Abstract
Purpose
Surgeons performing total knee arthroplasty (TKA) on the osteoarthritic valgus deformity often use a posterior stabilized (PS) and semi-constrained implants to substitute for the release of a contracted posterior cruciate ligament (PCL) instead of a cruciate retaining (CR) implant. Calipered kinematic alignment (KA) strives to retain the PCL and use a CR implant. The aim of this study of the windswept deformity was to determine whether the level of implant constraint, outcome scores, and alignment after bilateral calipered KA TKA are different between a pair of knees with a varus and valgus deformity in the same patient.
Methods
A review of a prospectively collected database identified all patients with a windswept deformity treated with bilateral TKA (n = 19) out of 2430 consecutive primary TKAs performed between 2014 and 2019. Operative reports determined the level of implant constraint. Patient response to the Forgotten Joint Score (FJS) and Oxford Knee Score (OKS) assessed outcomes at a mean follow-up of 2.3 years. Postoperative alignment was measured on an A-P computer tomographic scanogram of the limb.
Results
CR implants were used in 15 of 19 (79%) valgus deformities and 17 of 19 (89%) of varus deformities (n.s.). No knees required a semi-constrained implant. There was no difference in the median postoperative FJS and OKS (n.s.), and a 1° or less difference in the mean postoperative distal lateral femoral angle (p = 0.005) and proximal medial tibial angle (n.s.) between the paired varus and valgus knee deformity.
Conclusion
Based on this small series, surgeons that use calipered KA TKA can expect to use CR implants in most patients with windswept deformity and achieve comparable outcome scores and alignment between the paired varus and valgus deformity.
Level of evidence
IV
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
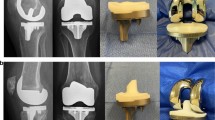
‘Windswept’ deformity refers to a patient with a valgus deformity in one knee and a varus deformity in the other (Fig. 1) [14]. Some authors believe the posterior cruciate ligament (PCL) is often contracted in the valgus deformity and that resecting it and using a posterior stabilized (PS) total knee arthroplasty (TKA) implant is simpler than using a cruciate retaining (CR) implant [4]. TKA treatment of the valgus deformity is associated with more frequent use of ligament releases and semi-constrained implants and with lower outcome scores than the varus deformity [12, 25, 27]. Hence, the unique feature of studying the windswept deformity is that implant constraint, outcome, and alignment can be compared between a pair of knees with a varus and valgus deformity in the same patient.
Composite shows the preoperative weight-bearing radiograph (left image) of a patient with a windswept osteoarthritic deformity with a preoperative valgus deformity (right knee) and varus deformity (left knee). The postoperative anteroposterior scanogram (middle and right image) shows the restoration of similar right and left distal lateral femoral angles (DLFA), proximal medial tibial angles (PMTA) (middle image), and hip–knee–ankle (HKA) angles (right image) in paired knees after treatment with bilateral calipered KA TKA
Calipered kinematic alignment (KA) TKA strives to restore the patient’s pre-arthritic joint lines without releasing the PCL in knees with a varus and valgus deformity. There is growing interest in the KA technique as an alternative to mechanical alignment (MA), because eight studies reported better patient satisfaction, function, ease of recovery, soft tissue balance, flexion, and joint-line and limb alignment than MA TKA [2, 3, 10, 11, 13, 21, 34]. Whereas two other studies reported similar tibial component migration at 2 years [9] and similar clinical outcomes [35].
Because the knee deformity affects the choice of implant constraint and outcome scores, this study aimed to determine whether the level of implant constraint, outcome scores, and alignment after bilateral calipered KA TKA are different between a pair of knees with a varus and valgus deformity in the same patient.
Materials and methods
An Institutional Review Board issued an approval (1439898-1) that allowed a retrospective review of a single surgeon’s existing data in a prospectively collected image and clinical database between January 2014 and January 2019 that contained 2430 knees treated with primary TKA. All patients fulfilled the Centers for Medicare and Medicaid Services guidelines for medical necessity and each knee fulfilled the following criteria including (1) disabling knee pain and functional loss unresolved with nonoperative treatment modalities; (2) radiographic evidence of Kellgren-Lawrence Grade II to IV arthritic change or osteonecrosis; (3) any severity of clinical varus or valgus deformity; (4) and any severity of flexion contracture [30]. The surgeon performed each TKA with the calipered KA technique.
A review of weight-bearing radiographs of bilateral knees exposed during full extension and 30°–45° of flexion identified nineteen patients (ten females, nine males, age 68 ± 7 years) with medial joint space narrowing in one knee and lateral joint space narrowing in the other that were subsequently treated with bilateral calipered KA TKA. Comparisons of preoperative clinical and radiographic characteristics between the pair of knees with a varus and valgus deformity in the same patient are shown in Table 1.
The following is an overview of the previously well-described calipered KA technique [31]. The adjustments for setting the distal and posterior femoral resection guide to restore the patient’s pre-arthritic angle and level of the femoral joint lines are based on knowing that the varus and valgus Grade II–IV Kellgren–Lawrence osteoarthritic knees have negligible bone wear at 0° and 90° and that the mean full thickness cartilage wear approximates 2 mm [6, 16]. The varus–valgus orientation and level of the proximal–distal resection were set so the thicknesses of the distal femoral resections as measured with a caliper made specifically for use with KA (Medacta or Zimmer/Biomet) to within 0 ± 0.5 mm to match those of the condyles of the femoral component after compensating for cartilage wear and kerf of the saw blade. This method was also used to set the internal–external orientation and the level of the anterior–posterior resection. An accuracy analysis showed a mean difference between the femoral component and the target of the patient’s pre-arthritic distal and posterior femoral joint lines of less than 1 mm and 1° [18, 26] (Fig. 2).
Verification worksheet intraoperatively records the caliper measurements and reminds the surgeon to check and make adjustments after each critical surgical step before proceeding to the next. The order of the bone cuts progress from distal femoral to posterior femoral, anterior femoral, chamfer femoral, and tibial resection. Adjustment of the thickness of the distal medial and distal lateral femoral resections as measured with a caliper to within 0 ± 0.5 mm of the thickness of the condyles of the femoral component after compensating for cartilage wear and a ~ 1 mm kerf from the saw cut and 2 mm of cartilage wear when present sets the varus–valgus orientation and proximal–distal coincident with the patient’s pre-arthritic joint line. Adherence to this manufacturing process is responsible for the high accuracy of the calipered KA technique
The knee was balanced by adjusting the proximal–distal position, varus–valgus rotation, and the slope of the tibial resection according to six options in a decision-tree (Fig. 3). The varus–valgus orientation of the resection was set coincident with the native proximal tibial joint line using two verification checks. First, the thicknesses of the medial and lateral tibial condyles were measured at the base of the tibial spines with a caliper and the resection was adjusted until they were equal. Second, with the knee in full extension, the varus–valgus angle of the tibial resection was adjusted, working in 1°–2° increments, until there was negligible medial and lateral liftoff of the trial insert from each condyle of the femoral component during a varus–valgus laxity assessment with the spacer block and trial component. An accuracy analysis showed the proportion of patients with a proximal medial tibial angle (PMTA) of the tibial component within the target of the normal left to right symmetry of the contralateral normal knee was 97% [8, 20]. The slope was set coincident with the native joint line using two verification checks with trial components. The slope and insert thickness were adjusted working in 1°–2° increments until (1) the caliper measurement of the offset of the anterior tibia from the distal medial femoral condyle with the knee in 90° of flexion matched that of the knee at exposure after compensating for any cartilage wear on the distal medial femur; and (2) the passive internal–external rotation of the tibia on the femur approximated ± 15°, which restores native laxity [28, 29]. An accuracy analysis showed a mean difference between the posterior slope of the tibial component and the target of the native posterior slope of 0° [8]. The internal–external (I–E) rotation of the tibial component was set using either an anatomically shaped kinematic tibial template or an anatomically shaped anatomic baseplate. An accuracy analysis showed a mean difference between the I–E rotation of the tibial component and the target of the flexion–extension (F–E) plane of the native knee of 2° or less [24]. Accordingly, these verification checks restore the native rectangular extension space, tibial compartment forces laxities, and alignments of the limb and femoral and tibial joint lines [17, 20, 28, 32, 33]. Cementation of the femoral, tibial, and patella components concluded implantation.
Decision-tree provides six options to balance the cruciate-retaining (CR) component by adjusting insert thickness and proximal–distal position, and varus–valgus orientation, and the slope of the tibial resection without a ligament release. The use of a cruciate-substituting (CS) insert compensates for an incompetent or detached posterior cruciate ligament
For the analysis of implant constraint, a review of the operative report identified the management of the PCL, the number of other ligament releases, the constraint and brand of the implant, and the use of stems and cones. A Chi-square analysis with an α = 0.05 showed that 38 knees provided a power of 0.87 to detect an effect size of 0.5 for the association between the type of knee deformity and the level of implant constraint.
For the analysis of outcome scores, the patient filled-out the Forgotten Joint Score (FJS) (best 100, worst 0), and the Oxford Knee Score (OKS) (best 48, worst 0) for their pair of knees with a varus and valgus deformity on an emailed or postal mailed evaluation sent between April and May 2019.
For the analysis of postoperative alignment, measurements were made by one author blinded to the condition of the preoperative knee on a non-weight bearing anteroposterior and lateral computer tomographic scanograms of the limb obtained on the day of discharge. The radiation dosage of 0.5 mSv is lower than a conventional long-leg radiograph. Adjustment of the rotation of the limb so that the flange was between the posterior condyles of the femoral component limited the projection error from malrotation to approximately ± 1° [7]. A previously described technique measured (1) the distal lateral femoral angle (DLFA) as the varus–valgus angle of the femoral component to the mechanical axis of the femur; (2) the proximal medial tibial angle (PMTA) as the varus–valgus angle of the tibial component to the mechanical axis of the tibia; and 3) the hip–knee–ankle (HKA) angle as the angle of the intersection of the mechanical axis of the femur and tibia using image-analysis software (Horos Imaging Software. https://www.horosproject.org) (Fig. 1) [7, 20, 33]. Values < 90° indicated varus. Values > 90° indicated valgus.
Statistical analysis
Data were analyzed using statistical software (JMP® Pro 14.1.0, www.jmp.com, SAS, Cary, NC, USA). The mean and standard deviation described the distribution of continuous variables. The Shapiro–Wilk test showed a non-normal distribution of the FJS and OKS, so the median and interquartile range (IQR) characterized the distribution. A Chi-Square analysis determined the association between the type of knee deformity and the level of implant constraint. A Wilcoxon Signed Rank or a Paired Student’s t test identified differences in the FJS, OKS, DLFA, PMTA, and HKA angle between a pair of knees with a varus and valgus deformity in the same patient. Significance was p < 0.05.
Results
In terms of implant constraint, CR implants were used in 15 of 19 (79%) valgus deformities and 17 of 19 (89%) of varus deformities (n.s.) (Table 2) No patient required a release of the PCL or a semi-constrained implant. A short tibial stem extension was used in one knee with a valgus deformity. For the eight patients that treated the varus deformity first, the valgus deformity was treated 5 ± 1 months later. For the 11 patients that treated the valgus deformity first, the varus deformity was treated 10 ± 10 months later.
In terms of postoperative outcome scores, there was no differences in the FJS and OKS between paired knees with varus and valgus deformity at a mean follow-up of 2.3 years (range 1–4 years) (Figs. 4, 5). The median FJS was 90 [IQR 69–96] for the valgus deformity and 90 [73–100] for the varus deformity (n.s.). The median OKS was 47 [39–47] for the valgus deformity and 47 for the varus deformity [41–47]) (n.s.). No patient had had an additional knee operation.
Scatter plot shows the mean (x-axis) and the left and right difference (y-axis) of the postoperative Forgotten Joint Score (FJS) (x-markers) for each patient (N = 19), the overall mean difference of 0.3 points (solid line) between the KA TKAs performed on those knees with a preoperative varus or valgus deformity (n.s.), and the 95% CI of the overall mean difference of − 2.7 to 3.3 points (dotted lines)
Scatter plot shows the mean (x-axis) and the left and right difference (y-axis) of the postoperative Oxford Knee Score (OKS) (x-markers) for each patient (N = 19), the overall mean difference of 0.1 points (solid line) between the KA TKAs performed on paired knees with a varus and valgus deformity (n.s.), and the 95% CI of the overall mean difference of − 0.7 to 0.9 points (dotted lines)
In terms of postoperative alignment, the difference was 1° or less for the DLFA, PMTA, HKA angle between the paired knees with varus and valgus deformity (Figs. 6, 7, 8). The mean DLFA was 94° ± 2.1° for the valgus deformity and 93° ± 1.7° for the varus deformity (p = 0.005). The mean PMTA was 87° ± 1.7° for the valgus deformity and 87° ± 1.3° for the varus deformity (n.s.). The mean HKA angle was 91° ± 2.3° for the valgus deformity and 90° ± 2.1°) for the varus deformity (n.s.).
Scatter plot shows the mean (x-axis) and the left and right difference (y-axis) of the postoperative distal lateral femoral angle (DLFA) (x-markers) for eighteen patients (one excluded because of a preoperative malunion of a femoral shaft fracture), the overall mean difference of 1.1° (solid line) between the KA TKAs performed on paired knee with varus and valgus deformity (p = 0.005), the 95% CI of the overall mean difference of 0.4°–1.9° (dotted lines), and the 2 of 18 (11%) patients with a left and right difference greater than ± 3° (circles)
Scatter plot shows the mean (x-axis) and the left and right difference (y-axis) of the postoperative proximal medial tibial angle (PMTA) (x-markers) for eighteen patients (one excluded because of a preoperative malunion of a femoral shaft fracture), the overall mean difference of − 0.1° (solid line) between the KA TKAs performed on paired knee with varus and valgus deformity (n.s.), the 95% CI of the overall mean difference of − 1.1° to 0.9° (dotted lines), and the 2 of 18 (11%) patients with a left and right difference greater than ± 3° (circles)
Scatter plot shows the mean (x-axis) and the left and right difference (y-axis) of the postoperative hip–knee–ankle (HKA) angle (x-markers) for eighteen patients (one excluded because of a preoperative malunion of a femoral shaft fracture), the overall mean difference of 0.9° (solid line) between the KA TKAs performed on paired knee with varus and valgus deformity (n.s.), the 95% CI of the overall mean difference of − 0.3° to 2.2° (dotted lines), and the 3 of 18 (17%) patients with a left and right difference greater than ± 3° (circles)
Discussion
The most important message of the present study was that calipered KA TKA treated both knees of most patients with a windswept deformity with a CR implant and achieved comparable outcome scores and alignment between paired knees with a varus and valgus deformity.
In terms of implant constraint, calipered KA treated the varus and valgus deformity with a CR implant by restoring the patient’s native or pre-arthritic joint line of the knee and by retaining the PCL without the release of other ligaments, which is different from MA [5, 7, 33, 37]. The basis for the treatment of the valgus deformity with KA is the anatomical fact that the lateral femoral condyle is not hypoplastic. As determined by imaging of the femoral condyles perpendicular to the transverse axis of the knee, the mean asymmetry between the radii of the medial and lateral femoral condyle in knees with a varus and valgus deformity is clinically unimportant when aligning a total knee prosthesis [6]. In contrast, the incorrect assumption that lateral femoral condyle is ‘hypoplastic’ is used by MA surgeons to justify the setting of the femoral component distal and posterior relative to the native lateral femoral joint line, which tightens the PCL and the lateral side of the knee. Balancing a tight lateral side often requires stepwise release of the PCL, lateral collateral ligament, lateral retinaculum, and iliotibial band [4, 25]. Hence, the strategies for managing the preoperative varus and valgus deformity are the same for KA and different for MA.
In terms of postoperative outcome scores, KA effectively restored similar FJS and OKS between the paired varus and valgus knee deformity, which is different from MA. MA treatment of a preoperative valgus deformity requires more ligament releases than a preoperative varus deformity. One MA study reported the use of one or more ligament releases in 83% of patients with a preoperative valgus deformity lowered the Knee Society Score 18-points when compared to a subgroup of patients without ligament release [25]. Hence, one explanation for the high outcome scores after calipered KA TKA of the preoperative valgus deformity is that PCL and other ligaments were not released.
In terms of postoperative alignment, both legs had the same joint lines and limb alignment. Some of these joint lines would fit within the varus or valgus 'outlier range' according to the MA criterion. However, categorizing alignment in an 'outlier range' does not predict implant survival or outcome scores after KA TKA and is weakly if not negligibly predictive of implant survival after MA TKA [1, 7, 19, 23, 33]. KA TKA had a high 10-year accepted implant survival of 98.5% regardless of whether the postoperative alignment was in an 'outlier range' [7, 32, 33]. After calipered KA TKA, intra-operative forces in the medial and lateral compartments of patients with an 'outlier range' were comparable to those 'in-range', with no evidence of overload of the medial or lateral tibial compartments [33]. The knee adduction moment after KA TKA is lower than after MA TKA, which is associated with a negligible risk of tibial component failure from a varus mechanism [19, 22]. In contrast, MA changes most patient's pre-arthritic joint lines, which requires ligament releases, causes high tibial compartment forces not correctable to those of the native knee by ligament release, and a high tibial adduction moment [15, 19, 22, 25, 33].
This study has several limitations. First, these results represent a small number of patients (n = 19), which should be confirmed by studies with a larger sample size. Accruing a large sample of patients with windswept deformity is quite challenging because of the extremely low 0.8% incidence out of 2430 consecutive primary TKA performed in a 5-year interval. Achieving a higher sample size is essential to attain sufficient power and to reduce the risk of a Type II error for the assessment of post-operative outcome scores and alignment. The range of preoperative varus and valgus deformities in the present study might not represent the range of all patients with windswept deformity. However, the range of knee deformity in the present study of − 3° for the varus deformity and 11° for the valgus deformity is comparable to the range of − 5° for the varus deformity and 16° for the valgus deformity of the study that used MA TKA [14].
Conclusions
In summary, surgeons that use calipered KA TKA can expect to use CR implants to treat both knees in most patients with windswept deformity and achieve comparable outcome scores and alignment between paired knees with a varus and valgus deformity.
References
Bonner TJ, Eardley WG, Patterson P, Gregg PJ (2011) The effect of post-operative mechanical axis alignment on the survival of primary total knee replacements after a follow-up of 15 years. J Bone Joint Surg Br 93:1217–1222
Calliess T, Bauer K, Stukenborg-Colsman C, Windhagen H, Budde S, Ettinger M (2017) PSI kinematic versus non-PSI mechanical alignment in total knee arthroplasty: a prospective, randomized study. Knee Surg Sports Traumatol Arthrosc 25:1743–1748
Dossett HG, Estrada NA, Swartz GJ, LeFevre GW, Kwasman BG (2014) A randomised controlled trial of kinematically and mechanically aligned total knee replacements: 2-year clinical results. Bone Jt J 96-B:907–913
Favorito PJ, Mihalko WM, Krackow KA (2002) Total knee arthroplasty in the valgus knee. J Am Acad Orthop Surg 10:16–24
Howell SM (2019) Calipered Kinematically Aligned Total Knee Arthroplasty: An Accurate Technique That Improves Patient Outcomes and Implant Survival. Orthopedics 42:126–135
Howell SM, Howell SJ, Hull ML (2010) Assessment of the radii of the medial and lateral femoral condyles in varus and valgus knees with osteoarthritis. J Bone Jt Surg Am 92:98–104
Howell SM, Shelton TJ, Hull ML (2018) Implant survival and function 10 years after kinematically aligned total knee arthroplasty. J Arthroplasty 33:3678–3684
Johnson JM, Mahfouz MR, Midillioglu MR, Nedopil AJ, Howell SM (2017) Three-dimensional analysis of the tibial resection plane relative to the arthritic tibial plateau in total knee arthroplasty. J Exp Orthop 4:27
Laende EK, Richardson CG, Dunbar MJ (2019) A randomized controlled trial of tibial component migration with kinematic alignment using patient-specific instrumentation versus mechanical alignment using computer-assisted surgery in total knee arthroplasty. Bone Jt J 101-B:929–940
MacDessi SJ, Griffiths-Jones W, Chen DB, Griffiths-Jones S, Wood JA, Diwan AD et al (2020) Restoring the constitutional alignment with a restrictive kinematic protocol improves quantitative soft-tissue balance in total knee arthroplasty: a randomized controlled trial. Bone Jt J 102-B:117–124
Matsumoto T, Takayama K, Ishida K, Hayashi S, Hashimoto S, Kuroda R (2017) Radiological and clinical comparison of kinematically versus mechanically aligned total knee arthroplasty. Bone Jt J 99-B:640–646
Mazzotti A, Perna F, Golinelli D, Quattrini I, Stea S, Bordini B et al (2019) Preoperative valgus deformity has twice the risk of failure as compared to varus deformity after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 27:3041–3047
McEwen PJ, Dlaska CE, Jovanovic IA, Doma K, Brandon BJ (2020) Computer-assisted kinematic and mechanical axis total knee arthroplasty: a prospective randomized controlled trial of bilateral simultaneous surgery. J Arthroplasty 35:443–450
Meding JB, Anderson AR, Ritter MA, Faris PM, Keating EM (2000) Windswept deformity in bilateral total knee arthroplasty. J Arthroplasty 15:562–566
Meneghini RM, Ziemba-Davis MM, Lovro LR, Ireland PH, Damer BM (2016) Can intraoperative sensors determine the “Target” ligament balance? Early outcomes in total knee arthroplasty. The Journal of Arthroplasty 31:2181–2187
Nam D, Lin KM, Howell SM, Hull ML (2014) Femoral bone and cartilage wear is predictable at 0° and 90° in the osteoarthritic knee treated with total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 22:2975–2981
Nedopil AJ, Howell SM, Hull ML (2019) Deviations in femoral joint lines using calipered kinematically aligned TKA from virtually planned joint lines are small and do not affect clinical outcomes. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-019-05776-w
Nedopil AJ, Howell SM, Hull ML (2016) Does malrotation of the tibial and femoral components compromise function in kinematically aligned total knee arthroplasty? Orthop Clin N Am 47:41–50
Nedopil AJ, Howell SM, Hull ML (2017) What mechanisms are associated with tibial component failure after kinematically-aligned total knee arthroplasty? Int Orthop 41:1561–1569
Nedopil AJ, Singh AK, Howell SM, Hull ML (2018) Does calipered kinematically aligned TKA restore native left to right symmetry of the lower limb and improve function? J Arthroplasty 33:398–406
Niki Y, Nagura T, Kobayashi S, Udagawa K, Harato K (2020) Who will benefit from kinematically aligned total knee arthroplasty? Perspectives on patient-reported outcome measures. J Arthroplasty 35(438–442):e432
Niki Y, Nagura T, Nagai K, Kobayashi S, Harato K (2018) Kinematically aligned total knee arthroplasty reduces knee adduction moment more than mechanically aligned total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 26:1629–1635
Parratte S, Pagnano MW, Trousdale RT, Berry DJ (2010) Effect of postoperative mechanical axis alignment on the fifteen-year survival of modern, cemented total knee replacements. J Bone Joint Surg Am 92:2143–2149
Paschos NK, Howell SM, Johnson JM, Mahfouz MR (2017) Can kinematic tibial templates assist the surgeon locating the flexion and extension plane of the knee? Knee 24:1006–1015
Peters CL, Jimenez C, Erickson J, Anderson MB, Pelt CE (2013) Lessons learned from selective soft-tissue release for gap balancing in primary total knee arthroplasty: an analysis of 1216 consecutive total knee arthroplasties: AAOS exhibit selection. J Bone Jt Surg Am 95:e152
Riviere C, Iranpour F, Harris S, Auvinet E, Aframian A, Chabrand P et al (2017) The kinematic alignment technique for TKA reliably aligns the femoral component with the cylindrical axis. Orthop Traumatol Surg Res 103:1069–1073
Rossi R, Rosso F, Cottino U, Dettoni F, Bonasia DE, Bruzzone M (2014) Total knee arthroplasty in the valgus knee. Int Orthop 38:273–283
Roth JD, Howell SM, Hull ML (2019) Analysis of differences in laxities and neutral positions from native after kinematically aligned TKA using cruciate retaining implants. J Orthop Res 37:358–369
Roth JD, Howell SM, Hull ML (2015) Native knee laxities at 0°, 45°, and 90° of flexion and their relationship to the goal of the gap-balancing alignment method of total knee arthroplasty. J Bone Jt Surg Am 97:1678–1684
Services CfMaM (2012) Documenting medical necessity for major joint replacement (hip and knee) SE 1236. pp 1–5. Available at: https://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/2012-Transmittals-Items/SE1236.html
Shelton TJ, Gill M, Athwal G, Howell SM, Hull ML (2019) Outcomes in patients with a calipered kinematically aligned TKA that already had a contralateral mechanically aligned TKA. J Knee Surg. https://doi.org/10.1055/s-0039-1693000
Shelton TJ, Howell SM, Hull ML (2019) Is there a force target that predicts early patient-reported outcomes after kinematically aligned TKA? Clin Orthop Relat Res 477:1200–1207
Shelton TJ, Nedopil AJ, Howell SM, Hull ML (2017) Do varus or valgus outliers have higher forces in the medial or lateral compartments than those which are in-range after a kinematically aligned total knee arthroplasty? Limb and joint line alignment after kinematically aligned total knee arthroplasty. Bone Jt J 99-B:1319–1328
Waterson HB, Clement ND, Eyres KS, Mandalia VI, Toms AD (2016) The early outcome of kinematic versus mechanical alignment in total knee arthroplasty: a prospective randomised control trial. Bone Jt J 98-B:1360–1368
Young SW, Walker ML, Bayan A, Briant-Evans T, Pavlou P, Farrington B (2017) The Chitranjan S. Ranawat Award: no difference in 2-year functional outcomes using kinematic versus mechanical alignment in TKA: a randomized controlled clinical trial. Clin Orthop Relat Res 475:9–20
Funding
The authors report that there was no funding for this research project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Our ethical committee approved the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Howell, S.M., Shelton, T.J., Gill, M. et al. A cruciate-retaining implant can treat both knees of most windswept deformities when performed with calipered kinematically aligned TKA. Knee Surg Sports Traumatol Arthrosc 29, 437–445 (2021). https://doi.org/10.1007/s00167-020-05968-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-05968-9