Abstract
Purpose
The purpose of this study was to examine the radiological features of hinge fracture occurring at the distal medial femoral cortex in knees undergoing biplanar lateral closed-wedge distal femoral osteotomy (LCW-DFO) in double-level osteotomy (DLO) based on pre- and postoperative CT image analyses. It was hypothesised that medial hinge fractures in LCW-DFO would occur with a similar incidence to that in high tibial osteotomy, and its occurrence would affect the clinical/radiological outcomes and induce unintended change in alignment depending on the fracture type (direction of the fracture).
Methods
A consecutive series of 36 knees (31 patients) with primary varus osteoarthritis undergoing DLO comprised the study population. The mean age at surgery was 62.0 ± 5.9 years. Presence of hinge fracture was assessed on radiographs and CT images at 1 week. The fracture type was classified depending on the direction of the fracture line: crack propagation in line with the osteotomy (type 1) and fractures extending proximally (type 2) or distally (type 3) from the tip of the wedge. Computer-assisted assessments of bony limb alignment and bony geometry were conducted on a full-length weight-bearing radiograph and CT images using image analysis software. In addition, subjective clinical results were evaluated using the Knee Injury and Osteoarthritis Outcome Score (KOOS). Radiological and clinical follow-up results at 1 and 2 years were compared to the preoperative data, while comparative analysis was made between the subjects with and without a hinge fracture.
Results
Postoperative image examinations revealed type 1 and 2 medial femoral hinge fractures in 4 and 7 knees, while no type 3 fracture was identified in the study population. Consequently, the overall incidence of the hinge fracture was 30.6% (11 of the 36 knees). Four of those 11 fractures (36.4%) could not be detected on plain radiographs. CT image analysis for three-dimensional bony geometry showed greater increase in internal rotation of the distal bony segment (increased femoral antetorsion by 9.5° on average) after surgery compared to the knees without a hinge fracture (P = 0.01). Clinical evaluation using the KOOS at 2 years showed no significant difference between the groups with and without hinge fractures.
Conclusion
In LCW-DFO, medial femoral hinge fractures occurred in 30.6% of the cases. Knees with type 1 hinge fracture exhibited significantly greater increase in femoral antetorsion as compared to those without hinge fracture. In this case series, postoperative weight-bearing protocol was delayed for knees with hinge fracture. Consequently, surgical results were not affected by the occurrence of hinge fracture for up to 2 years.
Level of evidence
IV (case series)
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Osteotomy around the knee is a well-established and commonly adopted surgical option for knees with uni-compartmental osteoarthritis [4, 26, 39, 42, 45]. There are several surgical options for the mode and the level of osteotomies. Among those, correction by a single-level isolated high tibial osteotomy (HTO) in knees with severe varus deformity has been shown to result in non-anatomical joint line obliquity which induces subsequent problems such as increased shear force at the cartilage [1, 3, 13, 31, 34, 35, 38, 42, 46, 48]. Double-level osteotomy (DLO) combining a lateral closed-wedge distal femoral osteotomy (LCW-DFO) [5, 9] and a medial open-wedge high tibial osteotomy (MOW-HTO) [15, 26, 45] was introduced with the intent to anatomically reconstruct the bony geometry and limb alignment [1,2,3, 31, 38]. In recent years, development of minimally invasive osteotomy techniques with improved surgical instruments has reduced the rate of operative complications and expanded its indication [27, 39, 50]; however, there are still some complications associated with the procedure. Hinge fracture is among those problems which may impair the surgical outcomes.
Hinge fractures in open-wedge osteotomy were documented by Takeuchi et al. [47] for fractures around the lateral tibial cortex in MOW-HTO. They classified this fracture depending on the direction of the fracture and showed that the fracture extending distally to the osteotomy induced subsequent complications such as delayed union and correction loss. Subsequent to this report, there have been a number of papers dealing with lateral hinge fractures after MOW-HTO [12, 20, 22,23,24, 44]. However, there is a paucity of relevant information for CW-DFO [8, 21, 32]. Moreover, previous relevant studies reporting clinical consequences of the hinge fracture were focused on bony healing and coronal plane alignment in plain radiographic examination, though rotational malalignment of the lower limb on the axial plane has been also shown to substantially influence the biomechanical environment in the knee [5, 9, 18, 25].
In this study, pre- and postoperative CT examinations were included in the analytical measures, which enabled accurate assessments of fracture line and three-dimensional alignment. The purpose of this study was to examine the radiological features of hinge fractures occurring at the distal medial femoral cortex in knees undergoing LCW-DFO in DLO based on CT image analyses. It was hypothesised that medial hinge fracture would be identified after MOW-DFO with a similar incidence to that in HTO, and its occurrence would affect the clinical/radiological outcomes and induce unintended change in alignment depending on the fracture type (direction of the fracture).
Patients and methods
Study population
A consecutive series of knees with severe varus osteoarthritis (more than 10° of varus) that met our surgical indication and underwent DLO during the study period from January 2014 to August 2017 were initially included in the study. The patients were followed up for a minimum of 2 years. During the process of data acquisition, subjects without complete radiological/clinical data set were excluded from the study population. The design of this study was approved by the Review Board of Hyogo College of Medicine (No. 2218).
Surgical indication and planning
Among various osteotomy options, DLO was adopted when there were combined varus deformities both in the distal femur and the proximal tibia. At preoperative surgical planning using digital planning software (mediCAD, Hectec, Germany), first, the mechanical lateral distal femoral angle (mLDFA, normal value; 85°–90°), the mechanical medial proximal tibial angle (mMPTA, normal value; 85°–90°) and the joint line convergence angle (JLCA, normal value; 0°–2°) [33] were measured. Then, surgical simulation was initiated with isolated MOW-HTO. During the simulation and planning of the osteotomy, the intended mechanical tibiofemoral angle (mTFA) was set to 1° (a slightly valgus position) corresponding to %weight-bearing line of 52% [31]. If the predicted mMPTA in the surgical simulation was 95° or greater (or the wedge size was 15 mm or greater), then DLO was considered as an option and surgical planning for DLO was conducted accordingly [30, 31].
Surgical procedure
All surgeries were performed by the first author (H.N.). Detailed descriptions of our surgical procedures have been made in our previous paper [30]. DLO was performed using a minimally invasive biplanar osteotomy technique combined with a locking compression plate (LCP) fixation. The osteotomy procedure was conducted under fluoroscopic control following the technique developed by a working group from the Netherlands organized by van Heerwaarden [11]. The femoral osteotomy was conducted first using the minimally invasive plate osteosynthesis (MIPO) technique [27, 50]. The TomoFix medial distal femur (MDF) anatomical plate (DePuy Synthes, Solothurn, Switzerland) originally designed for the contralateral femur was bent according to the individual’s anatomy and used for fixation. Subsequently, the surgery was completed with MOW-HTO via a technique which was previously described by Lobenhoffer and Staubli [26, 30, 42, 45].
Postoperative rehabilitation
The operated knee was not immobilised after surgery. Range of motion exercise was initiated on the following day as tolerated. Partial weight-bearing with one third of body weight using crutches was allowed at 3 weeks with progression to full weight-bearing at 4 weeks. If a hinge fracture was identified in postoperative imaging examination, full weight-bearing was delayed and not permitted until after callus formation of the hinge fracture site was identified [29].
Postoperative follow-up
Postoperative follow-up evaluations were periodically performed every 3 months within a year and then every 6 months afterwards. Comprehensive radiological and clinical evaluations were conducted at 1 year and 2 years, and the results were compared to the preoperative status. The first author (H.N.) performed the periodical clinical and radiological follow-up examinations.
Data acquisition
A non-weight-bearing radiograph was taken at 1 week after surgery, and the presence of hinge fractures in the distal femur was assessed on anteroposterior radiograph. In addition, CT examination was performed on all knees preoperatively and at 1 week post-operation with the informed consent of each patient and the patient’s family. CT images were acquired using a 256-slice multidetector CT scanner (SOMATOM Definition Edge, Siemens Healthineers, Erlangen, Germany), and sequential images from the hip joint to the ankle joint were obtained with a 0.7-mm slice thickness, 40-cm field of view, and 512 × 512 matrix (pixel size: 0.78 mm).
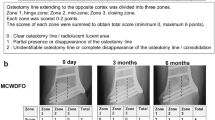
Classification of the hinge fractures
Evaluation of hinge fractures was made on coronal CT images around the femoral osteotomy site. If the fracture line extending from the end of the osteotomy breached the medial femoral cortex, the diagnosis of a medial femoral hinge fracture was made. Based on the orientation of the fracture line, the following classification was made: type 1, a fracture extending to the medial cortex in line with the osteotomy; type 2, a fracture breaching the medial cortex proximally to the osteotomy line (Fig. 1); and type 3, a fracture extending distally from the osteotomy.
Evaluation of the alignment and bony geometry
Radiological parameters of the limb alignment and bony geometry were measured on a long-leg weight-bearing radiograph using an image analysis software (mediCAD®, Hectec, Germany) [43]. Radiographic examinations for measurement of those parameters were conducted preoperatively and at 1 and 2 years after surgery.
Measurement of femoral torsion
After extracting the Digital Imaging and Communications in Medicine (DICOM) data from the Picture Archiving and Communication System (PACS) software, the CT image data were imported into ZioCube imaging software (Ziosoft Inc, Japan) for measurement of femoral torsion. The femoral torsion was measured following the Waidelich method [40, 51]. First, the axial images of the femoral head and the trochanter, as well as the femoral condyle, were selected. The proximal joint line was defined through centres of circle/ellipses of the femoral head and the greater trochanter; while, the distal reference line was defined as the tangent line to the posterior edges of the lateral/medial femoral condyles. The angle between the proximal and distal reference lines was used to measure femoral torsion.
To match the three-dimensional orientation of the preoperative image with that of the postoperative image, a longitudinal axis of the femur was established in three-dimensional CT images and used as a reference axis (Fig. 2). In addition, the level of the slice showing the same bony contour and geometry was selected for the comparative analysis at the two time periods.
Matching of pre- and postoperative CT images. a The axial centre of the femoral shaft is identified on the axial images at two levels of the proximal femur. b, c The longitudinal axis of the femur is established by connecting the two axial centre points on coronal and sagittal planes. d, e In order to match the three-dimensional orientation of the preoperative image with that of the postoperative image, one of the images at the two time periods is rotated around the centre of the femoral head on coronal and sagittal planes until matching of the longitudinal axis is achieved
Reliability of the CT measurement was assessed via intraclass correlation coefficients (ICC). In assessment of the intra- and interrater reliabilities, the images of 10 randomly selected subjects were subjected to the analysis. Repeated measurements by a rater with one-week time interval as well as independent measurements by 2 raters (S.K. and R.U.) were conducted. Consequently, high ICC values of more than 0.9 were demonstrated for both analyses. Based on the high repeatability confirmed by the reliability analysis, measurement results derived from a single rater’s assessment (S.K.) were adopted in the study.
Clinical outcome evaluation
Clinical outcome was evaluated using the validated patient-reported outcome measure, Knee Injury and Osteoarthritis Outcome Score (KOOS) [7, 37]. The evaluations were conducted at 1 and 2 years after surgery and the per- and postoperative results were statistically compared.
Statistical analysis
Changes from the preoperative to postoperative parameter values in each group were statistically assessed using the Mann–Whitney’s U test, while comparison among the three groups was analysed using one-way ANOVA with post hoc Turkey’s test. Statistically significant level was set at P < 0.05.
A power analysis was conducted using STATA for comparison of the femoral torsion values between the groups. The analysis was conducted using the mean and SD values derived from this study. Femoral torsion angle was adopted as the primary outcome measure. The sample size in the comparative group was assumed to be equal. Consequently, it was shown that 12 subjects in each group would be necessary to detect the significant difference using the two-sided test at a power of 90% and P < 0.05.
Results
Study population
A consecutive series of 55 knees in 42 patients who underwent DLO in our institute between January 2014 and August 2017 were initially enrolled in the study. Among those, 19 knees in 11 patients were subsequently excluded from the analysis due to the lack of complete image data set, leaving 36 knees in 31 patients as subjects for the data analyses of the present study. The study population comprised of 6 males and 25 females, and the mean age of the included patients was 62.0 ± 5.9 years (range 54–75 years). Clinical follow-up data of more than 2 years after surgery were available for all 31 patients with the mean follow-up period of 37.0 ± 5.0 months (range 30–46 months).
Occurrence of hinge fractures
In the 36 included knees, type 1 and 2 medial hinge fractures were identified in 4 and 7 knees, respectively; while no type 3 fracture was encountered in this case series. Consequently, the overall incidence among the study population was 30.6% (11 of the 36 knees). Hinge fractures could not be detected on plain radiograph in 1 of the 4 type 1 and 3 of the 7 type 2 fractures. Therefore, in total, plain radiograph failed to reveal 4 of the 11 hinge fractures with a diagnostic failure rate of 36.4% (Fig. 3).
Radiological results
Bony union was uneventfully attained in all knees, though the postoperative time period for full weight-bearing was delayed in patients with hinge fractures. As shown in Table 1, radiological measurements at 1- and 2-year follow-up evaluations showed restoration of normal knee alignment and bony geometry with the mean mTFA and mLDFA corrected to normal ranges. Restoration of normal limb alignment and bony geometries was achieved in both of the groups with and without hinge fractures, and the occurrence of hinge fractures did not affect the radiological outcomes in either type 1 or type 2 hinge fracture groups.
In the CT examinations for rotational on the axial plane, the mean preoperative torsion of the femur in the total study population was 28.7° ± 9.5° (range 7.6°–56.9°). After the osteotomy, the bony segment distal to the osteotomy exhibited a small increase in internal torsion with the mean increase of 1.6° ± 2.8° (range 4.1° external rotation–6.2° internal rotation) in knees without hinge fractures. In knees with a type 1 hinge fracture, the distal segment was internally rotated (femoral torsion was increased) by 9.5° ± 8.0° on average (range 2.8°–20.8° internal rotation), which was significantly larger than that in knees without hinge fractures (P = 0.01). In knees with a type 2 hinge fracture, internal rotation of the distal segment increased by 3.1° ± 5.4° on average (range 3.4° external rotation–6.2° internal rotation) without significant difference in postoperative rotational change compared to the knees with no hinge fracture (P = 0.51) (Table 2).
Clinical results
During the study period, no intra- and early postoperative complications requiring additional management were encountered, except for hinge fractures. A hinge fracture in one case was managed with additional fixation using a medial support plate for augmentation of fixation stability.
Clinical outcomes using the KOOS significantly improved after surgery in both groups with and without hinge fractures. The occurrence of hinge fractures did not affect the clinical outcomes in either type 1 or type 2 hinge fracture groups (Table 3).
Discussion
The most important finding in the present study is that the medial femoral hinge fracture occurred in 30.6% of the knees undergoing LCW-DFO. Furthermore, we described two types of hinge fractures based on the location of breaching within the medial femoral cortex. The fracture line extended in line with the osteotomy in type 1 fractures, while type 2 fractures breached the femoral cortex proximally to the osteotomy. When the hinge fracture was identified, postoperative weight-bearing protocol was delayed in this case series. Consequently, no significant differences in clinical and radiological outcomes were noted between the knees with and without hinge fractures. In knees with type 1 fracture, however, significant rotational change at the osteotomy site was noted on postoperative CT evaluation.
A lateral tibial hinge fracture as a complication of MOW-HTO has been reported in a number of studies [12, 20, 22,23,24, 26, 44, 47]. The overall incidence of hinge fractures following LCW-DFO in this case series (30.6%) was similar to that reported in those previous studies. Takeuchi et al. classified the hinge fracture in MOW-HTO depending on the direction of the fracture line (proximal, in line with the osteotomy, and distal) [47]. In the present series, the hinge fracture extending distally toward the articular surface which corresponds to Takeuchi type III fracture was not encountered. Presence of compliant cancellous bone with a substantial thickness in the femoral condyle may have served as an intervening barrier to prevent the distal extension of the fracture to in LCW-DFO.
As clinical consequences of the hinge fracture, subsequent problems such as over- or under-correction [29, 47] and delayed bone healing [29, 41] were reported in MOW-HTO. In the present study for LCW-DFO, however, the occurrence of hinge fractures did not affect the postoperative outcomes. In this case series, weight-bearing in the postoperative rehabilitation programme was delayed for knees with the hinge fracture and this management modification may have been a factor which effectively avoided the unfavourable sequence.
Although the clinical outcomes were not affected by the hinge fracture, CT evaluation showed increased internal rotation of the distal femoral bony segment (increased femoral antetorsion), especially in knees with type 1 fracture. The fracture plane in the type 1 fracture is extension of the osteotomy plane and flat, and thus, resistance to rotational motion is thought to be small. Previous cadaveric studies have shown that increased femoral antetorsion induced valgus deviation of the mechanical axis [5, 18]. In addition, biomechanical studies have shown that internal rotation of the distal femur results in increased patellofemoral contact stress [9, 25]. In total knee arthroplasty, internal rotation of the femoral component causes several unfavourable sequelae such as patellar maltracking and non-physiologic flexion kinematics [14, 17, 28, 36, 49]. Therefore, rotation at the osteotomy site as observed in this study may alter the mechanical environment in the knee, potentially affecting the surgical outcomes. Further follow-up study is required to clarify long-term consequence of the rotational malalignment.
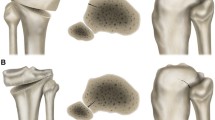
As regards prevention of the hinge fracture, its aetiology should be considered. Regarding the surgical factor, bony cut beyond the hinge point may lead to type 1 fracture; while, inadequate cut (mostly at the posterior cortex) with forceful wedge closing may cause type 2 fracture. To prevent the occurrence of hinge fractures, surgeons should carefully check the extent of osteotomy through inspection and fluoroscopic control during surgery. Previous papers dealing with hinge fractures in medial CW-DFO, other factors such as clearance of the gap following wedge resection, careful and slow wedge closure, and selection of appropriate hinge position (upper border of the femoral condyle rather than supracondylar region) have been listed as surgical knacks for the fracture prevention [21, 32]. Csernátony et al. [8] have proposed a new preventive measure by making an additional juxtacortical drill hole at the end of the osteotomy to reduce the local stress during wedge opening/closing.
As for the rotational change observed for knees with type 1 hinge fracture, it has been reported that osteosynthesis of distal femoral fractures using the MIPO technique is linked to rotational malalignment at a substantially high rate [6, 19]. When occurrence of the hinge fracture is noted during surgery, surgeons should cope with the risk for impaired stability (Fig. 4). Supplemental plate fixation on the medial side as well as close inspection of the fitting between the osteotomy surfaces through wider exposure can be countermeasures to cope with those potential problems. When the hinge fracture was recognised postoperatively, timing of weight-bearing should be delayed to avoid subsequent complications such as delayed bony healing.
There were several limitations included in this study. First, the study population was small, and thus, the study was underpowered. Therefore, type II error in the statistical analysis was likely to occur. Second, there are potential sources of errors included in the comparative CT image analysis for femoral torsion assessment. Although attempts were made to select the pre- and postoperative axial CT images with the same orientation and level, perfect image matching is theoretically not feasible leading to an assessment error. Moreover, the images analysis was conducted by a single observer, though a high ICC value (> 0.9) was confirmed. Third, complete osteotomy cut during surgery may not have been differentiated from type 1 hinge fracture in this series. Fourth, the differences in postoperative rotational change between the groups with and without a hinge fracture was small; thus, its clinical significance is unclear. Further follow-up study for a longer period is warranted. Fifth, we evaluated the hinge fracture by CT and radiograph taken at 1 week after surgery. Therefore, hinge fractures occurring after this time period could not be detected. Finally, there are still some potential factors related to the occurrence of hinge fractures such as bone quality (density) and osteotomy length/inclination that are not analysed in this study. Identification of the risk factors in multiple aspects would help to prevent this complication.
Conclusion
In LCW-DFO, medial femoral hinge fractures occurred in 30.6% of the cases. Knees with type 1 hinge fracture exhibited significantly greater increase in femoral antetorsion as compared to those without hinge fracture. In this case series, postoperative weight-bearing protocol was delayed for knees with hinge fracture. Consequently, surgical results were not affected by the occurrence of hinge fracture for up to 2 years.
References
Babis GC, An KN, Chao EY, Rand JA, Sim FH (2002) Double level osteotomy of the knee: a method to retain joint-line obliquity. Clinical results. J Bone Joint Surg Am 84:1380–1388
Benjamin A (1969) Double osteotomy for the painful knee in rheumatoid arthritis and osteoarthritis. J Bone Joint Surg Br 51:694–699
Benjamin A (1974) Double osteotomy of the knee. Scand J Rheumatol 3:65
Bonnin MP, Laurent JR, Zadegan F, Badet R, Pooler Archbold HA, Servien E (2013) Can patients really participate in sport after high tibial osteotomy? Knee Surg Sports Traumatol Arthrosc 21:64–73
Bretin P, O'Loughlin PF, Suero EM, Kendoff D, Ostermeier S, Hüfner T, Krettek C, Citak M (2011) Influence of femoral malrotation on knee joint alignment and intra-articular contract pressures. Arch Orthop Trauma Surg 131:1115–1110
Buckley R, Mohanty K, Malish D (2011) Lower limb malrotation following MIPO technique of distal femoral and proximal tibial fractures. Injury 42:194–199
Collins NJ, Prinsen CA, Christensen R, Bartels EM, Terwee CB, Roos EM (2016) Knee Injury and Osteoarthritis Outcome Score (KOOS): systematic review and meta-analysis of measurement properties. Osteoarthritis Cartilage 24:1317–1329
Csernátony Z, Kiss L, Manó S (2008) A new technique of wedge osteotomy to diminish undesirable fractures. Eur J Orthop Surg Traumatol 18:485–488
Dagneaux L, Allal R, Pithioux M, Chabrand P, Ollivier M, Argenson JN (2018) Femoral malrotation from diaphyseal fractures results in changes in patellofemoral alignment and higher patellofemoral stress from a finite element model study. Knee 25:807–813
Dorofeev A, Tylla A, Drescher WR, Stangl R (2019) Opposite cortical fractures in closed-wedge HTO: new classification and treatment algorithm. Knee 26:1058–1066
Freiling D, van Heerwaarden R, Staubli A, Lobenhoffer P (2010) The medial closed-wedge osteotomy of the distal femur for the treatment of unicompartmental lateral osteoarthritis of the knee. Oper Orthop Traumatol 22:317–334
Han SB, Choi JH, Mahajan A, Shin YS (2019) Incidence and predictors of lateral hinge fractures following medial opening-wedge high tibial osteotomy using locking plate system: better performance of computed tomography scans. J Arthroplasty 34:846–851
Hernigou P, Duffiet P, Julian D, Guissou I, Poignard A, Flouzat-Lachaniette CH (2013) Outcome of total knee arthroplasty after high tibial osteotomy: does malalignment jeopardize the results when using a posterior-stabilized arthroplasty? HSS J 9:134–137
Heyse TJ, El-Zayat BF, De Corte R, Chevalier Y, Fuchs-Winkelmann S, Labey L (2018) Internal femoral component malrotation in TKA significantly alters tibiofemoral kinematics. Knee Surg Sports Traumatol Arthrosc 26:1767–1775
Hofmann S, Lobenhoffer P, Staubli A, Van Heerwaarden R (2009) Osteotomies of the knee joint in patients with monocompartmental arthritis. Orthopade 38:755–769
Karaman O, Ayhan E, Kesmezacar H, Seker A, Unlu MC, Aydingoz O (2013) Rotational malalignment after closed intramedullary nailing of femoral shaft fractures and its influence on daily life. Eur J Orthop Surg Traumatol 24:1243–1247
Kawahara S, Okazaki K, Matsuda S, Nakahara H, Okamoto S, Iwamoto Y (2014) Internal rotation of femoral component affects functional activities after TKA–survey with the Knee Society Score. J Arthroplasty 29:2319–2323
Kenawey M, Liodakis E, Krettek C, Ostermeier S, Horn T, Hankemeier S (2011) Effect of the lower limb rotational alignment on tibiofemoral contact pressure. Knee Surg Sports Traumatol Arthrosc 19:1851–1859
Kim JW, Oh CW, Of JK, Park IH, Kyung HS, Park KH, Yoon SD, Kim SM (2017) Malalignment after minimally invasive plate osteosynthesis in distal femoral fractures. Injury 48:751–757
Kim KI, Kim GB, Kim HJ, Lee SH, Yoon WK (2018) Extra-articular lateral hinge fracture does not affect the outcomes in medial open-wedge high tibial osteotomy using a locked plate system. Arthroscopy 34:3246–3255
Kim TW, Lee MC, Cho JH, Kim JS, Lee YS (2019) The ideal location of the lateral hinge in medial closing wedge osteotomy of the distal femur: Analysis of soft tissue coverage and bone density. Am J Sports Med 47:2945–2951
Lee BS, Jo BK, Bin SI, Kim JM, Lee CR, Kwon YH (2019) Hinge fractures are underestimated on plain radiographs after open wedge proximal tibial osteotomy: evaluation by computed tomography. Am J Sports Med 47:1370–1375
Lee OS, Lee YS (2018) Diagnostic value of computed tomography and risk factors for lateral hinge fracture in the open wedge high tibial osteotomy. Arthroscopy 34:1032–1043
Lee SS, Celik H, Lee DH (2018) Predictive factors for and detection of lateral hinge fractures following open wedge high tibial osteotomy: plain radiography versus computed tomography. Arthroscopy 34:3073–3079
Liao TC, Yin L, Powers CM (2018) The influence of isolated femur and tibia rotations on patella cartilage stress: a sensitivity analysis. Clin Biomech (Bristol, Avon) 54:125–131
Lobenhoffer P, Agneskirchner JD (2003) Improvements in surgical technique of valgus high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 11:132–138
Lobenhoffer P, Kley K, Freiling D, van Heerwaarden R (2017) Medial closed wedge osteotomy of the distal femur in biplanar technique and a specific plate fixator. Oper Orthop Traumatol 29:306–319
Matsuda S, Miura H, Nagamine R, Urabe K, Hirata G, Iwamoto Y (2001) Effect of femoral and tibial component position on patellar tracking following total knee arthroplasty: 10-year follow-up of Miller-Galante I knees. Am J Knee Surg 14:152–156
Nakamura R, Komatsu N, Murao T, Okamoto Y, Nakamura S, Fujita K, Nishimura H, Katsuki Y (2015) The validity of the classification for lateral hinge fractures in open wedge high tibial osteotomy. Bone Joint J 97:1226–1231
Nakayama H, Iseki T, Kanto R, Kambara S, Kanto M, Yoshiya S, Schröter S (2018) Physiologic knee joint alignment and orientation can be restored by the minimally invasive double level osteotomy for osteoarthritic knees with severe varus deformity. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-018-5103-3
Nakayama H, Schröter S, Yamamoto C, Iseki T, Kanto R, Kurosaka K, Kambara S, Yoshiya S, Higa M (2018) Large correction in opening wedge high tibial osteotomy with resultant joint-line obliquity induces excessive shear stress on the articular cartilage. Knee Surg Sports Traumatol Arthrosc 26:1873–1878
Nha KW, Chang YS, Shon OJ, Shim BJ, Lee JS, Song JS, Bae JH (2019) Where is the target point to prevent cortical hinge fracture in medial closing-wedge distal femoral varus osteotomy? J Knee Surg 32:274–279
Paley D, Herzenberg JE, Tetsworth K, McKie J, Bhave A (1994) Deformity planning for frontal and sagittal plane corrective osteotomies. Orthop Clin North Am 25:425–465
Preston S, Howard J, Naudie D, Somerville L, McAuley J (2013) Total knee arthroplasty after high tibial osteotomy: no differences between medial and lateral osteotomy approaches. Clin Orthop Relat Res 472:105–110
Ramappa M, Anand S, Jennings A (2013) Total knee replacement following high tibial osteotomy versus total knee replacement without high tibial osteotomy: a systematic review and meta-analysis. Arch Orthop Trauma Surg 133:1587–1593
Riley J, Roth JD, Howell SM, Hull ML (2018) Internal-external malalignment of the femoral component in kinematically aligned total knee arthroplasty increases tibial force imbalance but does not change laxities of the tibiofemoral joint. Knee Surg Sports Traumatol Arthrosc 26:1618–1628
Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD (1998) Knee injury and osteoarthritis outcome score (KOOS)–development of a self-administered outcome measure. J Orthop Sports Phys Ther 28:88–96
Saragaglia D, Nemer C, Colle PE (2008) Computer-assisted double level osteotomy for severe genu varum. Sports Med Arthrosc 16:91–96
Schröter S, Ateschrang A, Lowe W, Nakayama H, Stockle U, Ihle C (2015) Early full weight-bearing versus 6-week partial weight-bearing after open wedge high tibial osteotomy leads to earlier improvement of the clinical results: a prospective, randomised evaluation. Knee Surg Sports Traumatol Arthrosc 25:325–332
Schröter S, Elson DW, Ateschrang A, Ihle C, Stöckle U, Dickschas J, Harrer J (2017) Lower limb deformity analysis and the planning of an osteotomy. J Knee Surg 30:393–408
Schröter S, Freude T, Kopp MM, Konstantinidis L, Döbele S, Stöckle U, van Heerwaarden R (2015) Smoking and unstable hinge fractures cause delayed gap filling irrespective of early weight bearing after open wedge osteotomy. Arthroscopy 31:254–265
Schröter S, Gonser CE, Konstantinidis L, Helwig P, Albrecht D (2011) High complication rate after biplanar open wedge high tibial osteotomy stabilized with a new spacer plate (position HTO plate) without bone substitute. Arthroscopy 27:644–652
Schröter S, Ihle C, Mueller J, Lobenhoffer P, Stöckle U, van Heerwaarden R (2013) Digital planning of high tibial osteotomy. Interrater reliability by using two different software. Knee Surg Sports Traumatol Arthrosc 21:189–196
Song KY, Koh IJ, Kim MS, Choi NY, Jeong JH, In Y (2019) Early experience of lateral hinge fracture during medial opening-wedge high tibial osteotomy: incidence and clinical outcomes. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-019-03237-0
Staubli AE, De Simoni C, Babst R, Lobenhoffer P (2003) TomoFix: a new LCP-concept for open wedge osteotomy of the medial proximal tibia–early results in 92 cases. Injury 34:55–62
Strecker W (2006) Planning analysis of knee-adjacent deformities. I. Frontal plane deformities. Oper Orthop Traumatol 18:259–272
Takeuchi R, Ishikawa H, Kumagai K, Yamaguchi Y, Chiba N, Akamatsu Y, Saito T (2012) Fractures around the lateral cortical hinge after a medial opening-wedge high tibial osteotomy: a new classification of lateral hinge fracture. Arthroscopy 28:85–94
Terauchi M, Shirakura K, Katayama M, Higuchi H, Takagishi K, Kimura M (2002) Varus inclination of the distal femur and high tibial osteotomy. J Bone Joint Surg Br 84:223–226
Valkering KP, Breugem SJ, van den Bekerom MP, Tuinebreijer WE, van Geenen RC (2015) Effect of rotational alignment on outcome of total knee arthroplasty. Acta Orthop 86:432–439
Visser J, Brinkman JM, Bleys RL, Castelein RM, van Heerwaarden RJ (2013) The safety and feasibility of a less invasive distal femur closing wedge osteotomy technique: a cadaveric dissection study of the medial aspect of the distal femur. Knee Surg Sports Traumatol Arthrosc 21:220–227
Waidelich HA, Strecker W, Schneider E (1992) Computed tomographic torsion-angle and length measurement of the lower extremity. The methods, normal values and radiation load. Rofo 157:245–251
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have nothing to disclose that could have direct or potential influence or impart bias on the work.
Funding
No external source of funding was used.
Ethical approval
The study was approved by Ethics Committee and judged at Hyogo College of Medicine (reference no. 2218).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nakayama, H., Kanto, R., Onishi, S. et al. Hinge fracture in lateral closed-wedge distal femoral osteotomy in knees undergoing double-level osteotomy: assessment of postoperative change in rotational alignment using CT evaluation. Knee Surg Sports Traumatol Arthrosc 29, 3337–3345 (2021). https://doi.org/10.1007/s00167-020-06197-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-06197-w