Abstract
Purpose
The purpose of this study was to describe the medial and lateral posterior tibial slope (MPTS and LPTS) on 3D-CT in a Caucasian population without osteoarthritis. It was hypothesised that standard TKA alignment techniques would not reproduce the anatomy in a high percentage of native knees.
Methods
CT scans of 301 knees [male:female = 192:109; mean age 30.1 (\(\pm\) 6.1)] were analysed retrospectively. Tibial slope was measured medially and laterally in relation to the mechanical axis of the tibia. The proportion of MPTS and LPTS was calculated, corresponding to the “standard PTS” of 3°–7°. The proportion of knees accurately reproduced with the recommended PTS of 0°–3° for PS and 5°–7° for CR TKA were evaluated.
Results
Interindividual mean values of MPTS and LPTS did not differ significantly (mean (range); MPTS: 7.2° ( – 1.0°–19.0°) vs. LPTS: 7.2° ( − 2.4°–17.8°), n.s.). The mean absolute intraindividual difference was 2.9° (0.0°–10.8°). In 40.5% the intraindividual difference between MPTS and LPTS was > 3°. When the standard slope of 3°–7° medial and lateral was considered, only 15% of the knees were covered. The tibial cut for a PS TKA or a CR TKA changes the combined PTS (MPTS + LPTS) in 99.3% and 95.3% of cases, respectively.
Conclusion
A high interindividual range of MPTS and LPTS as well as considerable intraindividual differences were shown. When implementing the recommended slope values for PS and CR prostheses, changes in native slope must be accepted. Further research is needed to evaluate the impact of altering a patient’s native slope on the clinical outcome.
Level of evidence
IV.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The medial and lateral posterior tibial slopes (MPTS and LPTS) are important features of the complex three-dimensional (3D) anatomy of the proximal tibia [19]. Historically, MPTS and LPTS have not been considered as two different entities, mainly because the separate evaluation of MPTS and LPTS on conventional radiographs is difficult and often does not provide sufficient information for preoperative planning [22]. Over the last decade, personalized computer-assisted 3D planning for total knee arthroplasty (TKA) or tibial osteotomies has been introduced with the goal of improving accuracy and reducing outliers and thereby improving patient satisfaction [6, 12]. Instead of using a rather simplified systematic approach to TKA alignment, as implemented in current standard techniques and instruments, the reconstruction of an individual alignment has been proposed [9, 11]. This would not only include the coronal alignment, but also restore the patient`s native MPTS and LPTS. However, adjusting the surgical approach as closely as possible to the patient’s anatomy requires precise knowledge of the anatomic variability of the native knee. Although there are studies reporting on PTS measured on 3D-CT in osteoarthritic (OA) knees [18], there are limited data on MPTS and LPTS in non-OA knees in the Caucasian population [22, 24]. Accordingly, it is unknown how PTS changes over time. For OA patients, a high variability of PTS with differences in mean values of up to 5° and interindividual ranges as high as 30° have been reported [20]. Since there is a trend in orthopedics to restore the original anatomy in both joint-preserving therapy options as well as joint-replacing alternatives (e.g., kinematic alignment), it is of great importance to analyze the native anatomy in a first step. The purpose of this study was to describe inter and intraindividual differences of MPTS and LPTS on 3D-CT in a Caucasian population without OA. The first hypothesis was that a difference of more than \(\pm\) 3° between the MPTS and LPTS exists in more than 25% of knees. The second hypothesis was that the patients’ individual, native anatomy does not correspond to the standard PTS chosen in sagittal TKA alignment of 3°–7°, nor to the recommended PTS for posterior stabilized (PS) or cruciate-retaining (CR) TKA in more than 50% of knees [1, 22]. The purpose of the second hypothesis was to show in which proportion of patients and to what extent the native slope is altered when the tibial component is implanted according to the conventional standard.
Materials and methods
Approval was obtained from the local ethical committee (Ethikkommission Nordwest- und Zentralschweiz, ID 2018-00223). The hospital registry was searched for patients younger than 45 years and older than 16 years, who received a CT of the knee, according to the Imperial Knee Protocol [7]. Each leg of these patients meeting the aforementioned criteria was assessed separately for the following exclusion criteria: hip, knee or ankle prosthesis, osteotomy (e.g., varus osteotomy), any radiological signs of osteoarthritis or fractures, and reported injury of the collateral ligaments. Finally, a total of 301 non-OA knees from 160 patients were included in this study. SPECT/CT was obtained between January 2011 and March 2017. All patients received a 99mTc-hydroxymethane diphosphonate (HDP) SPECT/CT of the knee according to the Imperial Knee Protocol using a Symbia T16 (Siemens, Erlangen, Germany). CT scans consisted of 3-mm-thick low-dose slices of the femoral head and the ankle and high-resolution 0.7-mm slices of the knee [7]. Both legs from 141 patients and a single leg from 19 patients were included. SPECT/CT was conducted for the following reasons: knee pain of unknown origin (e.g. anterior knee pain without trauma) (n = 22); osteochondritis dissecans (n = 13); persistent pain after treatment of sports injury (n = 87) and idiopathic patellar pathology (n = 36). In 15 patients both knees were affected by one of the aforementioned pathologies. The limb, which was the reason for the imaging was labelled as “symptomatic” and the contralateral leg as “asymptomatic”. This left a total of 143 asymptomatic non-osteoarthritic knees and 158 symptomatic non-osteoarthritic knees.
All measurements were performed by the same trained engineer who has more than 10 years’ experience in this field. A previously validated, commercially used planning software (KneePLAN 3D, Symbios, Yverdon les Bains, Switzerland) was used. This software creates a 3D model based on the CT images obtained during the SPECT/CT. For CE marking, the accuracy of measurements including inter- and intra-observer reliability has been reported as excellent, having measurement variability within 1° [5].
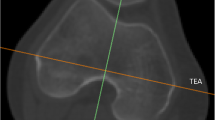
For measuring the MPTS and LPTS the mechanical axis of the tibia was established using the tibial spine and the ankle centre as reference. The individual slope was defined as the line tangential to the most prominent aspects of the anterior and posterior cortices of the respective compartment [23]. The angle between the plane perpendicular to the mechanical axis of the tibia and the individual slope was measured and defined as the MPTS or LPTS [19] (Fig. 1). Positive values correspond to a posterior tibial slope, whereas negative values to an anterior tibial slope. A difference of \(\pm\) 3° between MPTS and LPTS was considered to be physiological [18].
In conventional TKA the PTS is chosen between 3° and 7°. With varying knee implant designs, adaptions regarding PTS are required due to varying knee kinematics. In PS TKA a PTS of 0°–3° is recommended to provide tibial component stability and avoid anterior post impingement [1]. In CR designs a PTS of 5°–7° is aimed to achieve adequate range of motion (ROM) postoperatively, particularly in flexion [21].
The proportion of MPTS and LPTS corresponding to a standard PTS as well as the proportion of knees accurately reproduced by specifically recommended PTS for PS (0°–3°) and CR (5°–7°) TKA were evaluated. Clinically accepted deviations of \(\pm\) 1.5° were incorporated in the analysis.
Statistical analysis
Descriptive statistics, such as means, standard deviations and ranges are presented. The distribution of MPTS and LPTS are shown. T-tests for independent samples were used to compare sex specific influences and for paired samples to compare MPTS and LPTS. The relationship between the two angles was tested with Pearson correlations. All data were analysed by an independent statistician. The p values were two-sided and considered statistically significant if smaller than 0.05. Post hoc power analysis was conducted two-sided (p < 0.05) with the given n and a power of 80% using G*Power 3.1.9. Gender-specific differences could be found with a small to medium effect size d = 0.34. Differences between MPTS and LPTS and correlations between the angles could both be found with a small effect size d = 0.17 and rho = 0.16, respectively.
Results
Mean values, ranges, and standard deviations of MPTS and LPTS are listed in Table 1. There were 192 (63.8%) male and 109 (36.2%) female patients [mean age ± standard deviation (SD) 30.1 ± 6.7 (range 16–44 years)]. MPTS and LPTS differed less than 0.5° and not significantly between male and female knees. Therefore, the influence of sex on PTS is negligible.
Inter- and intraindividual analysis
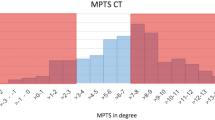
A significant positive correlation between MPTS and LPTS (r = 0.44; p < 0.001) was shown. Interindividual mean values did not differ significantly. However, high interindividual ranges of 20° were shown for MPTS as well as LPTS (Table 1). The mean absolute intraindividual difference was 2.9° (0.0°–10.8°) (Table 1). In 40.5% of knees MPTS and LPTS differed more than 3° from each other (Fig. 2), thus confirming the first hypothesis. In approximately one-third of patients either the MPTS or the LPTS corresponded to the standard PTS of 3°–7°. Considering the entire PTS (MPTS + LPTS) only 15% of knees corresponded to the standard PTS (Table 2).
There was no statistical difference in MPTS or LPTS between symptomatic and asymptomatic knees.
Hypothetical TKA (CR and PS) analysis
The tibial cut for a PS TKA changes the MPTS in 90.6%, the LPTS in 91.7% and the combined PTS (MPTS + LPTS) in 99.3% of cases (Fig. 3). The tibial cut for a CR TKA changes the MPTS in 77.4%, the LTPS in 82.4% and the combined PTS (MPTS + LPTS) in 95.3% of cases (Fig. 4). Even if clinically acceptable deviations of \(\pm\)1.5° (3.5°–8.5°) in CR TKA are considered, the native anatomy is matched in a total of only 29.6% of knees (Fig. 5), thus confirming the second hypothesis.
Discussion
The most important finding of the present study is that in more than 40% of knees there are relevant intraindividual differences between MPTS and LPTS of more than 3°; these differences are even up to 11°. The fact that the PTS is highly variable has been shown before, but differences in MPTS and LPTS might have been obscured by the analysis of only mean values which, even in this cohort, do not differ at all. This implies that in this clinical setting—even if the intraoperatively chosen slope corresponds to the native slope of one compartment—in 40% of TKAs the anatomy of the other compartment’s slope is changed more than 3° thus leading to an altered flexion and/or extension gap in the respective compartment.
The second most important finding is that 63.5% of MPTS and 65.4% of LPTS do not correspond to the standard slope of 3°–7° or the recommended PTS for PS and CR TKA. Therefore, both hypotheses have been confirmed. It might be particularly important that the intraindividual differences between MPTS and LPTS are considered, as more recent studies recommend reconstruction of the native slope. Several authors are of the opinion that anatomical reconstruction has a positive influence on the outcome after TKA [3, 13, 14, 17, 27, 30]. However, up to date, the selection of slope for TKA is still discussed controversially. With the goal of reconstructing the native anatomy the question arises which slope (MPTS/LPTS or mean) should be used as the reference for the tibial cut. General recommendations do not exist. There is, however, one study which recommends using the LPTS as a reference [15]. These data show that a tibial cut resembling the MPTS leads to a relevant bone loss of the lateral plateau of more than 10 mm in thickness (= standard tibial prosthetic component) in 24% of the evaluated knees. When using the LPTS as a reference, excessive resection occurred in only 2% of cases. However, this study analysed a very selective cohort of mainly female Japanese, varus misaligned knees with a mean MPTS of 9° and a mean LPTS of 8°. Therefore, this cohort and their results differ from ours and are probably not applicable to the broader Caucasian population. However, regarding the reference slope for the tibial cut Kuwano et al. [15] believe that the flatter slope should be chosen to avoid excessive resection and instability.
Considering different knee implants with varying PTS recommendations, changes to the patient’s native anatomy, even higher than shown by our data, have to be expected. The clinical consequences of these findings are not fully known and warrant further research. A flat slope reduces the tibiofemoral rollback and causes posterior tibiofemoral impingement [30]. The maximum force on the quadriceps and the patellofemoral contact stress decrease with increased PTS [14]. Moreover, the maximal flexion achieved postoperatively is affected by PTS. An increment of 1° in the tibial slope results in an improvement of 1.7°–2.6° in flexion [2, 17, 25], reaching a plateau effect at 6° [4]. On the other hand, an excessive slope compromises the insertion point of the posterior cruciate ligament (PCL), possibly causing sagittal and (small) coronal instability. This becomes especially important in situations where the anterior cruciate ligament (ACL) is no longer present or has been resected and the only passive restraint to an anterior tibial translation is provided by the posterior lip of the tibial insert. Higher stresses on the posterior lip of the insert lead to eventual polyethylene wear [29] and flexion instability [26].
Interestingly, compared to the results of the non-OA knees, other studies evaluating the MPTS and LPTS in OA knees using preoperative images [23] show a tendency towards a flatter MPTS in varus knees and a higher LPTS in valgus knees. In valgus knees, the natural roll-back mechanism combined with tibial internal rotation could lead to posterior bone loss in the lateral compartment leading to an increased LPTS. Vice versa, the internal rotation in varus knees could lead to anteriorly located bone loss in the more constrained medial compartment leading to a decreased MPTS. Unfortunately, longitudinal data are still missing and therefore the exact natural course and the mechanisms leading to changes of PTS in OA knees are not known.
Our findings provide insight into the diversity of anatomy and morphology of the non-OA knee joint. Using current standard techniques, PTS cuts are mainly dependent on the surgeon’s philosophy and on the implant design. So far, the patient’s individual anatomy has been considered secondary. Recently published studies showed a wide variation of knee phenotypes regarding the coronal alignment [8]. The results of the current study justify the assumption that the anatomical diversity of the knee joint is even greater and more complex when the sagittal plane is also considered. Due to the high intraindividual differences, hypothetically, the reconstruction of two different slopes by using two unicondylar knee arthroplasties or a tibial insert with two different designs of sagittal curvature might be an option to prevent PTS alterations. However, the influence of certain specific anatomic factors will have to be considered. These factors include the curvature of the distal femoral condyle in the sagittal view (different radius/radii of curvature and centre), the “soft tissue” slope (cartilage and menisci) as well as the joint line of both compartments in the frontal and sagittal plane. Until now there is no TKA system providing the option of implementing two different slopes. Our data will serve as input for future studies and represent another piece of the “puzzle” on the way to a more individualized medicine, which will certainly need further investigation.
This study has several limitations. First, the measurements are only based on Caucasian non-OA knees and the clinical consequences are of a presumptive nature and cannot be transferred directly to OA knees or other ethnicities. Second, the measurements were done on 3D-reconstructed CT images. However, a recent study analyzing MPTS and LPTS on 3D-CT images in the central weight-bearing zone of the tibial plateau presented comparable results [10]. Third, only the bony tibial slope was measured. Changes in the slope can be expected by including the tibial cartilage and menisci (“tibial soft tissue slope”). MRI analyses of the tibial soft tissue slope showed that the tibial slope is more horizontal in the lateral compartment than in the medial compartment. Due to the steeper posterior angulation medially, even greater differences between the compartments can be expected [16]. Fourth, inter and intra-reader reliability were not assessed. However, inter-reader reliability has been reported to be excellent for PTS measurement on CT scans [28], and thus, differences were assumed to be minimal.
The clinical importance of this study is that it highlights the variability of PTS and especially the intraindividual differences of the medial and lateral compartment. This might be important for the clinical work-up as well as preoperative planning and intraoperative decisions.
Conclusion
A high interindividual range of MPTS and LPTS as well as considerable intraindividual differences were shown in native knees. When implementing the recommended slope values for PS and CR prostheses, changes in native slope are to be expected.
Further research is needed to evaluate the impact on the clinical outcome of altering a patient’s native slope.
Abbreviations
- ACL:
-
Anterior cruciate ligament
- AP:
-
Anterior – posterior
- CR:
-
Cruciate retaining
- MPTS:
-
Medial posterior tibial slope
- OA:
-
Osteoarthritis
- ROM:
-
Range of motion
- PCL:
-
Posterior cruciate ligament
- PS:
-
Posterior stabilized
- PTS:
-
Posterior tibial slope
- ROM:
-
Range of motion
- LPTS:
-
Lateral posterior tibial slope
- TKA:
-
Total knee arthroplasty
- 3D:
-
Three dimensional
References
Bai B, Baez J, Testa NN, Kummer FJ (2000) Effect of posterior cut angle on tibial component loading. J Arthroplasty 15:916–920
Bellemans J, Robijns F, Duerinckx J, Banks S, Vandenneucker H (2005) The influence of tibial slope on maximal flexion after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 13:193–196
Catani F, Leardini A, Ensini A, Cucca G, Bragonzoni L, Toksvig-Larsen S, Giannini S (2004) The stability of the cemented tibial component of total knee arthroplasty posterior cruciate-retaining versus posterior-stabilized design1 1No benefits or funds were received in support of this study. J Arthroplasty 19:775–782
Chambers AW, Wood AR, Kosmopoulos V, Sanchez HB, Wagner RA (2016) Effect of posterior tibial slope on flexion and anterior-posterior tibial translation in posterior cruciate-retaining total knee arthroplasty. J Arthroplasty 31:103–106
Figueroa J, Guarachi JP, Matas J, Arnander M, Orrego M (2016) Is computed tomography an accurate and reliable method for measuring total knee arthroplasty component rotation? Int Orthop 40:709–714
Fucentese SF, Meier P, Jud L, Köchli G-L, Aichmair A, Vlachopoulos L, Fürnstahl P (2020) Accuracy of 3D-planned patient specific instrumentation in high tibial open wedge valgisation osteotomy. J Exp Orthop 7:7. https://doi.org/10.1186/s40634-020-00224-y
Henckel J, Richards R, Lozhkin K, Harris S, y Baena FMR, Barrett ARW, Cobb JP (2006) Very low-dose computed tomography for planning and outcome measurement in knee replacement. J Bone Joint Surg Br 88-B:1513–1518
Hirschmann MT, Moser LB, Amsler F, Behrend H, Leclercq V, Hess S (2019) Phenotyping the knee in young non-osteoarthritic knees shows a wide distribution of femoral and tibial coronal alignment. Knee Surg Sports Traumatol Arthrosc 27:1385–1393
Hirschmann MT, Moser LB, Amsler F, Behrend H, Leclerq V, Hess S (2019) Functional knee phenotypes: a novel classification for phenotyping the coronal lower limb alignment based on the native alignment in young non-osteoarthritic patients. Knee Surg Sports Traumatol Arthrosc 27:1394–1402
Hoch A, Jud L, Roth T, Vlachopoulos L, Fürnstahl P, Fucentese SF (2020) A real 3D measurement technique for the tibial slope: differentiation between different articular surfaces and comparison to radiographic slope measurement. BMC Musculoskelet Disord 21:635. https://doi.org/10.1186/s12891-020-03657-9
Hochreiter B, Hirschmann MT, Amsler F, Behrend H (2019) Highly variable tibial tubercle–trochlear groove distance (TT–TG) in osteoarthritic knees should be considered when performing TKA. Knee Surg Sports Traumatol Arthrosc 27:1403–1409
Jud L, Vlachopoulos L, Beeler S, Tondelli T, Fürnstahl P, Fucentese SF (2020) Accuracy of three dimensional-planned patient-specific instrumentation in femoral and tibial rotational osteotomy for patellofemoral instability. Int Orthop. https://doi.org/10.1007/s00264-020-04496-y
Kang K-T, Koh Y-G, Son J, Kwon O-R, Lee J-S, Kwon SK (2017) Biomechanical effects of posterior condylar offset and posterior tibial slope on quadriceps force and joint contact forces in posterior-stabilized total knee arthroplasty. Biomed Res Int 2017:1–12
Kang K-T, Kwon SK, Son J, Kwon O-R, Lee J-S, Koh Y-G (2018) The increase in posterior tibial slope provides a positive biomechanical effect in posterior-stabilized total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 26:3188–3195
Kuwano T, Urabe K, Miura H, Nagamine R, Matsuda S, Satomura M, Sasaki T, Sakai S, Honda H, Iwamoto Y (2005) Importance of the lateral anatomic tibial slope as a guide to the tibial cut in total knee arthroplasty in Japanese patients. J Orthop Sci 10:42–47
Lustig S, Scholes CJ, Leo SPM, Coolican M, Parker DA (2013) Influence of soft tissues on the proximal bony tibial slope measured with two-dimensional MRI. Knee Surg Sports Traumatol Arthrosc 21:372–379
Malviya A, Lingard EA, Weir DJ, Deehan DJ (2009) Predicting range of movement after knee replacement: the importance of posterior condylar offset and tibial slope. Knee Surg Sports Traumatol Arthrosc 17:491–498
Meier M, Janssen D, Koeck FX, Thienpont E, Beckmann J, Best R (2020) Variations in medial and lateral slope and medial proximal tibial angle. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-020-06052-y
Meier M, Zingde S, Best R, Schroeder L, Beckmann J, Steinert AF (2020) High variability of proximal tibial asymmetry and slope: a CT data analysis of 15,807 osteoarthritic knees before TKA. Knee Surg Sports Traumatol Arthrosc 28:1105–1112
Meric G, Gracitelli GC, Aram L, Swank M, Bugbee WD (2015) Tibial slope is highly variable in patients undergoing primary total knee arthroplasty: analysis of 13,546 computed tomography scans. J Arthroplasty 30:1228–1232
Mizu-uchi H, Colwell CW, Matsuda S, Flores-Hernandez C, Iwamoto Y, D’Lima DD (2011) Effect of total knee arthroplasty implant position on flexion angle before implant-bone impingement. J Arthroplasty 26:721–727
Naendrup J-H, Drouven SF, Shaikh HS, Jaecker V, Offerhaus C, Shafizadeh ST, Pfeiffer TR (2020) High variability of tibial slope measurement methods in daily clinical practice: comparisons between measurements on lateral radiograph, magnetic resonance imaging, and computed tomography. Knee. https://doi.org/10.1016/j.knee.2020.01.013
Nunley RM, Nam D, Johnson SR, Barnes CL (2014) Extreme variability in posterior slope of the proximal tibia: measurements on 2395 CT scans of patients undergoing UKA? J Arthroplasty 29:1677–1680
Pangaud C, Laumonerie P, Dagneaux L, LiArno S, Wellings P, Faizan A, Sharma A, Ollivier M (2020) Measurement of the posterior tibial slope depends on ethnicity, sex, and lower limb alignment: a computed tomography analysis of 378 healthy participants. Orthop J Sports Med. https://doi.org/10.1177/2325967119895258
Shi X, Shen B, Kang P, Yang J, Zhou Z, Pei F (2013) The effect of posterior tibial slope on knee flexion in posterior-stabilized total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 21:2696–2703
Sierra RJ, Berry DJ (2008) Surgical technique differences between posterior-substituting and cruciate-retaining total knee arthroplasty. J Arthroplasty 23:20–23
Singh G, Tan JH, Sng BY, Awiszus F, Lohmann CH, Nathan SS (2013) Restoring the anatomical tibial slope and limb axis may maximise post-operative flexion in posterior-stabilised total knee replacements. Bone Joint J 95-B:1354–1358
Utzschneider S, Goettinger M, Weber P, Horng A, Glaser C, Jansson V, Müller PE (2011) Development and validation of a new method for the radiologic measurement of the tibial slope. Knee Surg Sports Traumatol Arthrosc 19:1643–1648
Wasieliwski RC, Galante JO, Leighty RM, Natarajan RN, Rosenberg AG (1994) Wear patterns on retrieved polyethylene tibial inserts and their relationship to technical considerations during total knee arthroplasty. Clin Orthop Relat Res 299:31–43
Wittenberg S, Sentuerk U, Renner L, Weynandt C, Perka CF, Gwinner C (2019) Importance of the tibial slope in knee arthroplasty. Der Orthopade 49:10–17
Funding
No direct support for this project was received.
Author information
Authors and Affiliations
Contributions
AKC and BH were involved in the conceptualization and design of the study. AKC, BH, and FA were involved in analysis and interpretation of the data. AKC and BH were drafting the manuscript. SH, HB, and MTH were involved in manuscript revision. All authors edited, read, and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
MTH and FA are paid by DepuySynthes, Lima, S&N, Symbios. MTH is a board member of ESSKA, EKA and DKG, and a member of the editorial team of KSSTA, AP SMART, World J Orthopaedics. All the other authors declare that they have no competing interests.
Ethics approval and consent to participate
Approval was obtained from the local ethical committee (Ethikkommission Nordwest- und Zentralschweiz, ID 2018-00223). All procedures performed were in accordance with the ethical standards of the institutional and/or the national research committees and with the 1964 Declaration of Helsinki and its later amendments or with comparable ethical standards.
Informed consent
Informed consent was obtained from all participants of the study.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Calek, AK., Hochreiter, B., Hess, S. et al. High inter- and intraindividual differences in medial and lateral posterior tibial slope are not reproduced accurately by conventional TKA alignment techniques. Knee Surg Sports Traumatol Arthrosc 30, 882–889 (2022). https://doi.org/10.1007/s00167-021-06477-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-021-06477-z