitatively evaluated to improve the reproducibility and accuracy of the test. Special attention has focused on quantifying the horizontalization of torn ACL. This may be particularly subtle in chronic tears when a fibrous union between the two cruciate ligaments occurs [3, 5, 8, 9, 11, 14, 18, 19]. However, many of these measurements have never been widely and systematically used, probably because they are cumbersome and time consuming. Our aim was to reevaluate and compare the diagnostic utility of various quantitative parameters and nonquantitative imaging findings for diagnosing ACL tears by MRI. Particular emphasis is put on the evaluation of three different quantitative parameters, including a simplified method for measuring the ACL angle.
Materials and methods
Study design
We retrospectively evaluated preoperative MRI studies in 100 patients whose ACL status had been surgically confirmed. Two different groups of patients were considered. The first consisted of 50 patients in whom ACL tear was arthroscopically confirmed and repaired (44 men, 6 women; mean age 27.4±6.5 years, range 15–41); only complete tears were included in the study. The second group, considered as the control group, consisted of 50 other patients whose meniscus had been explored and operated on by arthroscopy and whose ACL had been found intact (31 men, 19 women; mean age 41.5±13.1 years, range 11–71). One patient in the control group was later found to have a partial ACL tear, but it was considered to be related to recent trauma and subsequent to the MRI study.
The MRI studies of the 100 patients were performed in two different institutions, with a device of either 1.0 or 1.5 T. Slightly different MRI protocols were used although most patients underwent the following sequences: axial T1-weighted sequence (TR/TE 500–600/8–15 ms), sagittal proton density (PD) and T2-weighted sequence (TR/TE 2800–3350/15–86 ms), axial and/or coronal T2*-weighted sequence (TR/TE 850–1100/17–31 ms, flip angle 30°), and axial or coronal fat-saturated PD-weighted sequence (TR/TE 1800–2200/17–25 ms, flip angle 150).
All the MRI studies of the patients were retrospectively reviewed on film hardcopies by a musculoskeletal radiologist (J.M.M.) and an orthopedic surgeon (J.C.) who were blinded to the arthroscopic findings, clinical history, and initial MRI interpretations. Patients and controls were randomly mixed for imaging review. Various categories of imaging signs were evaluated in both groups, including quantitative parameters and nonquantitative imaging findings. The quantitative parameters were measured with a hand-held goniometer by a single observer (J.C.). A single measurement was performed in all the quantitative parameters. The evaluation of nonquantitative MRI findings, which included ACL abnormalities, secondary findings, and associated injuries was also performed by a single observer (J.M.M.). All patients included in the study underwent arthroscopic surgery. The medical charts and arthroscopic reports of all patients were retrospectively reviewed to determine, when possible, the age of the injury and the surgical findings; however, as the age of the ligamentous injury could not be consistently ascertained in a significant number of patients, this parameter could not be statistically evaluated.
Evaluation of quantitative parameters
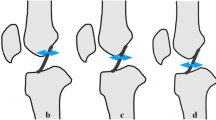
The orientation of the ACL ligament was quantitatively evaluated by measuring the ACL angle and the Blumensaat angle. The ACL angle (Fig. 1a) is the angle formed by the intersection of two lines: one tangential to the anterior aspect of the distal portion of the ACL and the other tangential to the most anterior aspect of the intercondylar eminence and perpendicular to the long axis of the tibia, as seen on a midsagittal MRI image. The Blumensaat angle (Fig. 1b) is the angle formed by the intersection of a line tangential to the anterior aspect of the distal portion of the ACL and a second line tangential to the intercondylar roof. By convention angles with proximal vortexes are considered negative and those with distal vortexes positive. A third quantitative parameter evaluated in the study was the posterior cruciate ligament (PCL) angle (Fig. 1c), formed by two lines tangential to the proximal and distal portions of the PCL. These three quantitative parameters were measured in both groups of patients, and appropriate threshold values were statistically determined. Those patients in whom the torn ACL could not be identified at all on the sagittal plane of the corresponding MRI examination were not included in the study. Those patients in whom the entire PCL could not be identified on a single sagittal image were also discarded.
Diagrams demonstrating angle measurements. a The ACL angle was the angle formed by the intersection of two lines: one tangential to the anterior aspect of the distal portion of the ACL (thick dotted line), and the other tangential to the most anterior aspect of the intercondylar eminence and perpendicular to the long axis of the tibia (thick dotted line), as seen on a midsagittal MRI image. b The Blumensaat angle was the angle formed by the intersection of a line tangential to the anterior aspect of the distal portion of the ACL (thick dotted line) and a second line tangential to the intercondylar roof (thin dotted line). c The PCL angle is formed by two lines tangential to the proximal and distal portions of the PCL respectively (thin and thick dotted lines)
Evaluation of nonquantitative findings
Various nonquantitative MRI signs were evaluated in both groups of patients, including ACL abnormalities, secondary findings, and associated injuries. The ACL was considered normal on MRI when it was present as a continuous band of intermediate signal on PD- and T2-weighted images. The ACL was considered torn when one or more ACL abnormalities were found, including nonvisualization, discontinuity, abnormal signal intensity, and focal or diffuse thickening. Nonvisualization was determined when the ACL could not be visualized in the coronal or axial planes. As noted above, those patients in whom the ACL could not be identified on the sagittal images were not included in the study. Discontinuity was defined as a focal gap in the ligament, regardless of whether the alignment of the distal portion was altered, found in at least two different imaging planes. Abnormal signal intensity was defined as focal or diffuse increased signal intensity on PD- and T2-weighted images within the ligament. Focal or diffuse thickening was defined whenever the thickness of the ACL was not uniform or was 7 mm or greater.
Various secondary findings were evaluated in both groups of patients, including the PCL line sign, anterior tibial displacement, bone bruises, osteochondral injuries, and avulsion fractures. The PCL line sign was considered positive when a line tangential to the posterior aspect of the distal portion of the PCL failed to intersect with the medullar cavity of the femur within its distal 5 cm. Anterior tibial displacement was considered positive if the distance between two lines parallel to the long axis of the tibia, one tangential to the posterior margin of the lateral femoral condyle and the other tangential to the posterior aspect of the lateral tibial plateau, exceeded 5 mm. These two secondary findings were considered nonquantitative parameters because, with adequate training, we were able to interpret the feature without using rulers or scales. The presence of bone bruises in the posterolateral tibial plateau, the lateral femoral condyle, or both was evaluated on the fat-saturated PD-weighted axial and coronal MRI images, and recorded as a single parameter. Accentuated lateral femoral notch and chondral or subchondral lesions other than bone bruises were recorded as osteochondral injuries. Segond fractures and other avulsion fractures (particularly avulsion fractures of the intercondylar eminence) were recorded separately.
Finally, associated injuries were evaluated in the MRI studies of all patients, including evaluation of medial or lateral meniscal tears and medial or lateral collateral ligamentous lesions.
Statistical analyses
ACL abnormalities, secondary findings, and associated injuries as seen on MRI were compared for their association with ACL tears. For descriptive analysis, quantitative parameters were evaluated by calculating the mean and standard deviation, and categorical parameters were evaluated by obtaining absolute and relative frequencies. The most suitable threshold values for the quantitative parameters were calculated with univariate logistic regression analysis. The sensitivity and specificity of all parameters were determined. Odds ratio and their 95% confidence intervals were also calculated by logistic regression analysis. Statistical analyses were all performed with commercially available software (SPSS 6.1).
Results
Table 1 summarizes the results of evaluating quantitative parameters, ACL abnormalities, secondary findings, and associated injuries as seen on MRI of patients with and without ACL tear. Table 2 summarizes the results of the quantitative study. All patients with torn ACL were positive for one of the quantitative parameters: 4 were positive on one parameter, 13 on two, and 33 on three. In patients with torn ACL the ACL angle averaged 25.9±6.7° (range 10–43), the Blumensaat angle 21.4±11.2° (−7 to 41), and the PCL angle 111.5±17.6° (76–152). In patients with intact ACL the ACL angle averaged 53.5±3.7° (48–64), the Blumensaat angle −8.2±6.5° (−22 to 6), and the PCL angle 128.9±14.3° (95–166).
Once these measurements had been obtained, they were analyzed statistically to determine the most appropriate threshold values for identifying torn ACLs. These were found to be 45° for the ACL angle, 0° for the Blumensaat angle and 115° for the PCL angle. A threshold of 45° for the ACL angle gave optimal statistical results: all of the 50 patients with torn ACL had an ACL angle of 45° or greater, while all of the 50 patients with normal ACL had an ACL angle less than 45°, with resultant sensitivity of 100% (95% CI: 92.9–100%) and specificity of 100% (92.9–100%). A threshold of 0° for the Blumensaat angle also gave good statistical results: 45 patients (90%) with torn ACL had a Blumensaat angle larger than 0°, while for 36 patients (72%) with intact ACL it was 0° or less, with resultant sensitivity of 90% (78.2–96.7%) and specificity of 98% (89.3–99.9%). Finally, a threshold of 115° for the PCL angle was also found to be appropriate: 35 patients with torn ACL (70%) had a PCL angle of 115° or less, while 41 patients (82%) with intact ACL had a PCL angle larger than 115°, with resultant sensitivity of 70% (55.4%–82.1%), and specificity of 82% (68.6–91.4%).
With regard to ACL abnormalities 47 patients with torn ACL were positive on at least one feature: 29 showed one, 14 two, 4 three, and no patient showed four. Discontinuity was the single most frequent ACL abnormality among the patients with torn ACL, giving a sensitivity of 66% (95% CI: 51.2–79%) and specificity of 100% (92.9–100%). Nonvisualization, abnormal signal intensity, and focal or diffuse thickening were found less frequently in this group of patients but still gave very high specificity for torn ACL. In the group of patients with preserved ACL nonvisualization or discontinuity was not found. In one patient in the control group diffuse increased signal intensity was noted in an otherwise preserved ACL, which was retrospectively interpreted as mucoid degeneration. In a second control group patient focal thickening of the ACL was found at arthroscopy, corresponding to an ACL ganglion cyst which was easily characterized on MRI. The diagnostic value of finding at least two different ACL abnormalities (including nonvisualization, discontinuity, and abnormal signal intensity) for predicting ACL tears reached a sensitivity of 58% (95% CI: 43.2–71.8%) and a specificity of 100% (95% CI: 92.9%, 100%).
A total of 47 patients with torn ACL showed one or more secondary findings on their MRI studies: 14 showed 1, 19 two, 11 three, 2 four, and 1 five (both types of avulsion injuries were considered as a single category). Anterior tibial displacement was much more frequent than the PCL line sign and reached a sensitivity of 74% (95% CI: 59.6–85.4%), although both parameters gave very good specificity (100% and 98%, respectively). With regard to bone bruises 20 patients with torn ACL (40%) had a bone bruise on the posterior aspect of the lateral tibial plateau while 24 (48%) showed a bone bruise on the lateral femoral condyle. Considering both signs as a single imaging feature, the sensitivity of bone bruises for detecting ACL tear was 44% (95% CI: 30–59%) and specificity 100% (92.9–100%). The sensitivity of chondral, osteochondral, and subchondral lesions for ACL tears was 46% (32–61%) and specificity 100% (92.9–100%). The correlation between MRI signs of bone bruise or osteochondral injury and arthroscopic findings was poor: only three osteochondral lesions of the femoral condyle and one impaction fracture of the posterior aspect of the lateral tibial plateau were found at surgery. Avulsion fractures were unusual in our study. Two Segond fractures were found in the group of patients with torn ACL. Another patient in the same group had an avulsion fracture of the intercondylar eminence of the tibia. Avulsion fractures, especially Segond fractures, were found to have low sensitivity for predicting ACL tears, but excellent specificity of 100% (95% CI: 92.9–100%). The diagnostic value of finding at least two different secondary findings for predicting ACL tears reached a sensitivity of 38% (24.7–52.8%) and specificity of 98% (89.3–99.9%).
MRI of patients with torn ACL showed various associated injuries: 10 patients (20%) showed medial meniscal tears and 5 (10%) lateral meniscal tears. Comparison with arthroscopic findings revealed the following: 15 true positives, 76 true negatives, 4 false positives, and 5 false negatives. In the control group MRI revealed 38 medial meniscal tears and 10 lateral meniscal tears in 46 patients; two patients were found to have tears on both menisci. Comparison with arthroscopic results gave the following results: 48 true positives, 49 true negatives, 0 false positives, and 1 false negative (corresponding to one of the three patients with double meniscal lesion). Four control group patients with clinically suspected meniscal tear and unremarkable MRI were operated on, with one each of the following: pathological plica, ACL ganglion cyst, condylar osteochondral lesion, and patellar chondromalacia. The sensitivity and specificity of MRI for detecting meniscal tears in each group was not calculated, as this was not the purpose of the study. With regard to collateral ligamentous injuries seen on MRI 15 patients (30%) showed signs of previous medial collateral ligament sprain, and 3 (6%) signs of previous lateral collateral ligament sprain. No patients in this group showed injuries to both ligaments or to the PCL. There was no clear evidence in any control group patients of medial or lateral collateral ligamentous injury. The resultant sensitivity of meniscal or collateral ligamentous lesions for predicting ACL tears was low and the specificity variable.
Discussion
Previous studies evaluating the diagnostic sensitivity, specificity, and accuracy of MRI for diagnosing ACL tears have yielded generally good but variable results. The discrepancies may be due to minor variations in the use of inclusion criteria, imaging interpretation or statistical analysis. Apart from such controversial issues as the need to mask primary signs if secondary findings are to be accurately evaluated [3] and the need to separate acute and chronic ACL tears [5, 11, 19], the abundance of described MRI features probably reflects the fact that many of them reproduce the same pathogenic mechanism or pathological consequence. In addition, it clearly suggests that primary ACL abnormalities, also called primary signs, may not suffice for accurate diagnosis in all cases.
Quantitative evaluation of MRI aims to determine precise threshold values for various parameters which can be used systematically or selectively to improve diagnostic accuracy [3, 5, 8, 9, 11, 14, 18, 19]. Various MRI-based quantitative parameters have been suggested for diagnosing ACL tears, including the ACL angle, Blumensaat angle, PCL angle or index, and anterior translocation of the tibia. The ACL angle is an objective test for measuring the horizontalization of the distal aspect of the ligament, which is commonly appreciated on MRI images of torn ACL. The Blumensaat angle provides similar information although the reference plane is the intercondylar roof. The PCL angle or index reflects the increased buckling of the PCL, which in turn reflects the anterior translocation of the tibia. Finally, the anterior translocation of the tibia [20] expresses anterior instability, which is one of the paramount clinical features of ACL tears. We decided to consider anterior translocation of the tibia as a nonquantitative parameter because adequate training allowed as assessing this parameter correctly without rulers or scales. Once the three quantitative parameters had been measured in both groups, we statistically determined the most appropriate threshold values (Table 2) and compared our results with previously published data (Table 3). We found the ACL angle to have optimal utility in predicting ACL tears. The diagnostic yield of the Blumensaat angle was also good, while the performance of the PCL angle was significantly worse.
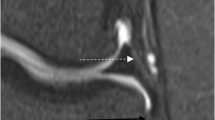
Using the lateral tibial plateau as the reference plane (Table 3), Gentili et al. [5] found that the ACL angle had a sensitivity of 91% and a specificity of 97% in predicting ACL tears. Using the medial tibial plateau, Murao et al. [11] found a sensitivity of 93% and a specificity of 84%. However, both methods of measuring the ACL angle require cumbersome postprocessing, as two different MRI sections are required to draw the reference lines. In this study we evaluated a simplified method for measuring the ACL angle. By adopting as the reference plane the line tangential to the most anterior aspect of the intercondylar eminence, as seen on the same sagittal MRI as the torn ACL (Fig. 1a), we attempted to simplify the measurement of the ACL angle. Using this method and choosing 45° as the most appropriate threshold value, we found that the ACL angle can reach a sensitivity of 100% (95% CI: 92.9–100%) and a specificity of 100% (92.9–100%) for predicting ACL tears. The overlapping of ACL angle values for torn and normal ACL ligaments was minimal (Fig. 2a), which reinforces the utility of the test. Although we were not able to evaluate the inter- and intraobserver variability of the test, we concluded that measuring the ACL angle in this simplified fashion is a sufficiently reliable and objective way for MRI-based quantitative determination of ACL tear, with sensibility and specificity similar to those obtained by other authors utilizing different methods.
Frequency distribution of ACL angles (a), Blumensaat angles (b), and PCL angles (c) in patients with torn (dark line) and normal (grey line) ACL. There is only minimal overlapping of ACL angle values between the two groups of patients (a), while overlapping is moderate for the Blumensaat angle (b) and severe for the PCL angle (c)
The Blumensaat angle has been found to have slightly negative values in normal individuals and becomes positive in torn ACLs (Table 3). Using a threshold value of 9°, Gentili et al. [5] found the Blumensaat angle to have a sensitivity of 91% and specificity of 86% for detecting ACL tears. However, at a threshold value of 15° the sensitivity decreased to 89% and the specificity reached 100% [5]. Using a threshold value of 9.5°, Lee et al. [8] found the angle to have a sensitivity of 94% and specificity of 96%. Our study shows that if the threshold value is greater than 0°, the sensitivity of the Blumensaat angle reaches 90% (95% CI: 78.2–96.7%) and specificity 98% (89.3–99.9%). Although our results indicate that the Blumensaat angle is also very acceptable for predicting ACL tears, it may be slightly worse than the ACL angle in this regard. Values slightly overlapped in the pathological and control groups (Fig. 2b), which hardly happened at all for the ACL angle. Although our threshold value was slightly different, our results agreed with those of previous studies.
The PCL angle has been found to decrease in patients with ACL tears (Table 3). Using a threshold value of 107°, Gentili et al. [5] found that the PCL angle had a sensitivity of 52% and specificity of 94% in predicting ACL tears. Using a threshold of 105°, McCauley et al. [9] found a sensitivity of 72–74% and specificity of 79–86%. Using a threshold value of 114°, Lee et al. [8] found the PCL angle to have a sensitivity of 74% and specificity of 71% for diagnosing ACL tears. The results of our study suggested that 115° may be the optimal threshold value, giving a sensitivity of 70% (55.4–82.1%) and specificity of 82% (68.6–91.4%). In our population the PCL angles significantly overlapped in both groups (Fig. 2c), thus diminishing the utility of the sign. Therefore the diagnostic utility of measuring the PCL angle seems to be significantly worse than measuring the ACL and Blumensaat angle, which is in accordance with previous studies.
Other authors have shown that intrinsic abnormalities in the ACL are the most reliable signs for predicting ligamentous tears [3, 8, 10, 14, 17, 18]. Although quantitative parameters, secondary findings, and associated injuries are worth noting and may increase observer’s confidence, ACL abnormalities are still the mainstay of MRI diagnosis [3]. In our study we evaluated four different ACL intrinsic abnormalities, considering the ACL angle and the Blumensaat angle as quantitative parameters from a different group. The single most useful nonquantitative ACL abnormality was discontinuity, with a sensitivity of 66% (95% CI: 51.2–79%) and specificity of 100% (92.9–100%). Most authors have found discontinuity to be the most useful primary sign, although Lee et al. [8] found it to reach a sensitivity of 21% in the pediatric population. Our own results may reflect the relatively strict criteria that we chose; only discontinuity noted on two different imaging planes was considered to be true discontinuity, which may have had impact on statistical results. We found that abnormal signal intensity and ligamentous thickening to have poor sensitivities, significantly worse than those found by other authors. This may reflect the presumed chronicity of our cases, which could not be demonstrated because of insufficient data. Direct nonvisualization was noted very inconstantly, which also reflected the inclusion criteria: those cases with complete nonvisualization on the three imaging planes were systematically excluded because of the impossibility of performing quantitative analysis.
Secondary findings have been found to improve the accuracy of MRI in predicting ACL tears [3, 5, 9, 10, 12, 13, 14, 15, 16, 17, 18, 19, 20]. We found that anterior tibial displacement was the most useful indicator of ACL tears, with a sensitivity of 74% (95% CI: 59.6–85.4%) and specificity of 100% (92.9–100%), which is in accordance with previously reported data [3, 8, 14, 20]. Paradoxically, the sensitivity and specificity of anterior tibial displacement evaluated in a nonquantitative fashion were better than those found with the PCL angle and the PCL line sign. In our study the PCL line showed very low sensitivity although high specificity. The other secondary findings, including bone bruises, osteochondral injuries, and avulsion fractures, also had variably low sensitivities but very high specificities. With regard to bone bruises, usually considered to be important indirect MRI signs, our poor results may indicate the long-standing nature of many injuries and partly the inconsistency of MRI protocols (owing to the retrospective nature of the investigation and the diverse origin of the studies).
Associated injuries cannot be considered truly useful predictors of ACL tears although they are common findings in MRI knee studies with ligamentous injuries. Previous reports have shown that posterior displacement or uncovering of the posterior horn of the lateral meniscus may be an important ancillary finding of ACL tear [3, 5, 8, 9, 18]. However, we did not evaluate this sign, which may be related to anterior translocation of the tibia.
Our statistical analysis of various combinations of ACL abnormalities and secondary findings revealed that no single association within either of these two categories had a better sensitivity or specificity than the ACL angle. However, ACL abnormalities and secondary findings should always be carefully evaluated and never replaced by simple measurement of quantitative parameters. Secondary findings are still useful, however, because the ACL may not be completely visualized in a single MRI section, which makes it difficult to thoroughly assess in a quantitative fashion. Some anatomical features (the diameter of the intercondylar notch) and volume average effects may make ACL abnormalities more difficult to assess. It should also be remembered that, although measuring the ACL angle may increase diagnostic accuracy, measurement may not always be possible or easy to reproduce.
Our study has several limitations. We did not assess the intraobserver and interobserver agreement of the angle measurements. This may have had some impact in the final outcome. However, the agreement of our results with previously published data seems to suggest that the bias may have been nonsignificant. In addition, we could not determine the exact chronology of the ligamentous injury in many cases, thus making it impossible to distinguish between acute and chronic lesions. This has been said to be relevant, as chronically torn ACLs may scar to the PCL, thus keeping the spatial location normal and giving an abnormally high ACL angle [5, 11]. Finally, we did not compare the results of our best imaging predictor, the ACL angle, with those of physical examination, which remains crucial for clinically diagnosing ACL tears [1].
In conclusion, we have demonstrated that MRI-based quantitative parameters are good predictors for ACL tears and may increase the overall sensitivity and specificity of MRI in this regard. The ACL angle may be confidently measured in a single midsagittal MRI section, and a threshold value of 45° can be considered the single most reliable quantitative parameter for predicting ACL tear in an MRI study.
References
Aglietti P, Buzzi R (1994) Lesiones crónicas del ligamento cruzado anterior. In: Insall (ed) Cirugía de la rodilla, 2nd edn. Panamericana, Madrid
Barberie JE, Carson BW, Finnegan M, Wong AD (2001) Oblique sagittal view of the anterior cruciate ligament: comparison of coronal versus axial planes as localizing sequences. J Magn Reson Imaging 14:203–206
Brandser EA, Riley MA, El-Khoury GY, Bennet DL (1996) MR imaging of anterior cruciate ligament injury: independent value of primary and secondary signs. AJR Am J Roentgenol 167:121–126
Fitzgerald SW, Remer EM, Friedman H, Rogers LF, Hendrix RW, Schafer MF (1993) MR evaluation of the anterior cruciate ligament: value of supplementing sagittal images with coronal and axial images. AJR Am J Roentgenol 160:1233–1237
Gentili AG, Seeger LL, Yao L, Do HM (1994) Anterior cruciate ligament tear: indirect signs at MR imaging. Radiology 193:835–840
Ha TPT, Li KCP, Beaulieu CF, Bergman G, Ch’en IY, Eller DJ, Cheung LP, Herfkens RJ (1997) Anterior cruciate ligament injury: fast spin-echo MR imaging with arthroscopic correlation in 217 examinations. AJR Am J Roentgenol 170:1215–1219
Katahira K, Yamashita Y, Takahashi M, Otsuka N, Koga Y, Fukumoto T, Nomura K (2001) MR imaging of the anterior cruciate ligament: value of thin slice direct oblique coronal technique. Radiat Med 19:1–7
Lee K, Siegel MJ, Lau DM, Hildebolt CF, Matava MJ (1999) Anterior cruciate ligament tears: MR imaging-based diagnosis in a pediatric population. Radiology 213:697–704
McCauley TR, Moses M, Kier R, Lynch JK, Barton JW, Jokl P (1994) MR diagnosis of tears of anterior cruciate ligament of the knee: importance of ancillary findings. AJR Am J Roentgenol 162:115–119
Mink JH, Deutsch AL (1989) Magnetic resonance imaging of the knee. Clin Orthop 244:29–47
Murao H, Morishita S, Nakajima M, Abe M (1998) Magnetic resonance imaging of anterior cruciate ligament (ACL) tears: diagnostic value of ACL-tibial plateau angle. J Orthop Sci 3:10–17
Murphy BJ, Smith RL, Uribe JW, Janecki CJ, Hechtman KS, Mangasarian RA (1992) Bone signal abnormalities in the posterolateral tibia and lateral femoral condyle in complete tears of the anterior cruciate ligament: a specific sign? Radiology 182:221–224
Pao DG (2001) The lateral femoral notch sign. Radiology 219:800–801
Robertson PL, Schweitzer ME, Bartolozzi AR (1994) Anterior cruciate ligament tears: evaluation of multiple signs with MR imaging. Radiology 193:829–834
Schweitzer ME, Cervilla V, Kursunoglu-Brahme S, Resnick D (1992) The PCL line: an indirect sign of anterior cruciate ligament injury. Clin Imaging 16:43–48
Stallenberg B, Gevenois PA, Sintzoff SA, Matos C, Andrianne Y, Struyven J (1993) Fracture of the posterior aspect of the lateral tibial plateau: radiographic sign of anterior cruciate ligament tear. Radiology 187:821–825
Stoller DW, Cannon WD, Anderson LJ (1997) The knee. In: Stoller DW (ed) Magnetic resonance imaging in orthopaedics and sports medicine, 2nd edn. Lippincott-Raven, Philadelphia, pp 311–342
Tung GA, Davis LM, Wiggins ME, Fadale PD (1993) Tears of the anterior cruciate ligament: primary and secondary signs at MR imaging. Radiology 188:661–667
Vahey TN, Broome DR, Kaye KJ, Shelbourne KD (1991) Acute and chronic tears of the anterior cruciate ligament: differential features at MR imaging. Radiology 181:251–253
Vahey TN, Hunt JE, Shelbourne KD (1993) Anterior translocation of the tibia at MR imaging: a secondary sign of anterior cruciate ligament tear. Radiology 187:817–819
Acknowledgements
We express our gratitude to John Bates and the Linguistic Service of the Rovira I Virgili University for their assistance in the preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mellado, J.M., Calmet, J., Olona, M. et al. Magnetic resonance imaging of anterior cruciate ligament tears: reevaluation of quantitative parameters and imaging findings including a simplified method for measuring the anterior cruciate ligament angle. Knee Surg Sports Traumatol Arthrosc 12, 217–224 (2004). https://doi.org/10.1007/s00167-003-0431-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-003-0431-2