Abstract
Purpose
The aim of this study was (1) to compare the clinical and radiological outcomes of robotic and conventional total knee arthroplasty with a minimum follow-up of ten years, (2) to evaluate the survival rate, (3) and to estimate the accuracy of the two techniques by analyzing the outliers of the total knee arthroplasty (TKA) patients.
Methods
We evaluated 351 patients (390 knees), 155 patients undergoing robotic TKA, and 196 patients treated with conventional TKA with a mean follow-up of 11.0 years. HSS, KSS, WOMAC, and SF-12 questionnaires were used for clinical evaluation. Mechanical alignment, implant radiological measurements, and outliers were analyzed for radiological results. Kaplan-Meier survival analysis was performed for survival rate.
Results
All clinical assessments showed excellent improvements in both groups (all p < 0.05), without any significant difference between the groups (p > 0.05). The conventional TKA group showed a significantly higher number of outliers compared with the robotic TKA group (0 < 0.05). The cumulative survival rate was 98.8% in the robotic TKA group and 98.5% in the conventional TKA group with excellent survival (p = 0.563).
Conclusion
Our study showed excellent survival with both robotic and conventional TKA and similar clinical outcomes at long-term follow-up. And, in terms of radiological outcome, robotic TKA showed better accuracy and consistency with fewer outliers compared with conventional TKA. With longer follow-up and larger cohort, the accuracy and effectiveness of robotic TKA on implant survival rate can be elucidated in the future.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Total knee arthroplasty (TKA) is currently the most promising and successful treatment for patients with end-stage knee osteoarthritis worldwide [1, 2]. Appropriate mechanical alignment plays a major role in the success of TKA, implant longevity, survival rate, and patient’s functional performance [3,4,5]. Advances in technology and surgery for improved accuracy of alignment led to the development and utilization of robotic TKA system [6,7,8].
Studies have reported the short-term and midterm results of total knee arthroplasty. A few reports of long-term results of conventional total knee arthroplasty also exist. However, most of them carried a small sample size, with previous generation implants and conflicting results [9,10,11]. Recently, there are some good short-term reports of robotic TKA and also evaluation of accuracy of the ROBODOC system [12, 13]. Studies reported that robotic TKA patients showed improvement in quality-of-life compared to conventional TKA patients in short-term follow-up. Unfortunately, to our knowledge, very few long-term reports compared the efficacy and clinical advantage of robotic TKA. Therefore, scientific evidence underlying long-term results of not only conventional TKA but also robotic TKA is very limited and controversial.
Also, around mid-1990s, the NexGen™ (Zimmer Biomet, Warsaw, IN, USA) implant was introduced with improved kinematics, patellar tracking, and reduced patella-femoral problems compared to previous prostheses [14]. Nexgen™ implant included side-specific design of the femoral component, enhanced lateral flange of the femur, and deepened trochlea. The tibial component was symmetrical between medial and lateral compartments. According to previous good short-term results of Nexgen™ TKA system, our institute adopted the implant and began application to many patients with either robotic TKA or conventional TKA technique.
The aim of this study was (1) to compare the clinical and radiological outcomes of robotic and conventional total knee arthroplasty with a minimum follow-up of ten years using specific implant, (2) to evaluate the survival rate, (3) and to estimate the accuracy of the two techniques by analyzing the outliers of the TKA patients.
Materials and methods
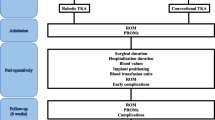
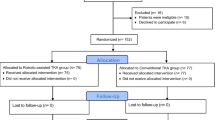
The retrospective randomized study was approved by institutional review board of Chonnam National University Hwasun Hospital and analysis was performed. Between January 2004 and December 2007, we identified consecutive cohorts of patients (1) who underwent primary total knee arthroplasty (2) using a specific total knee system (NexGen™, Zimmer, Inc., Warsaw, IN, USA) (3) with a minimum follow-up of ten years. We identified 508 patients (578 knees) in the cohort, including 203 patients (208 knees) who underwent robotic total knee arthroplasty using ROBODOC® and 305 patients (370 knees) who underwent conventional total knee arthroplasty. During the follow-up, 53 patients were unable to reach their contacts and 104 patients passed away during the follow-up. Finally, the cohort included 155 patients (160 knees) in the robotic TKA group and 196 patients (230 knees) in the conventional TKA group for analysis of long-term results (Fig. 1). The robotic TKA and conventional TKA groups included 110 and 120 patients as outpatients, respectively. A total of 45 of 155 patients in the robotic group and 76 of 196 patients in the conventional group who were unable to revisit the hospital underwent phone interview with the author to determine their current status and satisfactory level. Patients’ basic demographics are shown in Table 1. The mean follow-up duration was 0.4 years longer (p = 0.001) and the proportion of posterior-stabilized (PS) implant was higher in the conventional TKA group compared with the robotic TKA group (p < 0.001). Pre-operative varus deformity in the two groups did not show significant difference (p = 0.386).
Pre-operative planning (plain radiographs and CT evaluation)
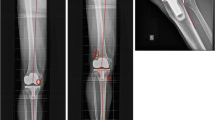
Pre-operatively, all patients underwent standard anteroposterior, lateral radiographic examination, Merchant & Lauren’s view, Rosenberg view, and standing extremity teleoroentgenography. Patients, who were scheduled for robotic TKA, underwent computed tomography (CT) to prepare for ROBODOC® planning. A helical CT scan was performed pre-operatively and transferred to ORTHODOC planning system. Three-dimensional surface remodeling was done for both femur and tibia. Femoral and tibial mechanical axes were identified according to the center of the hip, knee, and ankle. For each knee, component size, position, rotation, and alignment were properly planned for robotic TKA. All surgical procedures were carried out by one senior author (EKS) using either ROBODOC® (Curexo Technology Corp, Fremont, CA, USA)-assisted TKA or conventional TKA using modified-gap balancing technique.
Surgical procedure (ROBODOC®-assisted TKA and conventional TKA)
All knees were exposed with a standard midline incision via medial parapatellar arthrotomy, and the patella was everted laterally. In the ROBODOC®-assisted TKA, the patient’s leg was rigidly connected to the robot and bony landmarks of both femur and tibia were registered using a probe. After the registration was successfully accomplished, bone resection was automatically conducted by ROBODOC® as planned pre-operatively using ORTHODOC system (Fig. 2). Distal femur and proximal tibia were resected perpendicular to the mechanical axis, with 7° of posterior slope to the mechanical axis of the tibia in the sagittal plane. Femoral rotational alignment was planned perpendicular to the transepicondylar axis and the tibial rotational axis was oriented parallel to that of the femur [15]. In conventional TKA, after exposing the knee joint, bone resection was performed via tibia-first modified–gap balance technique. Tibial preparation was carried out using extramedullary cutting guide with proximal tibial resection perpendicular to the mechanical axis with 7° posterior slope. Tibial component rotation was aligned to the line connecting the posterior cruciate ligament insertion site and the medial edge to medial 1/3 of the tibial tuberosity. Distal femoral preparation was carried out by intra-medullary rod guide with 5° of valgus, and femoral rotation was determined according to the balanced flexion gap. After the bone resection, ligament balancing was performed in both groups, including deep medial collateral ligament (MCL) release, posterior capsular release, and sub-periosteal superficial MCL release. The technique involved inserting a commercial tensor device (Stryker Howmedica Osteonics Corp, Allendale, NJ, USA) with the knee in extension as described by Winemaker [16]. The surgeon measured medial and lateral gaps and performed ligament balancing procedure as much as needed to achieve equal medial and lateral gaps to within ± 2 mm. Also, the knee was then flexed to 90°, and rectangular flexion gap was achieved to the extension gap. The operating surgeon’s goal was to create a flexion gap that was greater than the extension gap by 2 mm [17]. When the ligament balancing was completed, femoral and tibial implants were implanted using bone cement.
Post-operative protocols
All patients in both groups underwent post-operative protocols equally. The patients were encouraged to start active and passive knee motion when the pain was tolerable. In addition, patients were encouraged to perform partial weight bearing ambulation using walker. Patients were followed up at the hospital at three, six and 12 months and annually, thereafter. At each visit, clinical and radiological evaluation were performed and recorded.
Clinical evaluations
During the follow-up, the range of motion was evaluated with standard goniometer and the clinical status of all patients was evaluated using Hospital for Special Surgery (HSS) [18], Knee Society score (pain and function) [19], Western Ontario and McMaster Universities (WOMAC) scoring system [20], and Short-Form (SF) 12 questionnaires [21].
Radiological evaluations
Anteroposterior, lateral, and standing radiographs were evaluated pre-operatively and at the final follow-up for alignment and component position. To obtain pre-operative radiological findings, pre-operative measurements were analyzed in all patient cohorts. Patients undergoing only phone interview were excluded from the final follow-up radiological measurements. Final radiographs were evaluated by the author (observer A), one independent orthopaedic surgeon (observer B) and one radiologist (observer C). Hip-knee-ankle (HKA) axis was measured with standing radiograph and for implant position; the coronal and sagittal inclinations of femoral and tibial components (α, β, γ, δ) were measured using anteroposterior and lateral radiographs (Fig. 3). Outliers were defined when the measured angle exceeded ± 3° from the neutral alignment in each radiological measurements on the final follow-up radiograph. The loosening was defined in the presence of progressive radiolucent lines or implant migration. To determine the intra-observer variation, the radiographic measurement was repeated by the author (observer A) after 1 week. To determine the inter-observer variation, the measurements were analyzed by three observers.
Statistical analysis
Means, standard deviations, and frequencies were analyzed, and Student’s t tests or Mann-Whitney U test were used to evaluate the continuous variables, and chi-squared test or Fisher’s exact test was used for categorical variables. Kaplan-Meier survival test was used for survival analysis with revision for any reason as an endpoint. Comparison between the groups was analyzed by log-rank test. Intra-observer consistency between the two sets of radiographic measurements obtained by observer A and inter-observer consistency between the three sets of measurements by observers A, B, and C were analyzed using Pearson’s correlation coefficient. The intra-class correlation coefficient (ICC) > 0.75 was regarded as excellent, ICC 0.40–0.75 was fair to good, and ICC < 0.40 was poor [20]. P value less than 0.05 was considered statistically significant and all statistical analyses were performed using SPSS 24.0 (SPSS, Chicago, IL).
Results
During the follow-up, all functional outcomes (ROM, HSS, KSS, WOMAC score, and SF-12 questionnaires) were significantly improved compared with the pre-operative status in both groups (all p < 0.05). Pre-operatively, ROM was significantly higher in the robotic group (p = 0.009) and KSS pain score was small but also significantly lower in the robotic TKA group (p = 0.008). However, at the final follow-up no significant differences were detected between the two groups based on the clinical outcomes (p > 0.05) (Table 2).
The HKA axis of the knee was significantly improved in both groups (p < 0.05), without any significant difference at final follow-up of the radiological outcomes between the two groups. Femoral and tibial implants were adequately positioned and a significant difference in sagittal inclination of femur was observed between the two groups. The proportion of overall outliers was significantly higher in the conventional TKA group (p < 0.05) and especially conventional TKA in HKA axis and sagittal position of both femoral and tibial implants (p < 0.05) (Table 3). Radiological measurements showed excellent intra-observer consistency and inter-observer consistency across the three observers (Table 4).
A total of eight cases (2.1%) of revision surgery were performed during the follow-up, including two cases (1.3%) in robotic TKA group and six cases (2.6%) in conventional TKA group, without any significant difference (p = 0.480). Both cases of revision involving the robotic TKA group were due to infection, and the robotic group did not show any loosening, polyethylene (PE) wear or instability. Among the six cases of revision involving the conventional TKA group, one was due to infection, two were due to aseptic loosening, two were due to PE wears, and one case due to instability. Infected TKA patients underwent two-stage reconstruction, two patients with aseptic loosening underwent revision TKA involving both femur and tibia, two patients with radiolucent line, and PE underwent insert exchange, and one patient showing instability was converted to constrained type TKA. Fortunately, there were no intra-operative complication during the surgery. All complications were revealed during the long-term follow-up, post-operatively.
The cumulative survival rate of TKA was 98.8% (95% CI, 13.4–13.5 years) in the robotic TKA group and 98.5% (95% CI, 13.6–13.9 years) in the conventional TKA group for any reason (Fig. 4), without any significant difference between the groups (p = 0.563).
Discussion
The study evaluated and compared the long-term results of both robotic and conventional TKA using the specific implant system. We found excellent clinical outcome involving both robotic and conventional TKA with a minimum follow-up of ten years, with no significant difference between two groups. In the present study, good radiological results were also obtained in both groups, and close-to-neutral limb alignment was quite constantly achieved, regardless of pre-operative knee conditions such as mechanical axis, gender, or implant type (CR/PS).
However, our study revealed that the proportion of HKA axis and implant position outliers was significantly higher in the conventional TKA. This result implicates that the consistency of the achieving neutral limb alignment is better in robotic-assisted technique compared to conventional human technique. Also, there are similar reports analyzing the accuracy and consistency of computer-assisted total knee arthroplasty. Chen et al. [22] reported 10% of outliers in navigational total knee arthroplasty compared to 26% in conventional technique; Shi et al. [23] reported 13.4% of outliers in computer-navigated TKA compared to 27.4% in conventional technique with less complication in computer-navigated TKA (4%) compared with conventional TKA (6.5%). Several studies reported that mechanical alignment greater than 3° after TKA and implant malpositioning are crucial factors underlying implant longevity [24,25,26,27,28,29]. Herry et al. [30] also reported that robotic system in unicompartmental knee arthroplasty (UKA) can improve the restitution of the joint-line and Turktas et al. [31] reported the usefulness and good short-term results of robotic system in patellofemoral arthroplasty. Despite the absence of any significant clinical differences in the 10-year follow-up of our study, we carefully suppose that patients undergoing conventional TKA carry a higher risk of failure in the future.
Previously, we reported a prospective randomized study with 30 patients of simultaneous bilateral total knee arthroplasty using ROBODOC®-assisted technique on the one side, and conventional technique on the other side of the knee. After minimum of one year follow-up, the results showed no significant difference in clinical results between the knees, but showed significantly higher accuracy in radiologic results including HKA axis, femoral coronal inclination, and tibial sagittal inclination [32]. In the current study, we evaluated 22 patients (44 TKAs) who underwent bilateral total knee arthroplasty with ROBODOC®-assisted TKA on the one side and conventional TKA on the other side. But, there were no significant difference between the two techniques not only in clinical results but also in radiological results (p > 0.05) (Table 5).
Long-term reports of total knee prosthesis followed up for longer than ten years are also available. Huizing et al. [33] reported a small number of cases with 87% survival of anatomic graduated component (AGC) TKA with 15 to 20 years of follow-up. Bachmann et al. [34] reported 97.7% survival rate of Duracon™ TKA with a mean of 10.9 years of follow-up. Jauregui et al. [35] also reported 99% survival rate of Duracon™ TKA with a mean follow-up of 11 years. Song et al. [36] reported 95% survival rate of E-motion TKA with a mean follow-up of nine years using the navigational TKA technique, and De Steiger et al. [37] reported 4.6% of less revision rate using navigational TKA, compared to the 5.2% revision rate of conventional TKA. Saragaglia et al. [38] also reported good survival rate of 98.7% using navigational TKA with 8.7 years of follow-up.
There were also several other reports of NexGen™ TKA with long-term follow-up. Bistolfi et al. [39] reported 98% survival rate of NexGen™ TKA using mobile bearing prostheses. The study also analyzed the survival rate with revision for any reason as an endpoint in which there were three cases of aseptic loosening and two cases of infection. Schiavone et al. [40] reported 94.7% survival rate with a minimum of 15-years of follow-up using NexGen™ posterior stabilized TKA. Seven failures were reported in which there were two cases of infection and rest cases with instability and aseptic loosening. Kim et al. [41] reported 100% survivorship NexGen™ implant in patients with bilateral TKA at ten years of follow-up using navigational TKA technique, which was an extraordinary result. (Table 6). Overall, our study results using NexGen™ implant with ROBODOC®-assisted technique showed a ten year survival rate of 98.5%, which was also comparable with previous results.
Recently, we also evaluated the ligament balance between the two techniques during total knee arthroplasty using objective orthosensor device. The study revealed that measured resection TKA using ROBODOC® needed more additional ligament balancing procedures compared to the conventional modified-gap balance technique (1.36 and 1.2 per person, respectively) [42]. Although we have not thoroughly recorded ligament balancing procedure in this study cohort, we could carefully assume that more ligament balancing procedure might have been performed in ROBODOC®-assisted TKA group, according to our recent study.
Interestingly, there are also some short-term satisfactory reports of MAKO system (Stryker, Mahwah, NJ) which is another up-to-date robotic technique in total knee arthroplasty. MAKO system is a real-time robotic arm–assisted total knee arthroplasty system which assist the surgeon by providing spatial boundaries and reference information for anatomical structures intra-operatively. And, the surgeon can modify the cutting level and degrees during the surgery according to patients’ specific anatomy and ligament state. Marchand et al. [43] reported that using MAKO system (Stryker, Mahwah, NJ) showed better improvement in short-term pain, physical function, and total satisfaction scores of the patients who underwent robot arm-assisted TKA compared to manual TKA patients. The study showed that mean six months post-operative pain and WOMAC score were better in MAKO TKA patients. In concern of the accuracy, Hampp et al. [44] reported that using robot arm-assisted TKA (RATKA) showed significantly higher accurate bone cuts and implant position compared to conventional TKA. Kayani et al. [45] also reported a prospective cohort study that RATKA patients showed significantly decreased pain, improved early functional recovery, and reduced time to hospital discharge which is crucial to efficacy of the technique, compared to conventional jig–based TKA patients. As this new technique has been introduced recently, long-term results have not been reported yet. But the clinical short-term results were comparable to previous robotic-assisted TKA, which can carefully assume that this new technology, RATKA, could also show positive effects to the patients alike robotic-assisted TKA patients.
The strength of this study is that, to our knowledge, this is the only current study that compared the long-term outcomes between robotic TKA to conventional TKA with a large number of patients. And we also tried to minimize the bias by unifying into one specific implant and excluding various environmental factors.
However, this study also has a few limitations. First, during the long-term follow-up, almost 30% of the patients were lost due to death and loss of contacts, which might have overestimated the survival rate. Second, analysis of the patients with a specific implant system (NexGen™) might not be generalized to other arthroplasty systems. Third, this was a single-centre study treated by a single, which can occur bias. Fourth, for ROBODOC-assisted TKA, both surgeon and patient should be aware of additional radiation risks for pre-operative CT scan and the cost effectiveness of the technique [46]. Compared to conventional technique, relatively higher cost of this technique could make surgeons hesitate to absorb the technique. However, robotic technology have potentially cost-saving role as a more accurate surgical procedure and also with gentle learning curve [47]. Additionally, future research and analysis would be needed to answer whether this technology can justify the additional cost for the patients’ clinical outcome and satisfaction.
Conclusion
Our study showed greater than 98% survival rate with both robotic and conventional TKA and similar clinical outcomes at long-term follow-up. Also, in terms of radiologic outcome, robotic TKA showed better accuracy and consistency with fewer outliers in mechanical axis and sagittal positioning of both femoral and tibial implants compared with conventional TKA. Based on longer follow-up and expansion of the cohort via a multi-centre study, we may be able to elucidate the efficacy of robotic TKA and effects on implant survival rate in the distant future.
References
Attar FG, Khaw FM, Kirk LM, Gregg PJ (2008) Survivorship analysis at 15 years of cemented press-fit condylar total knee arthroplasty. J Arthroplast 23:344–349
Carr AJ, Robertsson O, Graves S, Price AJ, Arden NK, Judge A et al (2012) Knee replacement. Lancet 379:1331–1340
Sharkey PF, Lichstein PM, Shen C, Tokarski AT, Parvizi J (2014) Why are total knee arthroplasties failing today--has anything changed after 10 years? J Arthroplast 29:1774–1778
Fehring TK, Odum S, Griffin WL, Mason JB, Nadaud M (2001) Early failures in total knee arthroplasty. Clin Orthop 392:315–318
Rodriguez JA, Bhende H, Ranawat CT (2001) Total condylar knee replacement: a 20-year follow-up study. Clin Orthop Relat Res 388:10–17
Tingart M, Luring C, Bathis H, Beckmann J, Grifka J, Perlick L (2008) Computer-assisted total knee arthroplasty versus the conventional technique: how precise is navigation in clinical routine? Knee Surg Sports Traumatol Arthrosc 16:44–50
Spencer JM, Chauhan SK, Sloan K, Taylor A, Beaver RJ (2007) Computer navigation versus conventional total knee replacement: no difference in functional results at two years. J Bone Joint Surg (Br) 89:477–480
Dutton AQ, Yeo SJ (2009) Computer-assisted minimally invasive total knee arthroplasty compared with standard total knee arthroplasty. Surgical technique. J Bone Joint Surg Am 91(Suppl 2 Pt 1):116–130
Nakano N, Matsumoto T, Ishida K, Tsumura N, Kuroda R, Kurosaka M (2013) Long-term subjective outcomes of computer-assisted total knee arthroplasty. Int Orthop 37:1911–1915
Tolk JJ, Koot HW, Janssen RP (2012) Computer navigated versus conventional total knee arthroplasty. J Knee Surg 25:347–352
Unwin O, Hassaballa M, Murray J, Harries W, Porteous A (2017) Minimally invasive surgery (MIS) for total knee replacement; medium term results with minimum five year follow-up. Knee 24:454–459
Liow MHL, Goh GS, Wong MK, Chin PL, Tay DK, Yeo SJ (2017) Robotic-assisted total knee arthroplasty may lead to improvement in quality-of-life measures: a 2-year follow-up of a prospective randomized trial. Knee Surg Sports Traumatol Arthrosc 25(9):2942–2951
Liow MH, Chin PL, Tay KJ, Chia SL, Lo NN, Yeo SJ (2014) Early experiences with robot-assisted total knee arthroplasty using the DigiMatch ROBODOC(R) surgical system. Singap Med J 55(10):529–534
Oh KJ, Goodman SB, Yang JH (2011) Prospective, randomized study between insall-burstein II and NexGen legacy with a minimum 9-year follow-up. J Arthroplast 26:1232–1238
Song EK, Seon JK, Yim JH, Netravali NA, Bargar WL (2013) Robotic-assisted TKA reduces postoperative alignment outliers and improves gap balance compared to conventional TKA. Clin Orthop Relat Res 471:118–126
Winemaker MJ (2002) Perfect balance in total knee arthroplasty: the elusive compromise. J Arthroplast 17:2–10
Sugama R, Kadoya Y, Kobayashi A, Takaoka K (2005) Preparation of the flexion gap affects the extension gap in total knee arthroplasty. J Arthroplast 20:602–607
Insall JN, Ranawat CS, Aglietti P, Shine J (1976) A comparison of four models of total knee-replacement prostheses. J Bone Joint Surg Am 58:754–765
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res 248:13–14
Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW (1988) Validation study of WOMAC: a health status instrument for measuring clinical important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol 15:1833–1840
Ware JE Jr, Kosinski M, Keller SD (1996) A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care 34:220–233
Chen JY, Chin PL, Tay DK, Chia SL, Lo NN, Yeo SJ (2014) Less outliers in pinless navigation compared with conventional surgery in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 22(8):1827–1832
Shi J, Wei Y, Wang S, Chen F, Wu J, Huang G, Chen J, Wei L, Xia J (2014) Computer navigation and total knee arthroplasty. Orthopedics 37(1):e39–e43
Choong PF, Dowsey MM, Stoney JD (2009) Does accurate anatomical alignment result in better function and quality of life? Comparing conventional and computer-assisted total knee arthroplasty. J Arthroplast 24:560–569
Jeffery RS, Morris RW, Denham RA (1991) Coronal alignment after total knee replacement. J Bone Joint Surg (Br) 73:709–714
Perillo-Marcone A, Barrett DS, Taylor M (2000) The importance of tibial alignment: finite element analysis of tibial malalignment. J Arthroplast 15:1020–1027
Parratte S, Pagnano MW, Trousdale RT, Berry DJ (2010) Effect of postoperative mechanical axis alignment on the fifteen-year survival of modern, cemented total knee replacements. J Bone Joint Surg Am 92:2143–2149
Ishida K, Matsumoto T, Tsumura N, Kubo S, Kitagawa A, Chin T et al (2011) Mid-term outcomes of computer-assisted total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 19:1107–1112
Gøthesen O, Espehaug B, Havelin LI, Petursson G, Hallan G, Strøm E et al (2014) Functional outcome and alignment in computer-assisted and conventionally operated total knee replacements: a multicentre parallel-group randomised controlled trial. Bone Joint J 96-B:609–618
Herry Y, Batailler C, Lording T, Servien E, Neyret P, Lustig S (2017) Improved joint-line restitution in unicompartmental knee arthroplasty using a robotic-assisted surgical technique. Int Orthop 41(11):2265–2271
Turktas U, Piskin A, Poehling GG (2016) Short-term outcomes of robotically assisted patello-femoral arthroplasty. Int Orthop 40(5):919–924
Song EK, Seon JK, Park SJ, Jung WB, Park HW, Lee GW (2011) Simultaneous bilateral total knee arthroplasty with robotic and conventional techniques: a prospective, randomized study. Knee Surg Sports Traumatol Arthrosc 19(7):1069–1076
Huizinga MR, Brouwer RW, Bisschop R, van der Veen HC, van den Akker-Scheek I, van Raay JJ (2012) Long-term follow-up of anatomic graduated component total knee arthroplasty: a 15- to 20-year survival analysis. J Arthroplast 27:1190–1195
Bachmann M, Bolliger L, Ilchmann T, Clauss M (2014) Long-term survival and radiological results of the Duracon™ total knee arthroplasty. Int Orthop 38:747–752
Jauregui JJ, Cherian JJ, Pierce TP, Beaver WB, Issa K, Mont MA (2015) Long-term survivorship and clinical outcomes following total knee arthroplasty. J Arthroplast 30:2164–2166
Song EK, Agrawal PR, Kim SK, Seo HY, Seon JK (2017) A randomized controlled clinical and radiological trial about outcomes of navigation-assisted TKA compared to conventional TKA: long-term follow-up. Knee Surg Sports Traumatol Arthrosc 24(11):3381–3386
De Steiger RN, Liu YL, Graves SE (2015) Computer navigation for total knee arthroplasty reduces revision rate for patients less than sixty-five years of age. J Bone Joint Surg (Am) 97(8):635–642
Saragaglia D, Sigwalt L, Gaillot J, Morin V, Rubens-Duval B, Pailhé R (2017) Results with eight and a half years average follow-up on two hundred and eight e-motion FP® knee prostheses, fitted using computer navigation for knee osteoarthritis in patients with over ten degrees genu varum. Int Orthop 42(4):799–804
Bistolfi A, Lee GC, Deledda D, Rosso F, Berchialla P, Crova M, Massazza G (2014) NexGen LPS mobile bearing total knee arthroplasty: 10-year results. Knee Surg Sports Traumatol Arthrosc 22:1786–1792
Schiavone Panni A, Falez F, D'Apolito R, Corona K, Perisano C, Vasso M (2017) Long-term follow-up of a non-randomised prospective cohort of one hundred and ninety two total knee arthroplasties using the NexGen implant. Int Orthop 41:1155–1162
Kim YH, Park JW, Kim JS (2017) The clinical outcome of computer-navigated compared with conventional knee arthroplasty in the same patients: a prospective, randomized, double-blind, long-term study. J Bone Joint Surg (Am) 99(12):989–996
Cho KJ, Seon JK, Jang WY, Park CG, Song EK (2018) Objective quantification of ligament balancing using VERASENSE in measured resection and modified gap balance total knee arthroplasty. BMC Musculoskelet Disord 19(1):266–276
Marchand RC, Sodhi N, Khlopas A, Sultan AA, Harwin SF, Malkani AL, Mont MA (2017) Patient satisfaction outcomes after robotic arm-assisted total knee arthroplasty: a short-term evaluation. J Knee Surg 30(9):849–853
Hampp EL, Chughtai M, Scholl LY, Sodhi N, Bhowmik-Stoker M, Jacofsky DJ, Mont MA (2018) Robotic-arm assisted total knee arthroplasty demonstrated greater accuracy and precision to plan compared with manual techniques. J Knee Surg. https://doi.org/10.1055/s-0038-1641729
Kayani B, Konan S, Tahmassebi J, Pietrzak JRT, Haddad FS (2018) Robotic-arm assisted total knee arthroplasty is associated with improved early functional recovery and reduced time to hospital discharge compared with conventional jig-based total knee arthroplasty. Bone Joint J 100-B(7):930–937
Swank ML, Alkire M, Conditt M, Lonner JH (2009) Technology and cost-effectiveness in knee arthroplasty: computer navigation and robotics. Am J Orthop (Belle Mead NJ) 38(2 Suppl):32–36
Lonner JH, Smith JR, Picard F, Hamlin B, Rowe PJ, Riches PE (2015) High degree of accuracy of a novel image-free handheld robot for unicondylar knee arthroplasty in a cadaveric study. Clin Orthop Relat Res 473(1):206–212
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The retrospective randomized study was approved by institutional review board of Chonnam National University Hwasun Hospital and analysis was performed
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Rights and permissions
About this article
Cite this article
Cho, KJ., Seon, JK., Jang, WY. et al. Robotic versus conventional primary total knee arthroplasty: clinical and radiological long-term results with a minimum follow-up of ten years. International Orthopaedics (SICOT) 43, 1345–1354 (2019). https://doi.org/10.1007/s00264-018-4231-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-018-4231-1