Abstract
Purpose
To evaluate the rotational profile of the lower extremity using computed tomography (CT) in accordance with the degree of varus deformity in medial condyle-affected knee joint osteoarthritis (OA).
Methods
This retrospective study included 1036 patients (872 lower extremities) with end-stage knee OA. The coronal alignment of the lower extremity was measured using standing anteroposterior radiography. The CT parameters of femoral anteversion and tibial torsion were assessed in relation to the knee joint. The axes were the femoral neck axis; the distal femoral axis, which was composed of the anterior trochlear axis, the clinical transepicondylar axis, and the posterior condylar axis; the axis of the proximal tibial condyles; and the bimalleolar axis.
Results
There was a tendency for increased external rotation of the knee joint parameters in relation to the hip and ankle joints as varus deformity of the lower extremity increased. The relative external rotational deformity of the knee joint in relation to the hip joint had a positive value with a good correlation. The relative external rotational deformity of the knee joint in relation to the ankle joint also demonstrated a positive value with a good correlation.
Conclusion
The distal femur and proximal tibia (knee joint) tended to rotate externally in relation to the hip and ankle joint, respectively, as the degree of varus deformity increased. This study identified the relationship between lower extremity varus deformity and rotational deformity of knee joints with OA.
Level of evidence
III.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Rotational alignment of the femoral and tibial components is essential for optimal patellar tracking, ligament balancing, and the best functional outcome of total knee arthroplasty (TKA) [12, 28]. Rotational deformity of the lower limb is an important concern because any rotational mismatch of the femoral and tibial components may lead to an increased rate of revision surgery and inferior clinical outcomes [17]. Femoral component malrotation may produce flexion instability, overstuffing, and patellofemoral maltracking [13], while malrotation of the tibial plate may induce a change in the knee kinematics that results in patellofemoral maltracking and incongruencies with the femoral component [27]. Knowledge of rotational deformities is also useful for understanding the aggravating mechanism of osteoarthritis (OA) of the knee joint.
The alignment deformity in knee OA has typically been evaluated using plain radiographs of the hip-knee-ankle or the tibiofemoral angle in the coronal plane. Although the presence of an underlying rotational deformity (relative rotational alignment between the distal femur and the proximal tibia) in OA of the knee joint has been suggested [8, 15, 30], few quantitative data reports are available regarding the relationship of a deformity with an overall lower extremity alignment, specifically the rotational capacity of the knee joint relative to the hip and ankle joints [14, 24]. However, identification of the rotational profile of the lower extremity using plain radiography is challenging due to difficulty in determining the relative positions of the femur neck, distal femur, proximal tibia, and distal tibia. When measurements can be attempted in knees with OA, this difficulty is compounded because anatomic landmarks are usually affected by arthritic changes. This evaluation may be better achieved using three-dimensional imaging techniques, such as computed tomography (CT). Although internal torsion of the femur and external torsion of the tibia have been reported in knees with OA [4, 6, 10, 19], the results obtained thus far regarding the presence of rotational deformity in the tibiofemoral joint are controversial [26, 37]. Increased external rotation of the tibia has been reported, and there has not been a significant difference in knees with OA [4, 6, 10, 19, 26, 37].
The purpose of this study was to evaluate the rotational profile of the lower extremity using CT in accordance with the degree of varus deformity in medial condyle-affected OA of the knee. The rotational profile evaluation should include the relative rotations of the hip, knee, and ankle joints, respectively. The hypothesis was that the external rotational deformity of the knee joint relative to the hip and ankle joints would increase according to the severity of the lower extremity varus deformity. This finding is important in regard to preoperative radiographic planning for prosthetic positions and intraoperative surgical decision-making to determine the appropriate prosthetic alignment as well as the rotational alignment in TKA.
Materials and methods
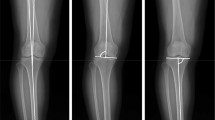
This retrospective study included 1036 non-consecutive patients (872 lower extremities; 456 male and 580 female patients) with end-stage knee OA (Kellgren-Lawrence [18] grades 3 and 4) who underwent TKA (Fig. 1). The study period was between March 2006 and December 2019. The average age at the time of surgery was 73 ± 8 years. The inclusion criteria were a medial compartment affected by end-stage OA with varus deformity. The exclusion criteria were lateral compartment OA, OA with valgus alignment, post-traumatic OA, rheumatic arthritis including other inflammatory arthritis types, and a post-infection state. Patients with flexion contracture greater than 10° were also excluded from the study as their inclusion could result in altered reciprocal rotational position between the femur and tibia [1]. All patients underwent preoperative standing full-limb anteroposterior (AP) radiography and lower extremity axial CT. The demographics and past medical histories of the patients were evaluated by reviewing their medical records (Table 1).
The coronal alignment of the lower extremity was measured using standing AP radiography of the lower extremities. Digital radiography was performed using the DGR-C54J2B (Samsung Electronics Co. Ltd, Suwon, South Korea) DigitalDiagnost Eleva (Philips Medical Systems, Best, The Netherlands) unit. The distance between the patient and the tube was 180 cm, and the image was obtained using radiation amounts of 70–85 kVp for durations of 20–40 mAs and with a 0.25-s exposure time. Three images of the lower extremities were obtained consecutively using a 14- × 17-inch grid standard cassette from the hip joint to the foot level, and the three images were automatically joined to form a composite image within the digital radiography device. Standing AP radiography of the lower extremities was performed with the patients facing the radiographic tube; foot rotation was held constant with a reference foot template on the platform of the radiographic system. In addition, the appropriate knee position, which was defined as a widened stance intended to vertically align the ankle to the femoral heads with the patella facing forward and half of the width of the fibular head being overlapped by the tibial condyle, was confirmed using a preview monitor before the final acquisition of the radiographs [3].
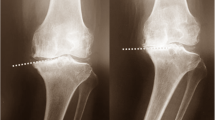
All radiographs were digitally acquired using a picture archiving and communication system viewer (INFINITT PiviewSTAR; Infinitt Healthcare, Seoul, Korea). The lower extremity alignment was determined using the mechanical tibiofemoral angle (mTFA). This angle was defined as the angle formed between the mechanical axis of the tibia and that of the femur (Fig. 2). The mechanical axis of the femur was defined as the line connecting the center of the femoral head and the center of the femoral notch. The mechanical axis of the tibia was defined as the line connecting the point between the medial and lateral tibial spines and the center of the tibial plafond. The mTFA was assigned a negative value when the knee was in varus alignment. The participants were divided into three groups according to the preoperative mTFA varus deformity as follows: neutral (0°) to 5°, between 5° and 10°, and more than 10° of varus deformity [38].
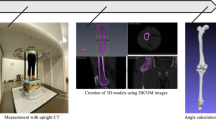
The CT parameters of femoral anteversion and tibial torsion were measured in relation to the knee joint. The lower extremity axial CT scan was obtained using a 64-channel single-source, dual-energy multidetector CT scan (SOMATOM Definition Edge, Siemens Healthcare, Erlangen, Germany). The image acquisition procedure was carried out for the lower extremities while the patients were fixed with a supporting sponge in a state of neutral rotation in a supine and feet-first position with radiation levels of 120 kVp for an effective mAs (20–35 mAs) duration and a 0.3-s rotation time with a detector collimation of 64 × 0.6 mm in 1.0-mm increments at a pitch of 0.8 with an 8–15-s scan time and a 7.24-mGY volume CT dosage index. The axial images were reconstructed into 1.0-mm thick sections taken through the hip, knee, and ankle joints with both limbs in the same position [2, 11].
All radiologic measurements were performed by the authors (RU, JHY) who were familiar with the assessment of the rotation profile of the lower extremities. The axes are the femoral neck axis (A, Fig. 3a) [35]; the distal femoral axis composed of the anterior trochlear axis (B1, Fig. 3b) [25], clinical transepicondylar axis (clinical TEA, B2, Fig. 3c) [39], and posterior condylar axis (B3, Fig. 3d); the axis of the proximal tibial condyles (C, Fig. 3e) [22, 23]; and the bimalleolar axis (D, Fig. 3f) [22, 23]. The relative rotational profile was calculated by defining these angles in relation to the horizontal base line. Internal torsion was assigned a negative (−) sign, while external torsion was assigned a positive (+) sign. Using these six angles, the next step was to calculate the femoral neck anteversion angle, tibial torsion angle, and total limb rotation angle [34]. The degree of femoral neck anteversion was calculated by subtracting the distal femoral angles (anterior trochlear line, clinical TEA, and the posterior condylar line) from the femoral neck angle; the tibial torsion was determined by subtracting the proximal tibial angle from the bimalleolar angle; and the total limb rotation was calculated by simply subtracting the degree of anteversion of the femoral neck from the tibial torsion angle. These six angles were recorded and compared for each patient and each limb. Measurement accuracy was one decimal; all the measured values were rounded up or down to full degrees. The protocol of the present study was approved by the institutional review board of institution (VHS 2020-0601). Informed consent was waived.
Assessment of the rotation profile of the lower extremities (right limb). a Femoral neck axis (A), b anterior trochlear axis (B1), clinical transepicondylar axis (B2) and posterior condylar axis (B3). c The axis of the proximal tibial condyles (C) and d the bimalleolar axis (D). The relative rotational profile was calculated based on the definition of these angles in relation to the horizontal base line
For statistical analysis, the mean values, standard deviations, and 95% confidence intervals were calculated individually for all measured angles for both preoperative mTFA and lower extremity CT scans. A Kolmogorov–Smirnov normality test was conducted for continuous variables to evaluate the distribution of the data composition. To determine the statistical significance of the relationship between the coronal alignment and the rotational profile of the lower extremity, a Spearman correlation analysis was used. One-way analysis of variance was conducted to determine the differences among the three groups. Interobserver and intraobserver reliabilities of the methods used to measure the radiographic parameters were assessed using intraclass correlation coefficients (ICCs). The two observers (RU, JHY) repeated the measurements twice with a 2-week interval after the initial assessment to minimize the learning effects. Sample size was calculated for a desired power of 80% and an α value of 0.05, and an estimated sample size of 143 patients was required. All statistical analyses were conducted using PASW statistics software package, version 24.0 (SPSS, Inc., Chicago, IL, USA). All statistical tests were performed with a significance level of 0.05.
Results
The relative values of the femoral neck axis (A); the distal femoral axis, comprising the anterior trochlear line (B1), clinical TEA (B2), and posterior condylar line (B3); the axis of the proximal tibial condyles (C); and the bimalleolar axis (D), according to the mechanical varus deformity of the lower extremity, are shown in Table 2. There was a tendency for increased external rotation of the knee joint parameters (B1, B2, B3, C) in relation to the hip (A) and ankle joints (D) as varus deformity of the lower extremity increased. The difference was more evident in patients with a moderate-severe deformity than it was for a mild-moderate deformity. Statistical significance was found for the A–B3 (p = 0.045), A–C (p = 0.032), D–B2 (p = 0.049), and D–C (p = 0.041) values. The correlation coefficient values between the mechanical tibiofemoral angle and each relative value are presented in Table 3. The relative external rotational deformity of the knee joint in relation to the hip joint showed a positive value with good correlation (A–B1, A–B2, A–B3, A–C). Statistical significance was found in the A–B2 (p = 0.032) and A–C (p = 0.023) values. In addition, the relative external rotational deformity of the knee joint in relation to the ankle joint also showed a positive value with good correlation (D–B1, D–B2, D–B3, D–C). Statistical significance was found for D–B2 (p = 0.049), D–B3 (p = 0.038), and D–C (p = 0.021) values. All ICC values of the intraobserver and interobserver reliabilities were excellent (> 0.8; Table 4).
Discussion
The most important findings of the present study were that varus deformity of knee joint OA was associated with significant rotational deformity. The distal femur tended to rotate externally in relation to the hip joint as the degree of varus deformity increased. Likewise, the proximal tibia tended to rotate externally in relation to the ankle joint as the degree of varus deformity increased. The amount of rotational deformity was more evident between moderate and severe deformities than it was between mild and moderate deformities of the lower extremity (Table 2). The relative external rotational deformity of the knee joint from either the hip and/or the ankle joint had a positive correlation with varus deformity of the lower extremity.
Regarding the surgical aspect of TKA, the anatomic landmarks of the distal femur (femoral epicondyles) and the proximal tibia (tibial tuberosity) are used intraoperatively to determine the position of the femoral and tibial components of TKA [32]. An important clinical implication is that the landmarks of each bone are the intrinsic cause of rotational mismatch following TKA. In TKA, tibial torsion indicates angular change from the proximal tibia and the distal tibia, while the knee joint characterizes the rotation of the tibia from the femoral bone. Both these factors can affect the rotational alignment of the tibial component [19]. While the femoral TEA is considered the functional flexion–extension axis of the knee joint [7], it is also widely accepted as the reference axis of the femoral component. Therefore, for the best TKA performance, the tibia’s rotational reference axis should correspond to the femoral TEA. However, tibial torsion in OA frequently occurs in the proximal tibia [37], and any relative variation in knee rotation changes with varus deformity [9]. The problem is that this risk proportionally increases as varus deformity increases, as was also demonstrated in this study. Therefore, surgeons who perform TKA should be aware of these considerations and must check for rotational mismatch between the components.
Rotational mismatch can be minimized by aligning the tibial component according to the femoral component rotation. The prosthetic design may play an important role in this aspect. There are also more concerns of rotational malalignment in constrained than in unconstrained prosthesis designs. A conforming and/or mobile tibial bearing surface may be advantageous because of self-aligning characteristics and could compensate for any femoro-tibial rotational mismatch [20, 21]. Furthermore, some of the tibial component designs have too asymmetric, a base plate geometry to provide more tibial plateau coverage. Maximal tibial bone coverage with proper rotational alignment of the tibial component may be competing concerns. However, proper rotational positioning of the tibial component has been shown to be a more important factor for long-term TKA function [16]. Until now, it has been difficult to draw conclusions because only a few clinical studies have assessed the relationship between rotational alignment and complications such as patellar maltracking, polyethylene wear, and revision for different component designs. Future studies should focus on this aspect.
No consensus on the relationship between the coronal alignment and the degree of femoral anteversion is currently available. Puthumanapully et al. [29] observed a reduced femoral anteversion of the lower extremity in participants with varus knee OA than in the controls who had normal alignment. In their study, a reduced femoral anteversion was detected in varus knees (9.4 ± 5°) compared with the normal controls (15.7 ± 5°). The authors measured the degree of femoral anteversion using the posterior condylar axis. In another study, Takai et al. [33] assessed the femorotibial angle using CT to determine the torsional alignment of the lower limb in OA. The torsion of the leg was measured as the inclination between the dorsal tangent to the femoral condyles and the line between the malleoli. Reikeras and Hoiseth [31] used the same method to assess the torsion of the leg in a normal adult population. Yagi et al. [37] also measured knee joint rotation angles in patients with medial, unicompartmental OA and compared them with a control group of healthy individuals. They reported that there was no significant difference between the two groups and that the range of the measured angle in the healthy individuals ranged from 9° of internal rotation to 26° of external rotation. Liodaski et al. [22] used the femoral neck-malleolar angle to measure lower-limb torsional deformities. In their study, the average knee joint rotation angle was 2.4 ± 6.4°, while the mean neck-malleolar angle was 13.2 ± 10.2°. Most of the aforementioned studies have major drawbacks in interpreting the rotational alignment of the lower extremity. The CT analysis should include the hip (femoral neck axis) and ankle (bimalleolar axis) joints together with the knee joint. A few studies only included the knee joint CT to analyze the rotational alignment of the lower extremity. Furthermore, the measured angles should be assessed as the relative angle rather than the absolute values. For example, the rotational range of the knee joint should be expressed as the relative angle from either the hip and/or the ankle joint.
The results of this study may also provide some useful information to help determine the pathogenesis of OA of the knee. It has been hypothesized that cartilage degeneration begins in the anteromedial aspect of the proximal tibia and then progresses posteromedially [36]. The tendency for the tibia to rotate externally in relation to the ankle joint may partly support this hypothesis. The exact pathomechanism of the underlying rotational deformity has not been identified in the previous literature, although impingement of the anterior cruciate ligament (ACL) and the subsequent insufficiency may be important. Future additional studies are needed to establish the role of the ACL in the development of OA in the knee joint and the rotational deformity.
This study had several limitations. First, it included only Asian patients with a female predominance. Therefore, a possible racial disparity in anatomic torsional deformity may have been present [5]. For drawing a definitive conclusion, large populations from other regional areas should be included. Second, this study assessed the rotational profile of the lower extremity using CT, which is a static method rather than a dynamic modality. Soft tissue conditions that can affect the dynamic alignment of the lower extremity (e.g., gait pattern) were therefore not reflected in this study. Third, standing AP radiography of the lower extremities was correlated with the rotational axes of CT studies, which are scanned with patients in a supine position. The deformities and rotational aspects may differ with weight-bearing conditions. Lastly, this study lacked clinical results. A clinical analysis of different prostheses selected according to the specific types of deformities should be further analyzed to determine the clinical meaning of this study’s findings.
This study investigated the relationship between lower extremity varus deformity and rotational deformity of knee joints with OA. Since the knee joint tends to rotate externally with an increased severity of genu varum deformity, the conventional technique of radiographic preoperative TKA planning may cause significant error. Advanced technology such as the navigation systems or the robotic-assisted TKA surgery should be considered.
Conclusion
The distal femur and proximal tibia (knee joint) tended to rotate externally in relation to the hip and ankle joints, respectively, as the degree of varus deformity increased. This finding is important in regard to preoperative planning and intraoperative surgical decision-making to determine the appropriate specific prosthetic alignment as well as the rotational alignment in TKA.
References
Aglietti P, Sensi L, Cuomo P, Ciardullo A (2008) Rotational position of femoral and tibial components in TKA using the femoral transepicondylar axis. Clin Orthop Relat Res 466:2751–2755
Buck FM, Guggenberger R, Koch PP, Pfirrmann CW (2012) Femoral and tibial torsion measurements with 3D models based on low-dose biplanar radiographs in comparison with standard CT measurements. AJR Am J Roentgenol 199:607–612
Chang CB, Jeong JH, Chang MJ, Yoon C, Song MK, Kang SB (2018) Concomitant ankle osteoarthritis is related to increased ankle pain and a worse clinical outcome following total knee arthroplasty. J Bone Jt Surg Am 100:735–741
Chang MJ, Jeong HJ, Kang SB, Chang CB, Yoon C, Shin JY (2018) Relationship between coronal alignment and rotational profile of lower extremity in patients with knee osteoarthritis. J Arthroplasty 33:3773–3777
Cho HJ, Chang CB, Yoo JH, Kim SJ, Kim TK (2010) Gender differences in the correlation between symptom and radiographic severity in patients with knee osteoarthritis. Clin Orthop Relat Res 468:1749–1758
Cho Y, Ko Y, Lee W (2015) Relationships among foot position, lower limb alignment, and knee adduction moment in patients with degenerative knee osteoarthritis. J Phys Ther Sci 27:265–268
Churchill DL, Incavo SJ, Johnson CC, Beynnon BD (1998) The transepicondylar axis approximates the optimal flexion axis of the knee. Clin Orthop Relat Res 356:111–118
Conti MS, Kleeblad LJ, Jones CW, Pearle AD, Sculco PK (2019) Distal femoral rotation is not associated with preoperative proximal tibial varus angle in patients with isolated medial compartment osteoarthritis. J Arthroplasty 34:281–285
Eckhoff DG, Johnston RJ, Stamm ER, Kilcoyne RF, Wiedel JD (1994) Version of the osteoarthritic knee. J Arthroplasty 9:73–79
Fujii T, Sato T, Ariumi A, Omori G, Koga Y, Endo N (2020) A comparative study of weight-bearing and non-weight-bearing 3-dimensional lower extremity alignment in knee osteoarthritis. J Orthop Sci. https://doi.org/10.1016/j.jos.2019.11.012
Guggenberger R, Pfirrmann CW, Koch PP, Buck FM (2014) Assessment of lower limb length and alignment by biplanar linear radiography: comparison with supine CT and upright full-length radiography. AJR Am J Roentgenol 202:161–167
Hauschild O, Muenzberg M, Knothe D, Konstantinidis L, Helwig P, Sudkamp NP, Thielemann FW (2013) Rotational limb alignment changes following total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 21:2346–2354
Heesterbeek PJ, Jacobs WC, Wymenga AB (2009) Effects of the balanced gap technique on femoral component rotation in TKA. Clin Orthop Relat Res 467:1015–1022
Hess S, Moser LB, Amsler F, Behrend H, Hirschmann MT (2019) Highly variable coronal tibial and femoral alignment in osteoarthritic knees: a systematic review. Knee Surg Sports Traumatol Arthrosc 27:1368–1377
Hudson D (2016) The rotational profile: a study of lower limb axial torsion, hip rotation, and the foot progression angle in healthy adults. Gait Posture 49:426–430
Incavo SJ, Coughlin KM, Pappas C, Beynnon BD (2003) Anatomic rotational relationships of the proximal tibia, distal femur, and patella: implications for rotational alignment in total knee arthroplasty. J Arthroplasty 18:643–648
Incavo SJ, Wild JJ, Coughlin KM, Beynnon BD (2007) Early revision for component malrotation in total knee arthroplasty. Clin Orthop Relat Res 458:131–136
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16:494–502
Khan MS, Seon JK, Song EK (2012) Rotational profile of lower limb and axis for tibial component alignment in varus osteoarthritic knees. J Arthroplasty 27:797–802
Kim TW, Park SH, Suh JT (2012) Comparison of mobile-bearing and fixed-bearing designs in high flexion total knee arthroplasty: using a navigation system. Knee Surg Relat Res 24:25–33
Kwak JY, Jeong JH, Lee SH, Jung HJ, Jung YB (2012) Comparison of the clinical outcomes after total knee arthroplasty with the LCS rotating platform mobile bearing knee system and the PFC Sigma RP-F mobile bearing knee system. Clin Orthop Surg 4:256–262
Liodakis E, Aljuneidi W, Krettek C, Ettinger M, Kenawey M (2011) The neck-malleolar angle: an alternative method for measuring total lower limb torsion that considers the knee joint rotation angle. Skeletal Radiol 40:617–621
Liodakis E, Doxastaki I, Chu K, Krettek C, Gaulke R, Citak M, Kenawey M (2012) Reliability of the assessment of lower limb torsion using computed tomography: analysis of five different techniques. Skeletal Radiol 41:305–311
Matsui Y, Kadoya Y, Uehara K, Kobayashi A, Takaoka K (2005) Rotational deformity in varus osteoarthritis of the knee: analysis with computed tomography. Clin Orthop Relat Res 433:147–151
Morizane K, Takahashi T, Konishi F, Yamamoto H (2011) The anterior trochlear line as a reference for femoral component positioning in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 19:2009–2015
Moussa M (1994) Rotational malalignment and femoral torsion in osteoarthritic knees with patellofemoral joint involvement. A CT scan study. Clin Orthop Relat Res 304:176–183
Nicoll D, Rowley DI (2010) Internal rotational error of the tibial component is a major cause of pain after total knee replacement. J Bone Jt Surg Br 92:1238–1244
Panni AS, Ascione F, Rossini M, Braile A, Corona K, Vasso M, Hirschmann MT (2018) Tibial internal rotation negatively affects clinical outcomes in total knee arthroplasty: a systematic review. Knee Surg Sports Traumatol Arthrosc 26:1636–1644
Puthumanapully PK, Harris SJ, Leong A, Cobb JP, Amis AA, Jeffers J (2014) A morphometric study of normal and varus knees. Knee Surg Sports Traumatol Arthrosc 22:2891–2899
Radler C, Kranzl A, Manner HM, Hoglinger M, Ganger R, Grill F (2010) Torsional profile versus gait analysis: consistency between the anatomic torsion and the resulting gait pattern in patients with rotational malalignment of the lower extremity. Gait Posture 32:405–410
Reikeras O, Hoiseth A (1989) Torsion of the leg determined by computed tomography. Acta Orthop Scand 60:330–333
Song SJ, Park CH, Bae DK (2019) What to know for selecting cruciate-retaining or posterior-stabilized total knee arthroplasty. Clin Orthop Surg 11:142–150
Takai S, Sakakida K, Yamashita F, Suzu F, Izuta F (1985) Rotational alignment of the lower limb in osteoarthritis of the knee. Int Orthop 9:209–215
Waidelich HA, Strecker W, Schneider E (1992) Computed tomographic torsion-angle and length measurement of the lower extremity. The methods, normal values and radiation load. Rofo 157:245–251
Weiner DS, Cook AJ, Hoyt WA Jr, Oravec CE (1978) Computed tomography in the measurement of femoral anteversion. Orthopedics 1:299–306
White SH, Ludkowski PF, Goodfellow JW (1991) Anteromedial osteoarthritis of the knee. J Bone Joint Surg Br 73:582–586
Yagi T, Sasaki T (1986) Tibial torsion in patients with medial-type osteoarthritic knee. Clin Orthop Relat Res 213:177–182
Yoon JR, Yang JH (2018) Satisfactory short-term results of navigation-assisted gap-balancing total knee arthroplasty using ultracongruent insert. J Arthroplasty 33:723–728
Yoshioka Y, Siu D, Cooke TD (1987) The anatomy and functional axes of the femur. J Bone Jt Surg Am 69:873–880
Acknowledgements
This work was supported by the research fund of Hanyang University (HY-2019). The authors would like to thank Ms. Min-Jung Lee for statistical analysis.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Ethical approval
This study was approved by the institutional review board of Veterans Health Service Medical Center (IRB No. VHS-2020-0601).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yoon, JR., Lee, J.K., Ryu, J. et al. Increased external rotation of the osteoarthritic knee joint according to the genu varum deformity. Knee Surg Sports Traumatol Arthrosc 29, 1098–1105 (2021). https://doi.org/10.1007/s00167-020-06100-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-06100-7