Abstract
Purpose
Kinematic alignment in TKA is supposed to restore function by aligning the components to the premorbid flexion–extension axis instead of altering the joint line and natural kinematic axes of the knee. The purpose of this study was to compare mechanically aligned TKA to kinematic alignment.
Methods
In this study, 200 patients underwent TKA and were randomly assigned to 2 groups: 100 TKAs were performed using kinematic alignment with custom-made cutting guides in order to complete cruciate-retaining TKA; the other 100 patients underwent TKA that was manually performed using mechanical alignment. The WOMAC and combined Knee Society Score (KSS), as well as radiological alignment, were determined as outcome parameters at the 12-month endpoint.
Results
WOMAC and KSS significantly improved in both groups. There was a significant difference in both scores between groups in favour of kinematic alignment. Although the kinematic alignment group demonstrated significantly better overall results, more outliers with poor outcomes were also seen in this group. A correlation between post-operative alignment deviation from the initial plan and poor outcomes was also noted. The most important finding of this study is that applying kinematic alignment in TKA achieves comparable results to mechanical alignment in TKA. This study also shows that restoring the premorbid flexion–extension axis of the knee joint leads to better overall functional results.
Conclusion
Kinematic alignment is a favourable technique for TKA.
Clinical relevance
The kinematic alignment idea might be a considerable alternative to mechanical alignment in the future.
Level of evidence
II.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Classic mechanical alignment (MA) in total knee arthroplasty (TKA) is meant to co-align the prosthetic components to the mechanical axes of the femur and tibia and restore neutral overall limb alignment [2]. In recent decades, it has been dogmatically suggested that MA leads to the longest implant survival. However, this assumption was recently questioned. With modern implant designs and improved surgical techniques, the failure rates do not correlate with the outliers in terms of range (0° ± 3°), varus (>3°), or valgus (>3°) following TKA [3, 13, 19, 20]. It is well known that using MA in TKA significantly improves function and satisfaction; nevertheless, a high percentage of patients are not satisfied after TKA [7]. Moreover, none of the efforts performed to achieve higher accuracy in component positioning, such as computer-assisted surgery, have resulted in better outcomes [5]. In contrast, several authors report significantly improved outcomes after slightly undercorrecting varus knees after TKA in comparison with neutral alignment or the slight overcorrection of valgus [18, 21, 23]. It was previously demonstrated that the limb alignment of the average population is not neutral [2, 9, 10]. Therefore, MA may compromise the outcomes after TKA due to changes in joint-line obliquity.
The principle of using kinematic alignment (KA) in TKA is to co-align the flexion–extension (F/E) axis of the femoral component to the natural kinematic axes of the patient’s individual knee. As the primary F/E axis is defined as the geometric centre of a cylinder aligned to the (premorbid) distal and dorsal femur condyles, the technique is meant to restore the natural surface of the distal and dorsal femur. Therewith, 4 of the 6 degrees of freedom to position the femoral component are set: varus–valgus alignment, distal–proximal position, rotation, and anterior–posterior position. The mediolateral position is determined as the centre of the distal femoral condyles and has little influence on the knee kinematics. The femoral flexion is used to adapt the size of the femoral component for an optimal fit and is orientated on the natural distal femoral flexion. The tibial component is then co-aligned parallel to the femur in the varus–valgus plane, so that the tibia rotation axis remains in the same perpendicular dependency to the primary F/E axis as in the natural knee. The slope of the tibial joint line is restored to that of the normal knee [4, 12]. In theory, no ligament releases are necessary because the natural orientation and tension of the soft tissue envelope are reconstructed.
Patient-specific custom-made cutting guides (PSI) were used to realize the philosophy of KA. The technique is based on magnetic resonance imaging scans of the knee, which can visualize osteoarthritic changes. The knee is shown on the MRI scan such that the plane of the oblique sagittal image is perpendicular to the primary axis of the femur, about which the tibia flexes and extends [8]. Proprietary software of the manufacturer of the PSI is used to remodel the knee into its preosteoarthritic state, create a 3-dimensional model of the joint, and identify the kinematic axes of the knee in order to restore the natural joint line and alignment of the preosteoarthritic limb. The cutting guides are shaped to fit the femur and tibia. The cuts are placed in a kinematically aligned manner, so that the knee is returned to its anatomic state before osteoarthritis. This natural alignment is supposed to avoid ligament release and balancing.
The aim of this study is to evaluate the potential benefits of this by using a prospective, randomized design to compare KA and MA cohorts, as to date, only very limited clinical evidence is available. Our null hypothesis is that there would be no clinical differences between the KA and MA cohorts.
Materials and methods
Between 2012 and 2013, 200 patients underwent TKA and were randomly assigned to 2 groups. Two different consultant teams performed the surgeries (only KA or MA), acquired the patients, and assigned them to a single group. In total, 100 TKAs were performed using custom-made cutting guides in order to implant cruciate-retaining TKA (Triathlon System, Stryker, Mahwah, NJ, USA) with KA (ShapeMatch Technology, Otismed Stryker). KA was determined using a proprietary protocol as outlined above and approved by the surgeon prior to surgery. The desired overall post-operative limb alignment, as well as the mechanical medial proximal tibial angle (mMPTA) and mechanical lateral distal femur angle (mLDFA), was determined. The other 100 patients underwent manual cruciate-retaining TKA (Triathlon System). The indications for TKA included progression in osteoarthritic changes, loss of function, and disabling knee pain. Patients were included in this study when (1) the preoperative varus–valgus deformity was ≤10°; (2) mLDFA was 86°–94°; and (3) mMPTA was 86°–94°. The exclusion criteria included (1) body mass index (BMI) >40, (2) history of infection in the knee, (3) post-traumatic osteoarthritis, (4) bony osteotomy, (5) chronic polyarthritis, and underlying (6) neurological disease with mobility impairment.
The following general patient data and scores were preoperatively determined: demographic data [sex, age, height/weight (in order to determine BMI)], and outcomes were assessed using the combined Knee Society Score (KSS) (0–200 indicates worst to best) [15]. Patients were also asked to provide a self-assessment of their limitations through the knee joint using the Western Ontario and McMaster Universities Arthritis Index (WOMAC) (0–96 indicates best to worst) [1]. Radiological evaluations were performed by one senior consultant and one resident, recording the preoperative and post-operative mMPTA, mLDFA, tibial slope, overall limb alignment, and flexion of the femoral component on long-leg standing radiographs and long sagittal films, which were obtained at 12 months after the surgery. In the KA group, the extent of post-operative limb alignment and deviation from the initial plan was evaluated additionally. In the MA group, the indication for TKA was primary osteoarthritis in 100 of 100 cases. In total, 57 women and 43 men with a mean age ± SD of 70 ± 8 years and a mean BMI ± SD of 30 ± 5 were included in this group. In the KA group, the indication for TKA was primary osteoarthritis in 100 of 100 cases. In total, 61 women and 39 men with a mean age ± SD of 67 ± 8 years and a mean BMI ± SD of 30 ± 4 were included in this group.
All patients directly received post-operative multimodal pain therapy, physical management, and continuous passive motion. Additionally, all patients received manual lymph drainage and were mobilized under full weight bearing using 2 crutches. After their hospital stays, 189 of 200 patients went to a rehabilitation unit, and the rest decided to return home with ambulant physiotherapy. All major and minor complications were recorded. Major complications were defined as the need for further operations with implant removal or revision, and minor complications were defined as surgery-related treatments that did not require revision. The KSS and WOMAC scores were recorded on follow-up after 12 months. Post-operative, weight-bearing radiographs were obtained during the patient’s office visits and used to analyse the knee alignment parameters.
Surgical procedure
In the KA group, the guides were designed to fit into the arthritic knee of each patient in only 1 specific position. The posterior cruciate ligament (PCL) was supposed to be preserved. On the femoral side, the distal femoral cut was set by the guide in order to achieve the rotational orientation of the conventional 4-in-1 cutting block. The component size was also determined during preoperative planning. The tibial cut was set by the guide, as well as the position and rotation of the platform. The trial components were inserted to check the range of motion, stability in flexion and extension, patellar tracking, and the functionality of the PCL.
In the MA group, the components were implanted in order to achieve neutral mechanical limb alignment. On the femoral side, an intramedullary alignment system was used to make the distal femoral cut. The rotation of the femoral component was bony referenced to the transepicondylar line and the Whiteside’s line with strict posterior referencing. The tibial component was aligned extramedullary and parallel to the mechanical axis with a 3° posterior slope. Rotation was orientated to the medial third of the tuberosity. The trial components were inserted and followed using the above-described procedure. Ligament balance was evaluated using a soft tissue tensioner (Stryker, Mahwah, NJ, USA), and balancing was performed according to Whiteside’s algorithms if necessary. The ethical board of the Hannover Medical School, Hanover, Germany, approved this study (#1439–2012).
Statistical analysis
The mean, standard deviation, and 95 % confidence intervals were determined for each measurement. The D’Agostino–Pearson test was used to evaluate the normal distribution of the data. The differences in means of the primary outcome parameters were evaluated using the Wilcoxon test for nonparametric data, and the unpaired t test was used to assess normally distributed data. Correlation analysis was performed using the Spearman test. The data analysis was performed using GraphPad Prism software (GraphPad Prism Software Inc., San Diego, CA, USA). The figures were also prepared using GraphPad Prism software. A posteriori power analysis was performed using the clinical-trials.de website. Assuming an alpha of 0.05, a pooled standard deviation for post-operative combined KSS, and with our sample sizes, this study had a statistical power of 0.99 to detect significant differences.
Results
Outcome evaluation of all knees was possible after 12 months in the KA group. In the KA group, 1 patient was intraoperatively converted to a posterior stabilized prosthesis due to the accidental resection of the PCL while the tibial cut was being performed. Intraoperatively, no ligament balancing was performed at all on the KA patients. In all MA patients, the cruciate-retaining (CR) components were used and soft tissue balancing was performed if necessary. In the KA group, 2 patients developed major complications and were revised due to severe multidirectional instability within the first year. In the MA group, 1 patient had to be revised due to instability within the first year and 1 patient was lost to follow-up after 12 months.
The detailed post-operative radiological outcomes are shown in Table 1. While the conventional MA group demonstrated good alignment with the targeted mechanical axis (1° ± 1° varus), the KA group demonstrated an average post-operative alignment of 1° ± 3° valgus. This means that the post-operative deviation from the initial plan, in terms of the overall limb alignment, was 2° ± 2° in the KA group.
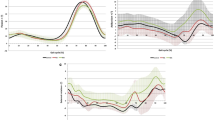
In the KA group, the combined KSS increased from 113 ± 54 points preoperatively to 190 ± 18 at 12 months post-operation. In the MA group, the combined KSS increased from 109 ± 41 points preoperatively to 178 ± 17 at 12 months post-operation (Fig. 1). This represents a statistically significant better KSS in the KA group (p = 0.02).
In the KA group, the WOMAC score decreased from 60 ± 19 points preoperatively to 13 ± 16 points at 12 months post-operation. In the MA group, the WOMAC score decreased from 62 ± 12 points preoperatively to 26 ± 11 points at 12 months post-operation. This difference is statistically significant (p = 0.001). The frequency distribution of the WOMAC scores shows that the majority of the patients in the KA group demonstrated ≤20 points; however, 6 patients demonstrated >40 points (Fig. 2). In the MA group, a broader distribution was noted for the majority of patients, and no such outliers were detected.
Correlation analysis indicated a significant and negative correlation between the deviation of the post-operative alignment from the initial preoperative KA plan and poor KSS in the KA group (r = −0.22; p = 0.02; Fig. 3). Regarding the WOMAC scores, correlation analysis indicated a correlation between a high flexed femoral component and a high WOMAC score in the KA group (r = 0.34; p = 0.005).
Discussion
The most important finding of this study is that using PSI KA in TKA achieves comparable results to non-PSI MA in TKA. This study shows that restoring the premorbid flexion–extension axis of the knee joint may lead to better functional results. Comparable clinical outcomes for KA were recently published by other groups [8, 13]. The primary hypothesis has to be rejected. A higher portion of knees with excellent function and subjectively excellent results were found in the KA group.
Although significantly better results in the KA group were noted, the distribution of the results is quite broad in comparison with the MA group and several treatment failures were noted (i.e. poor outcome scores). Regarding the WOMAC scores, 6 patients demonstrated >40 points in the KA group in comparison with only 1 patient with >40 points in the MA group. Regarding KSS, 5 patients demonstrated <150 points in the KA group in comparison with only 1 patient in the MA group. This might be due to malalignment or plan deviation issues, respectively. A particular example is shown in Fig. 4. This patient had a preoperative overall limb alignment of 1° valgus that was brought into about 8° valgus, although the patient was planned for 1° valgus. This patient had to be revised after 4 months due to the instability of highly constrained components. Other studies that used the same PSI system for KA did not report their plan deviations [8, 13, 14]. The large variations in plan deviations found in this study are contrary to other PSI techniques designed for the mechanical axis [11, 16, 25]. However, it remains unclear whether these deviations are due to surgical or design errors of the PSI. Because the specific KA of PSI (Stryker ShapeMatch Technology) is currently unavailable, there is no possibility of further investigating the accuracy of the planning algorithm or the PSI technology itself. In the future, it would be very interesting to determine whether the same problems develop when using the manual surgical technique to achieve KA, as described earlier as an alternative technique.
Since no correlation was seen between special preoperative deformities, designated plans, and post-operative outcomes, there is currently no evidence about which particular deviations might not be suitable for KA alignment. However, only mild deformities were treated, due to the inclusion criteria of this study.
The correlation between a high WOMAC score and high flexed femoral components was evaluated. This is comparable to recently published results. Kashmiri et al. reported that an increase in femoral component flexion leads to a decrease in the epicondylar distance and a more posterior patella in relation to the femur. This distance provides information about the anteroposterior position of the patella throughout the flexion cycle in relation to the femur. Furthermore, Keshmiri et al. report that an increase in femoral component flexion increases post-operative patellar lateral shift. Their generalized linear model indicated that at 90° flexion, a 1° change in femoral component flexion (preoperative to post-operative) results in an approximately +0.5 mm mediolateral patellar shift [17]. This might explain our findings to a certain degree, and femoral flexion must be considered when using KA in TKA. Yan et al. reported before that the use of PSI blocks might result in excessively flexed femoral components [24].
The outcome scores evaluated in this trial are comparable to other studies that also compare KA and MA [8] or focus on KA alone [12–14]. It is questionable that our good results are due to the use of PSI since its usage is not proven to be superior to manual TKA [6]. Moreover, the PSI guides used in this study might be responsible for our outliers, as this technique leaves space for intraoperative errors. In particular, there is no option for controlling alignment in the coronal plane or correcting the tibial slope (e.g. laceration of the PCL). Controlling femoral flexion in the sagittal plane is not possible either.
Several limitations should be addressed. Due to high overall costs, patient blinding was not performed in this study. Our radiological measurements were obtained using digital long-leg standing X-rays. It is well known that this kind of evaluation is not precise [22]. Due to radiation protection reasons, we were not allowed to do CT scans. Even the post-operative deviation in alignment from the initial preoperative KA plan is within the range of the potential inaccuracies of this method. Furthermore, only the results of a short follow-up period are reported, and the long-term effects of KA on implant longevity were not assessed.
Howell et al. recently reported accurate alignment, high function, and high subjective patient satisfaction in a cohort that underwent manually operated KA [14]. In concordance with our data, the idea of KA might be implemented in surgeons’ preoperative TKA planning.
Conclusion
The principle of KA might be the reason for the better outcomes reported in this study. In conclusion, KA might be an alternative technique for use in TKA. However, devastating errors may occur when performed in combination with the presented PSI technique.
References
Bellamy N, Buchanan WW (1986) A preliminary evaluation of the dimensionality and clinical importance of pain and disability in osteoarthritis of the hip and knee. Clin Rheumatol 5(2):231–241
Bellemans J, Colyn W, Vandenneucker H, Victor J (2012) The Chitranjan Ranawat award: is neutral mechanical alignment normal for all patients? The concept of constitutional varus. Clin Orthop Relat Res 470(1):45–53
Bonner TJ, Eardley WG, Patterson P, Gregg PJ (2011) The effect of post-operative mechanical axis alignment on the survival of primary total knee replacements after a follow-up of 15 years. J Bone Joint Surg Br 93(9):1217–1222
Calliess T, Ettinger M, Stukenborg-Colsmann C, Windhagen H (2015) Kinematic alignment in total knee arthroplasty: concept, evidence base and limitations. Orthopade 44(4):282–286
Calliess T, Ettinger M, Windhagen H (2014) Computer-assisted systems in total knee arthroplasty. Useful aid or only additional costs. Orthopade 43(6):529–533
Camarda L, D’Arienzo A, Morello S, Peri G, Valentino B, D’Arienzo M (2015) Patient-specific instrumentation for total knee arthroplasty: a literature review. Musculoskelet Surg 99(1):11–18
Carr AJ, Robertsson O, Graves S, Price AJ, Arden NK, Judge A, Beard DJ (2012) Knee replacement. Lancet 379(9823):1331–1340
Dossett HG, Estrada NA, Swartz GJ, LeFevre GW, Kwasman BG (2014) A randomised controlled trial of kinematically and mechanically aligned total knee replacements: two-year clinical results. Bone Joint J 96-B(7):907–913
Eckhoff DG, Bach JM, Spitzer VM, Reinig KD, Bagur MM, Baldini TH, Flannery NM (2005) Three-dimensional mechanics, kinematics, and morphology of the knee viewed in virtual reality. J Bone Joint Surg Am 87(Suppl 2):71–80
Eckhoff DG, Bach JM, Spitzer VM, Reinig KD, Bagur MM, Baldini TH, Rubinstein D, Humphries S (2003) Three-dimensional morphology and kinematics of the distal part of the femur viewed in virtual reality. Part II. J Bone Joint Surg Am 85-A(Suppl 4):97–104
Hamilton WG, Parks NL, Saxena A (2013) Patient-specific instrumentation does not shorten surgical time: a prospective, randomized trial. J Arthroplast 28(8 Suppl):96–100
Howell SM, Howell SJ, Kuznik KT, Cohen J, Hull ML (2013) Does a kinematically aligned total knee arthroplasty restore function without failure regardless of alignment category? Clin Orthop Relat Res 471(3):1000–1007
Howell SM, Papadopoulos S, Kuznik K, Ghaly LR, Hull ML (2015) Does varus alignment adversely affect implant survival and function six years after kinematically aligned total knee arthroplasty? Int Orthop. doi:10.1007/s00264-015-2743-5
Howell SM, Papadopoulos S, Kuznik KT, Hull ML (2013) Accurate alignment and high function after kinematically aligned TKA performed with generic instruments. Knee Surg Sports Traumatol Arthrosc 21(10):2271–2280
Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res 248:13–14
Jiang J, Kang X, Lin Q, Teng Y, An L, Ma J, Wang J, Xia Y (2015) Accuracy of patient-specific instrumentation compared with conventional instrumentation in total knee arthroplasty. Orthopedics 38(4):e305–e313
Keshmiri A, Maderbacher G, Baier C, Sendtner E, Schaumburger J, Zeman F, Grifka J, Springorum HR (2015) The influence of component alignment on patellar kinematics in total knee arthroplasty. Acta Orthop 86(4):444–500
Luyckx T, Vanhoorebeeck F, Bellemans J (2015) Should we aim at undercorrection when doing a total knee arthroplasty? Knee Surg Sports Traumatol Arthrosc 23(6):1706–1712
Magnussen RA, Weppe F, Demey G, Servien E, Lustig S (2011) Residual varus alignment does not compromise results of TKAs in patients with preoperative varus. Clin Orthop Relat Res 469(12):3443–3450
Matziolis G, Adam J, Perka C (2010) Varus malalignment has no influence on clinical outcome in midterm follow-up after total knee replacement. Arch Orthop Trauma Surg 130(12):1487–1491
Parratte S, Pagnano MW, Trousdale RT, Berry DJ (2010) Effect of postoperative mechanical axis alignment on the fifteen-year survival of modern, cemented total knee replacements. J Bone Joint Surg Am 92(12):2143–2149
Radtke K, Becher C, Noll Y, Ostermeier S (2010) Effect of limb rotation on radiographic alignment in total knee arthroplasties. Arch Orthop Trauma Surg 130(4):451–457
Vanlommel L, Vanlommel J, Claes S, Bellemans J (2013) Slight undercorrection following total knee arthroplasty results in superior clinical outcomes in varus knees. Knee Surg Sports Traumatol Arthrosc 21(10):2325–2330
Yan CH, Chiu KY, Ng FY, Chan PK, Fang CX (2015) Comparison between patient-specific instruments and conventional instruments and computer navigation in total knee arthroplasty: a randomized controlled trial. Knee Surg Sports Traumatol Arthrosc 23(12):3637–3645
Zhu M, Chen JY, Chong HC, Yew AK, Foo LS, Chia SL, Lo NN, Yeo SJ (2015) Outcomes following total knee arthroplasty with CT-based patient-specific instrumentation. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-015-3803-5
Acknowledgments
TC, CSC, HW, and ME are consultants for Stryker. This project was supported by the AXIS Foundation for Orthopedic research, Hamburg, Germany.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Calliess, T., Bauer, K., Stukenborg-Colsman, C. et al. PSI kinematic versus non-PSI mechanical alignment in total knee arthroplasty: a prospective, randomized study. Knee Surg Sports Traumatol Arthrosc 25, 1743–1748 (2017). https://doi.org/10.1007/s00167-016-4136-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-016-4136-8