Abstract
Purpose
The primary objective was to compare the functional outcomes after an isolated MPFL reconstruction using either a quasi-anatomical technique (group A) or an anatomical MPFL reconstruction (group B). The secondary objectives were to compare the rates of redislocation, range-of-motion and subjective patellar instability (Smillie test).
Methods
A multicenter longitudinal prospective comparative study was performed. Group A had 29 patients and 28 were included in Group B. Patients with trochlear dysplasia types C and D and patients who had undergone a trochleoplasty, a distal realignment or patella distalization concurrently with MPFL reconstruction were excluded. The main evaluation criterion was the Kujala functional score.
Results
The mean postoperative Kujala was 90.4 (89.4 in group A and 92.1 in group B). Upon comparing the mean difference between pre- and post-operative values, no differences were detected between the two groups (n.s).
Conclusions
Isolated quasi-anatomical MPFL reconstruction using a gracilis tendon autograft for recurrent patellar dislocation provides outcomes as good as the isolated anatomical MPFL reconstruction in patients with no trochlear dysplasia up to those with trochlear dysplasia type A and B at the 2–5 years follow-up.
Level of evidence
Level IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lateral patellar dislocation is a significant cause of knee injuries [2]. In this pathology, medial patellofemoral ligament (MPFL) reconstruction has a high rate of success for patients with patellofemoral instability. However, the complication rate associated with this procedure is 26.1% [28]. A frequently reported complication after MPFL reconstruction is the loss of knee flexion (13.4% of all complications), often associated with medial knee pain [28]. Enderlein et al., in a prospective study, found the incidence of medial knee pain after MPFL reconstruction in around 30% of the cases [5]. The fact that over-tensioning of the MPFL can cause an overload of the medial portion of the patella with a subsequent medial pain syndrome is well known [4, 6, 30]. The stiffness of the surgical construct may be one of the causes of that overload. In the Chassaing technique, the proper tension of the graft is determined after moving the knee through flexion and extension movements to assess the resulting patellar stability [3]. In the Schottle technique, the graft tension is deemed satisfactory when the lateral edge of the patella is aligned with the lateral edge of the trochlea [25].
Many MPFL reconstruction techniques have been described. Alm et al. [1] studied a surgical technique in which the gracilis or semitendinosus tendons are left intact in their insertion, looped around the adductor magnus tendon and attached at the medial facet of the patella in children and adolescents. They reported elevated redislocation rates due to maltracking of the patella in patients with patella alta, trochlear dysplasia or an elevated tibial tuberosity to trochlear groove distance (TT–TG) [1]. A modification of that technique was later described [17, 19]. This is a quasi-anatomical MPFL reconstruction technique that uses a gracilis tendon autograft attached to the patella at the anatomical ligament footprint and passed underneath the adductor magnus tendon, which is used as a pulley for femoral fixation. It has been shown that this technique provides good results in association with distal realignment (in cases of a preoperative TT–TG distance exceeding 20 mm), and/or patella distalization (in cases of patella alta as defined by a Caton–Deschamps index ˃ 1.2) [17]. Several biomechanical, anatomical and finite elements studies supporting the use of a non-anatomical technique have already been published [16, 18, 21]. No mention has been made relative to the results of this kind of patellofemoral ligament reconstruction when carried out on mature knees as an isolated surgical procedure.
The primary objective of the present study was to compare the functional outcomes after an isolated MPFL reconstruction using either a quasi-anatomical technique or an anatomical MPFL reconstruction. The secondary objectives were to compare the rates of redislocation, range-of-motion and subjective patellar instability in accordance with the Smillie test of those same patients.
The hypothesis was that an isolated quasi-anatomical MPFL reconstruction using a gracilis tendon autograft for recurrent patellar dislocation provides outcomes as good as a traditional anatomical technique in patients with no trochlear dysplasia up to those with moderate trochlear dysplasia at 2–5 years of follow-up.
Materials and methods
The study was intended to be a non-inferiority study with respect to a standard validated technique.
IRB approval
The study was approved by the ethics committee of ICATME—Institut Universitari Dexeus (2/2014).
Patients
The following inclusion criteria were used: (1) patients with objective recurrent (minimum two episodes of dislocation) patellar instability operated on from 2014 to 2016, (2) a patient agreement to return for a minimum 2-year follow-up period and (3) patient consent to participate in the study.
The following exclusion criteria were used: (1) patients with TT–TG realignment or patella distalization during the surgery (TT–TG > 20 mm and Caton–Deschamps index > 1.2), (2) patients who had undergone a trochleoplasty concurrently with MPFL reconstruction, (3) patients with grade C or D trochlear dysplasia, (4) subjects who could not fill out the questionnaires by themselves.
At the end of the study, 31 patients were consecutively operated on with an isolated quasi-anatomical MPFL reconstruction (group A) and 28 patients were consecutively operated on with an isolated anatomical MPFL reconstruction (group B). Two patients were lost during follow-up in the study group and none in the control group.
Finally, 29 and 28 patients were included in each group, respectively. The two groups were analyzed and considered homogenous and comparable. A complete description of the baseline characteristics is provided in Table 1.
Surgical procedure
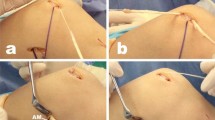
Group A The homolateral gracilis tendon (GT) autograft was always the graft of choice. A 2-cm vertical skin incision 1 cm medial to the anterior tibial tuberosity was used to approach the gracilis tendon (GT). After exposing the sartorial fascia, it was horizontally incised in line with the palpable GT. It is important not to go any deeper so as to prevent injury to the underlying superficial medial collateral ligament. Both the gracilis (proximal) and semitendinosus (distal) were identified and separated. After freeing the tibial attachment of the GT, a #2 high-strength suture (Hi-Fi, ConMed, Largo, FL) with a Krackow mattress was placed at its distal end. The GT was harvested using a closed tendon stripper and another similar suture was placed at the proximal end. The tendon was sized both in length and diameter and stored wrapped in vancomycin-soaked gauze. The doubled graft should be at least 90 mm in length (total graft length 180 mm) to properly reconstruct the MPFL. The diameter was checked just to be sure that the tendon could easily be passed through the patellar tunnels. The tendon was sized and stored in gauze soaked in vancomycin [20]. A 2-cm vertical skin incision was then made over the superior medial border of the patella to expose its proximal third. Two convergent drill holes (usually 4.5 mm in size) approximately 10 mm in depth were created leaving a bone bridge of 10 mm, thereby obtaining a V-shaped tunnel. Another 2–3-cm skin incision was made along the adductor magnus (AM) tendon, slightly proximal to the medial femoral epicondyle. The tendon of the AM was identified and dissected so as to be used as a pulley for the graft. The graft was then passed through the patella, then under the fascia and finally looped around the AM tendon back to the patella. The knee was cycled several times through full range-of-motion while keeping the graft under slight tension. Finally, both graft ends were sutured together at 30° of flexion with #0 high-resistance non-absorbable sutures. Tension was calculated on the basis that the patella could still be lateralized manually some 10 mm to prevent over-constraint. The lower limb was finally immobilized in a brace locked at full extension. No lateral retinacular release was performed in the present series.
Group B An anatomic double-bundle static MPFL reconstruction using homolateral semitendinosus autograft was always carried out. A 2-cm vertical skin incision was then made centered over the junction of the medial and middle thirds of the patella to expose its proximal third. Two convergent drill holes (usually 4.5 mm in size) approximately 10 mm deep were created leaving a bone bridge of 10 mm, thereby obtaining a V-shaped tunnel. Another 3-cm skin incision was made over the femoral insertion of the MPFL. The anatomic femoral insertion of the MPFL is always located between the medial femoral epicondyle (MFE) and the adductor tubercle (AT), usually 10 mm distally from the latter. The graft was then passed through the patella, then under the fascia and finally inserted to the anatomic footprint point without fluoroscopy at 30° of flexion by a suture anchor with enough tension to make the graft taut but without pulling. No lateral retinacular release was performed in the present series. The lower limb was finally immobilized in a brace locked at full extension.
Partial weightbearing was allowed immediately after surgery as tolerated, with a knee brace locked at full extension. Range-of-motion exercises were encouraged after 2 weeks and progressed to full range of motion by the sixth week. The brace was discarded at approximately 3 weeks depending on the status of the quadriceps. The protocol was the same for both groups and all the patients followed.
End points
The main evaluation criterion was the Kujala functional score [11]. Secondary evaluation criteria were functional scores consisting of the IKDC subjective [8], Tegner [29] and VAS, the rate of redislocation of the patella, subjective patellar instability in accordance with the Smillie test (apprehension when the patella is lateralized by the examiner) and range-of-motion measured with a goniometer.
The functional scores were collected by a single independent surgeon with a computerized questionnaire. The clinical examination data were collected by each surgeon in a prospective clinical evaluation.
Statistical analysis
Because a sample size calculation was not made, it was decided to carry out a posteriori power sample analysis at the end of the study. We conducted the analysis to determine if there was at least 80% power and a 95% confidence interval in our sample size to test the primary outcome of our study to confirm our hypothesis. Therefore, we performed a retrospective noninferiority power calculation using the Kujala knee score as a primary endpoint. A10-point lower Kujala score was considered a clinically relevant inferior clinical outcome. Based on previous studies, the standard deviation (SD) for the Kujala score was assumed to be 15 [5]. As result of our post hoc power analysis, the calculation resulted in a sample size of 28 or less subjects per group. This confirms the validity of the sample analyzed in the present study. Previous studies comparing the clinical results of two different MPFL reconstruction techniques described the same sample size when the noninferiority power calculation using the Kujala knee score as primary endpoint was calculated at the beginning of the study [12].
Categorical variables are expressed as frequencies and percentages, while continuous variables were described with mean and standard deviation. The differences between pre- and post-surgery were assessed with the Student's t test for paired data and the comparison between groups was performed with Student's t test for independent data. Person's correlation coefficient was also used to assess the relationship between the ICD and TA-GT along with other continuous variables. For all the analyses, two-sided p values of less than 0.05 were considered as statistically significant. The statistical analysis was performed using the SPSS 23 (SPSS, Chicago, IL) package.
Results
133 patients were operated on for recurrent patellar dislocation in the two institutions. 31 of them had an anterior tuberosity distalization and/or medialization, 11 had atrochleoplasty and 32 were excluded for having a grade C or D trochlear dysplasia. The baseline characteristics of the two groups are detailed in Table 1.
The mean postoperative Kujala was 90.4 ± 8.6, being 89.3 ± 8.5 in group A and 92.1 ± 9 in group B. No statistical differences were found between the two groups with regard to the improvement in the Kujala score, the improvement in the IKDC subjective score, the mean post-operative Tegner score, and the mean VAS decrease (Table 2).
With a linear regression, the influence of the CDI and type of trochlear dysplasia on the postoperative score and postoperative VAS were evaluated without identifying any correlation or any difference between the two groups. The evaluation of the influence of the TT–TG score highlighted a statistical correlation (p = 0.042) between increased TT–TG values and a decreased postoperative Kujala score. No differences were detected between the two groups.
A group comparison between patients with no trochlear dysplasia, Type A and type B dysplasia were done. No differences between the groups in terms of postoperative Kujala (n.s), postoperative IKDC (n.s) or postoperative VAS (n.s) were observed.
Only one postoperative patellar dislocation occurred. It was in group A and it happened at 8 months postoperative due to a traumatic accident during sport activities. The baseline characteristics of this patient were: dysplasia type A, TT–TG distance of 16 mm and a CDI of 1.2.
The mean postoperative range-of-motion was 133° ± 7 in group A and 134° ± 9 in group B. There was no statistical difference between the two groups (n.s). Neither were there any differences in terms of the preoperative values (n.s).
Subjective patellar instability was present in only two cases postoperatively, one in each group. In both cases, no further patellar dislocation occurred, and the patients were pain free.
Discussion
The most important finding of the present study was that an isolated quasi-anatomical MPFL reconstruction using a gracilis tendon autograft for recurrent patellar dislocation provides outcomes as good as the classical anatomical technique at 2–5 years follow-up in patients with no trochlear dysplasia up to those with moderate trochlear dysplasia.
Our results were verified by comparing the values found in our study with those found in previous published studies. In a meta-analysis, a mean postoperative Kujala score of 85.8 (95% CI 81.6–90.0) was found by Schneider et al. [24]. The pooled estimated mean postoperative Tegner score was 5.7, with 84.1% (95% CI 71.1–97.1%) of the patients returning to sports after surgery. The pooled total risk of recurrent instability after surgery was 1.2% (95% CI 0.3–2.1%), with a positive apprehension sign risk of 3.6% (95% CI 0–7.2%) and a reoperation risk of 3.1% (95% CI 1.1–5.0%). The studies were included without regard to the type of fixation. Furthermore, the grafts used were a semi-tendinosus autograft, a gracilis autograft, a quadriceps tendon or an autologous patellar tendon autograft. In a systematic review of 14 articles, Longo et al. [14] found that the most frequently used score was the Kujala score with a mean value of 83.26. Functional failures ranged from 0% to 8.8%. Major complications were not described. Minor complications ranged from 0 to 40%. Reoperations ranged from 4.5% to 17.7%. In another systematic review of isolated patellofemoral reconstruction, McNeilan et al. [15] described a mean Kujala score improvement for all the included patients ranging from 59.9 preoperatively to 89.1 postoperatively. The overall complication rate identified in that study was only 5.8%. The most commonly reported complication in adults was persistent subjective patellar instability in accordance with the Smillie test, without luxation in 1.8% of the cases.
There are several arguments that have advocated for the use of the adductor magnus tendon as a pulley for the graft instead of inserting it in the traditional Schottle point. According to Sanchis-Alfonso et al. [22, 23], the radiographic method described by Schottle et al. [26] does not ensure a precise location of the femoral fixation point in MPFL reconstruction surgery, from an anatomic standpoint. A mispositioned femoral tunnel occurs in between 31 and 71% of MPFL reconstructions [32]. The study done by Servien et al. also highlights the difficulty of a reproducible MPFL reconstruction with only 65–69% of the femoral tunnels well positioned [27]. Another study demonstrates that radiographic localization of the MPFL femoral tunnel results in inaccurate tunnel placement on a true lateral radiograph. This happens when there is deviation from a true lateral fluoroscopic image, which can be difficult to obtain intraoperatively [33]. For Melegari et al. [16], the use of the non-isometric attachment point of the adductor tubercle in medial patellofemoral ligament reconstruction does not alter the knee contact area or contact pressures as compared with isometric femoral attachment at the posterior medial epicondyle. For Tischer et al. [31], in the case of a patella alta, a slightly more proximal femoral insertion is beneficial for the biomechanical behaviour of the reconstructed MPFL, which due to the greater lengthening of the MPFL occurs for the first 20° of knee flexion in comparison to a normal patella height.
One of the strengths of this study is that patients with an isolated reconstruction of the MPFL were compared to avoid the bias generated by the other surgical techniques like distalization of the patella or medialization of the tibial tuberosity. The results of MPFL reconstruction using the present technique in association with a distal realignment procedure have been already shown [17].
Using an isolated reconstruction of the MPFL in patients with trochlear dysplasia could be criticized. A study associates trochlear dysplasia with poorer MPFL reconstruction clinical outcomes [9]. Furthermore, severe trochlear dysplasia is the most important predictor of residual patellofemoral instability after isolated MPFL reconstruction [10]. For these reasons, patients with dysplasia type C or D have been excluded from the present series.
TT–TG realignment or patella distalization was not performed in four young patients without closed growth plates, despite having an elevated TT–TG or a patella alta to prevent growth deviations. This was also the case for six patients with a TT–TG or a CDI at the upper edge of the accepted range of values (20 and 1.2, respectively). Even so, the subgroup of patients with a TT–TG ≥ 20 and the subgroup of patients with a CDI ≥ 1.2 did not show worse clinical outcomes or a higher percentage of re-dislocation.
The quasi-anatomical technique provides several advantages. It is an inexpensive procedure as no implants are used. The femoral physeal plate of young patients is not affected as no tunnel needs to be drilled and no hardware is needed to fix the graft to the bone. Moreover, no irradiation is called for as no intraoperative fluoroscopy is called for during surgery. Finally, the elastic fixation may provide better control over the possibility of medial patellofemoral over-constraint compared to the bone fixation of the graft, which seem to be more rigid than the “elastic fixation” [22].
This study had several limitations. The patients in the two groups were not operated on by the same surgeon, which can introduce a performance bias. A gracilis tendon was used in group A, while a semi-tendinosus tendon was used in group B. No radiographic analysis of the residual patellar tilt was done, but some studies claim that MPFL reconstruction produces no improvement in patellar tilt [7, 13]. Additionally, the patients were not randomized, but the two groups were homogeneous in terms of preoperative characteristics.
Conclusions
Isolated quasi-anatomical MPFL reconstruction using a gracilis tendon autograft for recurrent patellar dislocation provides outcomes as good as the isolated anatomical MPFL reconstruction in patients with no trochlear dysplasia or trochlear dysplasia type A and B at 2–5 years follow-up.
References
Alm L, Krause M, Mull C, Frosch K-H, Akoto R (2017) Modified adductor sling technique: a surgical therapy for patellar instability in skeletally immature patients. Knee 24:1282–1288
Askenberger M, Ekström W, Finnbogason T, Janarv P-M (2014) Occult Intra-articular knee injuries in children with hemarthrosis. Am J Sports Med 42:1600–1606
Chassaing V, Trémoulet J (2005) Medial patellofemoral ligament reconstruction with gracilis autograft for patellar instability. Rev Chir Orthop Reparatrice Appar Mot 91:335–340
Chouteau J (2016) Surgical reconstruction of the medial patellofemoral ligament. Orthop Traumatol Surg Res 102:S189–194
Enderlein D, Nielsen T, Christiansen SE, Faunø P, Lind M (2014) Clinical outcome after reconstruction of the medial patellofemoral ligament in patients with recurrent patella instability. Knee Surg Sports Traumatol Arthrosc 22:2458–2464
Geßlein M, Roessler PP, Schüttler KF, Biber R, Bail HJ, Efe T (2015) Complications and failure of MPFL reconstruction with free tendon grafts in cases of patellofemoral instability. Technol Health Care 23:659–666
Gobbi RG, Demange MK, de Ávila LFR, de Araújo Filho JAB, Moreno RA, Gutierrez MA, de Sá Rebelo M, Tírico LEP, Pécora JR, Camanho GL (2017) Patellar tracking after isolated medial patellofemoral ligament reconstruction: dynamic evaluation using computed tomography. Knee Surg Sports Traumatol Arthrosc 25:3197–3205
Hefti F, Müller W, Jakob RP, Stäubli HU (1993) Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc 1:226–234
Hiemstra LA, Kerslake S, Loewen M, Lafave M (2016) Effect of trochlear dysplasia on outcomes after isolated soft tissue stabilization for patellar instability. Am J Sports Med 44:1515–1523
Kita K, Tanaka Y, Toritsuka Y, Amano H, Uchida R, Takao R, Horibe S (2015) Factors affecting the outcomes of double-bundle medial patellofemoral ligament reconstruction for recurrent patellar dislocations evaluated by multivariate analysis. Am J Sports Med 43:2988–2996
Kujala UM, Jaakkola LH, Koskinen SK, Taimela S, Hurme M, Nelimarkka O (1993) Scoring of patellofemoral disorders. Arthroscopy 9:159–163
Lind M, Nielsen T, Miller L, Sørensen OG, Mygind-Klavsen B, Faunø P (2019) No difference in outcome between femoral soft-tissue and screw graft fixation for reconstruction of the medial patellofemoral ligament: a randomized controlled trial. Arthroscopy 35:1130–1137
Liu JN, Brady JM, Kalbian IL, Strickland SM, Ryan CB, Nguyen JT, Shubin Stein BE (2018) Clinical outcomes after isolated medial patellofemoral ligament reconstruction for patellar instability among patients with trochlear dysplasia. Am J Sports Med 46(4):883–889
Longo UG, Berton A, Salvatore G, Migliorini F, Ciuffreda M, Nazarian A, Denaro V (2016) Medial patellofemoral ligament reconstruction combined with bony procedures for patellar instability: current indications, outcomes, and complications. Arthroscopy 32:1421–1427
McNeilan RJ, Everhart JS, Mescher PK, Abouljoud M, Magnussen RA, Flanigan DC (2018) Graft choice in isolated medial patellofemoral ligament reconstruction: a systematic review with meta-analysis of rates of recurrent instability and patient-reported outcomes for autograft, allograft, and synthetic options. Arthroscopy 34:1340–1354
Melegari TM, Parks BG, Matthews LS (2008) Patellofemoral contact area and pressure after medial patellofemoral ligament reconstruction. Am J Sports Med 36:747–752
Monllau JC, Masferrer-Pino À, Ginovart G, Pérez-Prieto D, Gelber PE, Sanchis-Alfonso V (2017) Clinical and radiological outcomes after a quasi-anatomical reconstruction of medial patellofemoral ligament with gracilis tendon autograft. Knee Surg Sports Traumatol Arthrosc 25:2453–2459
Panagopoulos A, van Niekerk L, Triantafillopoulos IK (2008) MPFL reconstruction for recurrent patella dislocation: a new surgical technique and review of the literature. Int J Sports Med 29:359–365
Pérez-Prieto D, Capurro B, Gelber PE, Ginovart G, Reina F, Sanchis-Alfonso V, Monllau JC (2017) The anatomy and isometry of a quasi-anatomical reconstruction of the medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc 25:2420–2423
Pérez-Prieto D, Portillo ME, Torres-Claramunt R, Pelfort X, Hinarejos P, Monllau JC (2018) Contamination occurs during ACL graft harvesting and manipulation, but it can be easily eradicated. Knee Surg Sports Traumatol Arthrosc 26:558–562
Rood A, Hannink G, Lenting A, Groenen K, Koëter S, Verdonschot N, van Kampen A (2015) Patellofemoral pressure changes after static and dynamic medial patellofemoral ligament reconstructions. Am J Sports Med 43:2538–2544
Sanchis-Alfonso V, Ginovart G, Alastruey-López D, Montesinos-Berry E, Monllau JC, Alberich-Bayarri A, Pérez MA (2019) Evaluation of patellar contact pressure changes after static versus dynamic medial patellofemoral ligament reconstructions using a finite element model. J Clin Med 8:2093
Sanchis-Alfonso V, Ramírez-Fuentes C, Montesinos-Berry E, Elía I, Martí-Bonmatí L (2017) Radiographic location does not ensure a precise anatomic location of the femoral fixation site in medial patellofemoral ligament reconstruction. Orthop J Sports Med Med. https://doi.org/10.1177/2325967117739252
Schneider DK, Grawe B, Magnussen RA, Ceasar A, Parikh SN, Wall EJ, Colosimo AJ, Kaeding CC, Myer GD (2016) Outcomes after isolated medial patellofemoral ligament reconstruction for the treatment of recurrent lateral patellar dislocations: a systematic review and meta-analysis. Am J Sports Med 44:2993–3005
Schottle PB, Romero J, Schmeling A, Weiler A (2008) Technical note: anatomical reconstruction of the medial patellofemoral ligament using a free gracilis autograft. Arch Orthop Trauma Surg 128:479–484
Schöttle PB, Schmeling A, Rosenstiel N, Weiler A (2007) Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. Am J Sports Med 35:801–804
Servien E, Fritsch B, Lustig S, Demey G, Debarge R, Lapra C, Neyret P (2011) In vivo positioning analysis of medial patellofemoral ligament reconstruction. Am J Sports Med 39:134–139
Shah JN, Howard JS, Flanigan DC, Brophy RH, Carey JL, Lattermann C (2012) A systematic review of complications and failures associated with medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med 40:1916–1923
Tegner Y, Lysholm J (1985) Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res 198:43–49
Thaunat M, Erasmus PJ (2009) Management of overtight medial patellofemoral ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 17:480–483
Tischer T, Geier A, Lenz R, Woernle C, Bader R (2017) Impact of the patella height on the strain pattern of the medial patellofemoral ligament after reconstruction: a computer model-based study. Knee Surg Sports Traumatol Arthrosc 25:3123–3133
Tscholl PM, Ernstbrunner L, Pedrazzoli L, Fucentese SF (2018) The relationship of femoral tunnel positioning in medial patellofemoral ligament reconstruction on clinical outcome and postoperative complications. Arthroscopy 34:2410–2416
Ziegler CG, Fulkerson JP, Edgar C (2016) Radiographic reference points are inaccurate with and without a true lateral radiograph: the importance of anatomy in medial patellofemoral ligament reconstruction. Am J Sports Med 44:133–142
Acknowledgements
We would like to thank Mr. Eric L. Goode for his help with English correction. In addition, the authors thank Sergi Mojal for his expertise in performing the statistical analyses contained in this article.
Funding
No fundings were received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author(s) declare that they have no competing interests.
Ethical approval
The study was approved by the ethics committee of ICATME—Institut Universitari Dexeus (2/2014).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Marot, V., Sanchis-Alfonso, V., Perelli, S. et al. Isolated reconstruction of medial patellofemoral ligament with an elastic femoral fixation leads to excellent clinical results. Knee Surg Sports Traumatol Arthrosc 29, 800–805 (2021). https://doi.org/10.1007/s00167-020-06016-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-06016-2