Abstract
Purpose
The primary objective of this study was to quantify the variations of the medial posterior tibial slope (MPTS) and the lateral posterior tibial slope (LPTS), as well as of the medial proximal tibial angle (MPTA), and to determine the fraction of patients for which standard techniques including different alignment techniques would result in alteration of the patient’s individual posterior tibial slope (PTS) and MPTA. Furthermore, it was of interest if a positive correlation between PTS and MPTA or between medial and lateral slope exists.
Methods
A retrospective study was performed on CT-scans of 234 consecutively selected European patients undergoing individual total knee replacement. All measurements were done on three-dimensional CAD models, which were generated on the basis of individual CT-scans, including the hip, knee, and ankle center. Measurements included the medial and lateral PTS and the MPTA. PTS was measured as the angle between the patient’s articular surface and a plane perpendicular to the mechanical axis of the tibia in the sagittal plane. MPTA was defined as the angle between the tibial mechanical axis and the proximal articular surface of the tibia in the coronal plane.
Results
Analysis revealed a wide variation of the MPTS, LPTS, and MPTA among the patients. MPTS and LPTS varied significantly both interindividually and intraindividually. The range of PTS was up to 20° for MPTS (from − 4.3° to 16.8°) and for LPTS (from − 2.9 to 17.2°). The mean intraindividual difference between MPTS and LPTS in the same knee was 2.6° (SD 2.0) with a maximum of 9.5°. MPTA ranged from 79.8 to 92.1° with a mean of 86.6° (SD ± 2.4). Statistical analysis revealed a weak positive correlation between MPTA and MPTS.
Conclusion
The study demonstrates a huge interindividual variability in PTS and MPTA as well as significant intraindividual differences in MPTS and LPTS. Therefore, the question arises, whether the use of standard techniques, including fixed PTSs and MPTAs, is sufficient to address every single patient’s individual anatomy.
Level of evidence
III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The proximal tibia shows a complex surface anatomy comprising asymmetric medial and lateral tibial plateaus, as well as variations in the posterior tibial slope (PTS) and the medial proximal tibial angle (MPTA). In total knee arthroplasty (TKA), a number of 20–30% of patients are not satisfied with their surgical intervention [2, 11, 14]. A potential reason could be disrespect of the patient’s individual anatomy. In a first step, this approach requires a profound understanding of the tibial geometry's complex anatomy in its three different planes, as well as of its interindividual and intraindividual variations. Medial and lateral PTS (MPTS and LPTS) may differ in an individual knee [12]. During preoperative surgical planning, patients usually only receive lateral X-rays, which often do not allow to determine the MPTS and LPTS separately and, therefore, do not provide sufficient information required for restoring the patient’s individual PTS, which is of particular importance in unicondylar knee arthroplasty. Furthermore, using standard techniques in cruciate retaining TKA, the overall PTS is conventionally decided varying between 3° and 7° and being often more dependent of the implant design or surgeon’s philosophy than the patient’s anatomy. In posterior stabilized TKA, the PTS is mostly cut in 0°–3° due to cam/spine mechanism. The consequences of changing PTS with knee implants, however, are complex and neither well investigated nor fully understood.
In addition to the variations of the MPTS and LPTS in the sagittal plane, also the variations of the MPTA in the frontal plane need to be considered. Various alignment techniques have been introduced including the mechanical alignment with an MPTA of 0°, the anatomical alignment with an MPTA of 3° varus, and the kinematic alignment, in which the MPTA is nearly not altered. Proponents of the last-mentioned alignment technique argue that by not altering the MPTA, the anatomy of the patient is more reconstructed, which might result in a better clinical outcome. However, the anatomy may show complex and severe axis deformities of an intra- or extraarticular origin [16]. Hess et al. in a systematic review of 15 studies reported a high coronal variability not being sufficiently addressed by current TKA alignment philosophies [6]. In a consequence, Hirschmann et al. introduced a new classification system, based on limb phenotypes, with the aim of a better understanding of the individual coronal knee alignment [7].
However, coronal alignment and not only the MPTA but both the MPTS and LPTS are essential parts of the tibial geometry in its three-dimensional nature, too [15]. All alignment techniques focus on MPTA while placing lesser focus on the PTS and, in particular, on the possible differences between MPTS and LPTS.
The primary objective of this study was to quantify the variations of the MPTS and LPTS, as well as of the MPTA and to determine the fraction of patients for which standard techniques including different alignment techniques would result in an alteration of the patient’s individual PTS and MPTA. Furthermore, it was of interest if a positive correlation (r > 0, p < 0.05) between a PTS and an MPTA or between medial and lateral slope does exist.
The hypothesis of the present study was that a high variation in MPTS, LPTS, as well as MPTA exists, and that standard techniques including different alignment techniques may not consider these variations sufficiently.
Methods
A retrospective study was performed on CT-scans of 234 patients scheduled for an individual knee replacement from 2014 until 2017. Patients were selected consecutively. Information about the study cohort is displayed in Table 1.
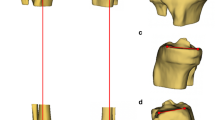
All measurements were done on three-dimensional CAD models, which were generated on the basis of individual CT-scans, including the hip, knee, and ankle center. Measurements included the MPTS, LPTS, and the MPTA. For measuring the MPTS and LPTS, first, the mechanical axis of the tibia was established using the ankle center. The patient’s individual slope was defined as the line tangent to the most prominent aspects of the anterior and posterior cortices of the respective compartment. The angle between the plane perpendicular to the mechanical axis of the tibia and the patient’s individual slope was measured and defined as the patient’s medial or lateral slope angle. MPTA was defined as the angle between the tibial mechanical axis and the proximal articular surface of the tibia in the coronal plane. To investigate if there are significant differences of MPTS, LPTS, and MPTA in gender or in alignment, variations have been evaluated respectively. To quantify the fraction of patients for whom the use of a standard technique would lead to an altered MPTS, LPTS, or MPTA > 2°, the patients’ data were compared to those of standard techniques. For the PTS, a standard value of 5° was used and the respective fraction of patients having an MPTS or LPTS < 3° or > 7° was determined. Concerning MPTA, a value of 90° was used for mechanical alignment, while a value of 87° was used for anatomical alignment and the fraction of patients was determined who had an MPTA < 88° or > 92°, and < 85° or 89°, respectively.
Statistical analysis
Statistical analysis was performed with Prism8 (Graph Pad Software).
Shapiro–Wilk normality test showed data of MPTS, LPTA, and MPTA to be distributed normally. Unpaired Student’s two-tailed t test was performed for differences in MPTS and LTPS with a statistical significance set at a p value of < 0.05. The comparison of MPTS and LPTS of different MPTA subgroups was assessed using a one-way ANOVA with Tukey’s adjustment for multiple comparisons. To identify any correlation between PTS and MPTA the Pearson’s correlation was performed and the correlation coefficient (r) was calculated. Alpha was set at 0.05. To assess inter-reader and intra-reader agreement, the intraclass correlation coefficient (ICC) was used. The intra-rater reliability was 0.96 for MPTS, 0.97 for LPTS, and 0.94 for MPTA. The inter-rater reliability was 0.88 for MPTS, 0.90 for LPTS, and 0.86 for MPTA. For sample size calculation, a two-sided sample size was assumed with an α (Type I error rate) of 5% and statistical power of 80%. A sample size of 230 would allow for the detection of significant differences between MPTS and LPTS of 2.9 standard deviations.
Results
Measurements of MPTS, LPTS, and MPTA are displayed in Table 2. Positive values correspond to a posterior tibial slope, whereas negative values correspond to an anterior tibial slope. The mean difference between MPTS and LPTS intraindividually was 2.6° (SD ± 2.0) with a maximum of 9.5°. Differences between the MPTS and LPTS were significant intraindividually (p = 0.02).
MPTS and LTPS did not differ significantly by gender, whereas MPTA was significantly different for females and males with females having a greater MPTA than men (p = 0.04) (Table 3).
MPTS and MPTA was significantly different between varus and valgus alignment with a p value of 0.02 and a p value of 0.0008, respectively. LPTS did not differ significantly between varus and valgus aligned knees (Table 4).
Analysis showed that 65% (152/234) of patients had an MPTS, and 53% (124/234) of patients had a LTPS < 3° or > 7°, which would result in an alteration of the patient’s PTS by more than 2° if a standard PTS of 5° was used (Figs. 1 and 2).
Analysis also showed that 83% (195/234) of patients had an MPTA > 92° or < 88°, which would result in a postoperative alteration of the patient’s MPTA > 2°, if a mechanical alignment technique with an MPTA of 90° were used (Fig. 3a). Using anatomical alignment with an MPTA set at 87° varus, it would result in a postoperative alteration of the MPTA > 2° in 41% (97/234) of patients having a MPTA > 89° or < 85° (Fig. 3b).
a Fraction of patients with different degrees of MPTA vs an MPTA of 0° in mechanical alignment. Analysis showed that 83% (195/234) of patients had an MPTA > 92° or < 88°, which would result in a postoperative change of the MPTA > 2° compared to the patient’s MPTA (highlighted red). b Fraction of patients with different degrees of MPTA vs. an MPTA of 3° varus in anatomical alignment. Analysis showed that 41% (97/234) of patients had an MPTA > 89° or < 85°, which would result in a postoperative change of the MPTA > 2° compared to the patient’s MPTA (highlighted red)
Analysis showed a weak but significant correlation between MPTS and MPTA (p = 0.03, r = 0.14) (Fig. 4). However, clustering the data into different MPTA subgroups (MPTA > 90°, MPTA 89–85° and MPTA < 85°) showed no significant differences in MPTS and LPTS (Table 5). In Addition, analysis showed a significant correlation between MPTS and LPTS (p ≤ 0.0001, r = 0.59) (Fig. 5).
Discussion
The most important finding of the present study is that the geometry of the tibial plateau varies enormously interindividually with a range over 20° for MPTS and LPTS and a range over 12° for MPTA as well as intraindividually with differences between the MPTS and LPTS of up to 9.5°, confirming the authors’ hypothesis. These variations may not be fully addressed by standard techniques including different alignment techniques and may, therefore, lead to alterations of the patient’s anatomy in knee arthroplasty.
The consequences of changing PTS with knee implants are multiple and neither well investigated nor fully understood. This is of utmost importance in particular to bi-cruciate retaining arthroplasties as UKA, bi-unicondylar or bi-cruciate retaining TKA, since the preservation of the cruciate ligaments requires a more precise restoration of the patient’s PTS [12]. If another UKA is added to the contralateral compartment due to disease progression, the surgeon can not only rely on the PTS of the already implanted component but has also to be aware of possible differences between the MPTS and LPTS. Furthermore, there is a huge debate on overcoming the dogma of the strict 90° mechanical alignment in knee arthroplasty to a more native situation as well.
The data obtained in the present study revealed a high variability of PTS and MPTA, which might result in an alteration of patient’s anatomy, if standard techniques are used. The setting of the PTS is usually dependent either on the surgeon, for example, by always aiming for 5° of PTS or dependent on the implant system and its instrumentation with additional inaccuracy of external cutting alignment. However, because of the variability of the PTS, such a setting might lead to alterations of the patient’s individual PTS in a huge amount of cases. These alterations are further caused by and potentially further increased by the fact that both MPTS and LPTS may differ in one single knee, too. Furthermore, if a standard instrument allows to define the PTS gradually and, therefore, allows a setting of PTS which is the same as the patient’s MPTS, alterations in LPTS would result.
Nunley et al. [12] also reported a high variability of the PTS with a range of 26.4° in the medial and 22.5° in the lateral compartment. They also reported that 44.5% of the medial and 60.7% of the lateral compartment had a PTS > 7° and thereby exceeding most standard instruments. An alteration of the patient’s individual PTS may result in clinical consequences impacting flexion ability [1, 17], quadriceps force required for knee motion [13], and anterior sliding of the tibial component [13, 18] or tension of the cruciate ligaments resulting in sagittal plane stability.
Concerning the MPTA, different alignment techniques have been introduced in the past including mechanical, anatomical and various types of kinematic alignment. The present study suggests, due to the verified high variability of the MPTA, that using mechanical or anatomical alignment may lead to alterations of the patient’s MPTA. Alterations of the angle and level of the patient’s joint line can lead to abnormal contact kinematics and the need for soft-tissue releases due to tightening or slackening of the collateral, posterior cruciate or retinacular ligaments, which might be the reason for the growing interest in kinematic alignment [3, 10, 19]. Proponents of the kinematic alignment argue that said technique results in a better reconstruction of the patient’s anatomy. Innocenti et al. reported that a neutral mechanical or a 3° of varus alignment has similar biomechanical effects, whereas a 6° varus alignment or changes in valgus alignment are associated with detrimental effects in medial UKA [9]. Hirschmann et al., who investigated coronal lower limb alignment in young non-osteoarthritic patients, reported on a high variability in coronal alignment and, therefore, claim for a more individualized approach to TKA alignment. However, not only the coronal alignment, but also the sagittal alignment in terms of PTS and, in particular in differences in MPTS and LPTS, need to be considered [8].
Another important finding of the present study was the significant difference between MPTS and LPTS. This fact should be considered, especially in UKA, when osteoarthritis progresses to the opposite femorotibial compartment and an additional UKA is added, as well as in bi-cruciate-retaining TKA, as the preservation of the cruciate ligaments requires a more precise restoration of the patient’s individual PTS [12]. Hashemi et al. [5] also reported significant intraindividual differences between MPTS and LTPS, whereas Haddad et al. [4] found no significant difference between MPTS and LTPS. However, their accuracy of measurements may be somewhat limited as their investigations were based on magnetic resonance imaging, which does not display the whole length of the tibia and, therefore, fails to show the true mechanical axis. Furthermore, their investigations were performed on healthy knees, whereas the present study’s results provide insight in the geometry of the tibial plateau in knees affected by osteoarthritis, which is of great importance, since osteoarthritis affects the tibial geometry and may lead to deformities in the coronal as well as in the sagittal plane. The present study also showed that knees in valgus alignment had a significant greater MPTS compared to knees in varus alignment (p = 0.02).
The present study further showed a significant positive correlation between MPTS and MPTA. However, the correlation is very weak, so that it is likely that MPTA and MPTS are stronger influenced by other factors that by each other. Furthermore, clustering the data into different MPTA subgroups (MPTA > 90°, MPTA 89–85° and MPTA < 85°) showed no significant differences in MPTS as well as LPTS (Table 5).
The present study showed several limitations that need to be considered. First and of great importance is the virtual nature of measurements, which cannot be directly transferred to the intraoperative situation. In addition, due to the present study’s nature as an imaging study, any conclusions concerning the clinical consequences are necessarily of a presumptive nature. Furthermore, all patients included in this study were all scheduled for a customized knee arthroplasty; however, to the authors’ opinion, this is no relevant limitation, because the selection criteria for receiving either UKA or TKA were the same irrespective of using a customized or an off-the-shelf-implant. The only difference was that in patients with a severe valgus or varus deformity (> 15°) or severe ligamentous instability, a customized TKA was contraindicated. Additionally, the cohort displays a representative European cohort receiving medial or lateral UKA as well as TKA and the consecutive selection should further limit the risk of selection bias. A further limitation of the present study is that CT does not display cartilage. However, the shortcomings resulting from that issue are similar to standard TKA instrumentation, which also does not allow for cartilage estimation and which are in common use in clinical practice. Even so, this is an important issue that should be considered by future studies and perhaps future instrumentation as in calipered arthroplasty techniques. Furthermore, CT does not display weight-bearing conditions. Also, the sample size is too small for generalization and does not regard possible ethnical differences, but displays a representative European cohort receiving medial or lateral UKA as well TKA and is, therefore, the highest sample size published so far, particularly considering the different arthroplasty entities.
Conclusion
The study demonstrates a huge interindividual variability in PTS and MPTA as well as significant intraindividual differences in MPTS and LPTS. Therefore, the question arises, whether the use of standard techniques, including fixed PTSs and MPTAs, is sufficient to address every single patient’s individual anatomy.
Abbreviations
- PTS:
-
Posterior tibial slope
- MPTS:
-
Medial posterior tibial slope
- LPTS:
-
Lateral posterior tibial slope
- MPTA:
-
Medial proximal tibial angle
- TKA:
-
Total knee arthroplasty
- UKA:
-
Unicondylar knee arthroplasty
References
Bellemans J, Robijns F, Duerinckx J, Banks S, Vandenneucker H (2005) The influence of tibial slope on maximal flexion after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 13:193–196
Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KDJ (2010) Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res 468:57–63
Dossett HG, Estrada NA, Swartz GJ, LeFevre GW, Kwasman BG (2014) A randomised controlled trial of kinematically and mechanically aligned total knee replacements: two-year clinical results. Bone Jt J 96:907–913
Haddad B, Konan S, Mannan K, Scott G (2012) Evaluation of the posterior tibial slope on MR images in different population groups using the tibial proximal anatomical axis. Acta Orthop Belg 78:757–763
Hashemi J, Chandrashekar N, Gill B, Beynnon BD, Slauterbeck JR, Schutt RC, Mansouri H, Dabezies E (2008) The geometry of the tibial plateau and its influence on the biomechanics of the tibiofemoral joint. J Bone Jt Surg Am 90:2724–2734
Hess S, Moser LB, Amsler F, Behrend H, Hirschmann MT (2019) Highly variable coronal tibial and femoral alignment in osteoarthritic knees: a systematic review. Knee Surg Sports Traumatol Arthrosc 27:1368–1377
Hirschmann MT, Hess S, Behrend H, Amsler F, Leclercq V, Moser LB (2019) Phenotyping of hip-knee-ankle angle in young non-osteoarthritic knees provides better understanding of native alignment variability. Knee Surg Sports Traumatol Arthrosc 27:1378–1384
Hirschmann MT, Moser LB, Amsler F, Behrend H, Leclerq V, Hess S (2019) Functional knee phenotypes: a novel classification for phenotyping the coronal lower limb alignment based on the native alignment in young non-osteoarthritic patients. Knee Surg Sports Traumatol Arthrosc 27:1394–1402
Innocenti B, Pianigiani S, Ramundo G, Thienpont E (2016) Biomechanical effects of different varus and valgus alignments in medial unicompartmental knee arthroplasty. J Arthroplasty 31:2685–2691
Matsumoto T, Takayama K, Ishida K, Hayashi S, Hashimoto S, Kuroda R (2017) Radiological and clinical comparison of kinematically versus mechanically aligned total knee arthroplasty. Bone Jt J 99:640–646
Noble PC, Conditt MA, Cook KF, Mathis KB (2006) The John Insall Award: patient expectations affect satisfaction with total knee arthroplasty. Clin Orthop Relat Res 452:35–43
Nunley RM, Nam D, Johnson SR, Barnes CL (2014) Extreme variability in posterior slope of the proximal tibia: measurements on 2395 CT scans of patients undergoing UKA? J Arthroplasty 29:1677–1680
Okamoto S, Mizu-uchi H, Okazaki K, Hamai S, Nakahara H, Iwamoto Y (2015) Effect of tibial posterior slope on knee kinematics, quadriceps force, and patellofemoral contact force after posterior-stabilized total knee arthroplasty. J Arthroplasty 30:1439–1443
Parvizi J, Nunley RM, Berend KR, Lombardi AV, Ruh EL, Clohisy JC, Hamilton WG, Della Valle CJ, Barrack RL (2014) High level of residual symptoms in young patients after total knee arthroplasty. Clin Orthop Relat Res 472:133–137
Thienpont E, Bellemans J, Victor J, Becker R (2013) Alignment in total knee arthroplasty, still more questions than answers. Knee Surg Sports Traumatol Arthrosc 21:2191–2193
Thienpont E, Parvizi J (2016) A new classification for the varus knee. J Arthroplasty 31:2156–2160
Walker PS, Garg A (1991) Range of motion in total knee arthroplasty. A computer analysis. Clin Orthop Relat Res 227–235
Wasielewski RC, Galante JO, Leighty RM, Natarajan RN, Rosenberg AG (1994) Wear patterns on retrieved polyethylene tibial inserts and their relationship to technical considerations during total knee arthroplasty. Clin Orthop Relat Res 31–43
Yoon J-R, Han S-B, Jee M-K, Shin Y-S (2017) Comparison of kinematic and mechanical alignment techniques in primary total knee arthroplasty. Medicine (Baltimore) 96
Funding
This study received no funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
FK receives royalties of Königsee and honoraria of ConforMIS, all outside the submitted work. DJ has received compensations covering the living costs in Boston from ConforMIS. JB receives honoraria from DePuy, Smith&Nephew and ConforMIS, all outside the submitted work. ET is a speaker bureau for ComaTec, KCI, Limo, Medacta, and Zimmer Biomet, receives royalties of Zimmer Biomet and is EKS President 2019, all outside the submitted work. RB has no potential conflict of interest. MM has no potential conflict of interest.
Ethical approval
Since the present study is based on analysing anonymised CT data, IRB approval was not required. Any information that could identify patients was not use in the analysis. Investigators dealt with anonymised data only. All procedures performed were in accordance with the ethical standards of the institutional and/or national research committee and with Declaration of Helsinki and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Meier, M., Janssen, D., Koeck, F.X. et al. Variations in medial and lateral slope and medial proximal tibial angle. Knee Surg Sports Traumatol Arthrosc 29, 939–946 (2021). https://doi.org/10.1007/s00167-020-06052-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-06052-y