Abstract
Purpose
Anterior cruciate ligament (ACL) surgery in the paediatric population has long been a challenge. Non-operative treatment will result in persistent instability which can lead to chondral and meniscal injuries. The results of primary open ACL repair are poor. Concerns of growth plate disturbance with transphyseal techniques and issues with relatively small-diameter grafts in Tanner 1 and 2 patients, which are inadequate, have contributed to these challenges. With advancing instrumentation, there is renewed interest in ACL repair. The minimally invasive approach of arthroscopic primary ACL repair retains the native ligament. The objective and subjective outcomes at 2 years are presented.
Methods
Paediatric patients, less than 16 years of age, presenting acutely with complete proximal ACL ruptures underwent direct arthroscopic ACL repair, reinforced by a temporary internal brace, which was subsequently removed after 3 months. Patient-reported outcome measures including the Lysholm, Tegner and KOOS scores were collected at 6 months, 1 year and 2 years post-operatively.
Results
Twenty patients (age 6–16) completed data at 2 years post-operatively. There were no failures, no complications and no growth disturbance out to 2 years. The 2-year postoperative outcomes; Lysholm 95 (90–100), Tegner 7 (6–10), KOOS-Child 96.5 (88.9–100) demonstrated statistically significant improvements following surgery (p < 0.001). Objective measurements with an accelerometer did not demonstrate any significant side-to-side difference.
Conclusion
ACL repair for proximal ACL tears in the paediatric population demonstrates the potential for excellent outcomes at short-term follow-up. This presents an attractive alternative to ACL reconstruction when an adequate ACL remnant permits direct repair. Our results demonstrate that paediatric ACL repair is safe and effective.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Paediatric anterior cruciate ligament (ACL) ruptures have traditionally been perceived as uncommon. With advancements in diagnostic imaging, increased clinical awareness, and more demanding childhood athletics, the incidence of ACL tears in the skeletally immature population has increased [3, 5]. Non-operative management of ACL injuries in children and adolescents, until skeletal maturity, will ubiquitously lead to persistent instability, functional decline and subsequent meniscal and chondral injury.
Surgical management of ACL tears in children and adolescents pose unique management challenges. The presence of open physes, particularly the undulating distal femoral physis, must be taken into consideration. Further, predicted growth remaining must be assessed to determine if a physeal sparing or physeal respecting procedure can be performed. These considerations have led to multiple surgical techniques to reconstruct ACL tears that minimise the risk of growth disturbance, while maximising patient outcomes [16, 21, 32]. Despite this work, no gold standard treatment algorithm or agreed upon graft choice has emerged.
Advancing arthroscopic techniques and instrumentation have led to a resurgence in interest in primary ACL repair. Primary arthroscopic ACL repair with modern techniques and implants has excellent clinical outcomes and these results are maintained at the mid-term follow-up [6]. There are practical advantages to this approach including reduced surgical morbidity and time to recovery [37]. Theoretical advantages include the restoration/preservation of normal knee proprioception and biomechanics [8] that may be due to the preservation of the native ACL and the ability to restore the ACL to the native femoral footprint.
Augmentation is thought to mitigate pathologic strain on a ligament repair that can optimise healing, while allowing for appropriate, early rehabilitation [38]. The purpose of this study is to report on early clinical outcomes after arthroscopic primary ACL repair with internal bracing in a cohort of skeletally immature patients, while providing an update to our original surgical technique. The purpose of this study was to evaluate if this minimally invasive arthroscopic primary ACL repair, which retains the native ligament, would result in low rates of re-rupture and failure yielding good clinical outcomes in the paediatric cohort.
Materials and methods
The study was approved by the institutional review board of Basingstoke and North Hampshire Hospital (ORTHOEVA10). All subjects gave their written informed consent to participate in this investigation. HRA and NEC ethical committee approval was not required for this study.
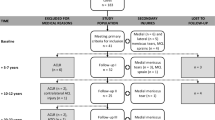
A prospectively maintained database was retrospectively reviewed to identify all paediatric ACL repairs performed between January 2014 and May 2017. Patient demographics were collected to include age, sex, BMI and side of injured limb. Inclusion criteria included skeletally immature patients undergoing primary repair for a Sherman 1 or 2 proximal femoral avulsion ACL tear with excellent ACL tissue quality defined by having a broad stump with mild interstitial tearing, with the ability to hold the fixation sutures [31]. Exclusion criteria included patients without pre-operative data, skeletal maturity, those who had a mid-substance tear or patients with an injury spectrum outside an isolated ACL rupture. Patients who underwent an ACL repair with the addition of another ligament reconstruction, e.g., anterolateral ligament reconstruction were not included in the study. An inadequate ACL stump remnant, i.e., inadequate tissue quantity or quality, on direct visualisation and probing does also preclude repair.
Primary subjective outcomes, validated for paediatric patients, were patient-reported outcome measures (PROMs), which included the Lysholm, Tegner and KOOS-child scores. These were collected pre-operatively, 1 year and 2 years post-operatively. Primary objective measurements were scored using the KiRa triaxial accelerometer which quantitatively assessed the Lachman’s and Pivot shift [1, 17, 27, 36]. Each of these tests was performed three times on the affected knee and the contralateral unaffected knee. The average of the three values was taken and the difference between the two limbs was calculated. Before testing, the KiRA device was attached to the lateral aspect of the tibia non-invasively on the skin with a hypo-allergic brace between the tibial tuberosity and Gerdy’s tubercle by a belt. This system was wirelessly connected to a tablet with Bluetooth where knee motion analysis was conducted. This tool measures the acceleration of the tibia relative to the femur for the pivot shift phenomenon (m/s2) and Lachman (mm) to determine the magnitude of each motion. The KiRA dynamic accelerometer was performed at final follow-up. Secondary outcomes included re-rupture, revision and growth arrest/disturbance rates.
Skeletal maturity was assessed via the presence or absence of open physes on radiographs and magnetic resonance imaging (MRI) and the Tanner–Whitehouse method [35]. This involved questions put forward in the clinic regarding the development of secondary sexual characteristics which were confirmed in the operating theatre under general anaesthetic. Coronal plane alignment was assessed clinically and radiologically with a long leg standing alignment radiograph in all patients at preoperative status and at 1 year postoperatively. Thereafter, radiological assessment was only undertaken if indicated by a change in clinical examination to limit radiation exposure. A transphyseal ACL internal brace technique (described below) was used in all cases. All patients were operated on by the senior author.
Surgical technique
ACL repair was considered in all skeletally immature patients. A transphyseal approach with small-diameter tunnels was adopted in all cases within this cohort.
Examination of the ACL was performed. If the tear was found to be a proximal avulsion or proximal rupture, Sherman types 1 and 2, respectively, repair of the native ligament was performed [31]. Proximal third and mid-substance tears, Sherman types 3 and 4, were not suitable for repair. The tissue quality is examined to ensure the stump is of sound structural integrity and can be satisfactorily approximated to the sidewall without gapping at the proximal end. The final decision was based on arthroscopy.
A passport cannula is passed through the anteromedial (AM) portal for suture management. Two high tensile braided composite looped sutures are passed around the proximal ACL stump, as a luggage tag-type stitch, with an arthroscopic suture passing instrument to approximate the remnant to the sidewall of the femoral condyle. The luggage lag stitch is passed through the midsubstance of the ACL remnant.
For Tanner stage 2–4 patients, a 4-mm spade tip beath pin with an eyelet is passed in a transphyseal fashion to create a femoral tunnel in the centre of the existing ACL footprint. For Tanner stage 1 patients, a 2.4-mm wire is passed and the tunnel is dilated up with a 3.5-mm drill. The spade tip is then loaded with a passing suture and the looped/folded end is retained through the passport cannula; while the free ends, through the eyelet, are passed through the femoral tunnel. This single loop is then divided to form two individual limbs, or shuttling sutures, which are present out of the AM portal and a simple knot is tied in the free end creating a “snare” at the end of each limb. The first shuttling suture is used to feed the two repair sutures, around the proximal ACL stump, into the femoral tunnel and at a later stage, the second snare is used to pull up the internal brace. By applying continuous tension on the repair sutures externally on the femoral side, the tension can be assessed and optimised and the sutures can be manipulated on the ACL to a favourable position to allow approximation of the ACL stump to the side wall.
A tibial tunnel ACL reconstruction aiming guide is then placed into the centre of the ACL footprint on the tibial side and a 2.4-mm wire is passed followed by a 3.5-mm reamer for Tanner stage 1 patients via a transphyseal technique. For Tanner stage 2–4 patients, this tunnel is expanded with a 4.5-mm drill. The reversed end of the 2.4 mm spade tip wire with the open eyelet is passed retrograde (the eyelet end is passed) up the tibial tunnel with a passing suture loaded through the eyelet. This passing suture is retrieved through the AM portal and the spade tip beath pin is removed. The second shuttling suture (in situ through the femoral tunnel and out of the AM portal) is then tied to the tibial passing suture. The tibial passing suture is then retrieved through the tibial tunnel. The resulting shuttling suture now passes through the both the tibial and femoral tunnels and through the centre of ACL fibres.
The augmentation device used is created with a metal cortical suspension button and non-biodegradable suture tape.
The passing suture is used to pass the augmentation device through the tibial tunnel, knee joint and femoral tunnel under a combination of direct and arthroscopic visualisation. The button is secured against the femoral cortex. This can be directly viewed with the arthroscope [33]. The ACL repair sutures are then sequentially tied onto each limb of the suture tape that is loaded through the button. Tension on the ACL repair sutures must be maintained during this step. The free tails are then fed through a bone anchor and secured onto the anteromedial surface of tibia, distal to the physis at 20° of knee flexion and neutral rotation.
Early full weight bearing was permitted with a full range of movement. Unloaded active extension and closed chain activities including use of a stationary bike were targeted in the early rehabilitation period.
The augmentation device was routinely released in a second procedure 3 months after the index surgery to avoid any possible growth disturbance and this release was performed by dividing it at its tibial end only. No intra-articular work was performed. During release, an EUA and second look arthroscopy of the ACL was performed.
Statistical analysis
Data were analysed using SPSS v.22 (IBM, New York, USA) and Excel 2010 (Microsoft, Washington, USA). Data were assessed for normality using the Shapiro–Wilks test and by visually analysing histograms. All data across all cohorts were not normally distributed. Descriptive statistics was calculated before a total of three Friedman tests were conducted, one for each type of questionnaire. A Bonferroni correction was performed to lower the likelihood of a Type I error. An adjusted α level was set at 0.017. Post hoc Wilcoxon signed rank pairwise comparisons with Bonferroni corrections were also obtained.
Results
A total of 20 paediatric ACL repairs were performed and completed pre- and post-operative outcome data which met the inclusion criteria. See Table 1 for demographic data.
Serial radiographs including long leg imaging were reviewed for the patient cohort and there were no physeal injuries leading to deformity or leg length discrepancy.
The outcome scores for the Lysholm, Tegner and KOOS-child activity scales were recorded. The median pre-operative, 1-year and 2-year post-operative scores are shown in Table 2. All PROMs showed a statistically significant improvement at all time points. The KiRA data demonstrated no significant side-to-side difference with regards to pivoting and a successful reduction in anterior translation to within 3 mm of the contralateral uninjured side. The average Lachman side-to-side difference was 1.2 mm. The average Pivot shift side-to-side difference was 0.3 m/s2.
At 3 months, a second look arthroscopy was undertaken and the internal brace released in all 20 patients. During the arthroscopy, the internal brace was only just visible in four cases (26%). The ACL repair was noted to be healed upon arthroscopic visualisation and probing in all 20 patients.
There have been no re-ruptures or revision reconstructions in this cohort study.
Discussion
The most important finding of the present study is that excellent short-term outcomes can be expected in paediatric patients with Sherman 1 and 2 proximal ACL tears managed with direct ACL repair. No revisions or re-ruptures were recorded in the final cohort at final follow-up. It is clear from the encouraging early results that repair may play an important role in paediatric ACL rupture management.
The resurgence of interest in primary ACL repair represents an exciting step forward in the treatment of this common and potentially debilitating injury.
Patients who are skeletally immature are thought to have a generally improved ability to heal from injury and/or surgery than their skeletally mature counterparts. Murray’s results support the improved capacity of functional healing of a ligament after injury and enhanced repair is dependent on the level of skeletal maturity. Murray et al. has improved our understanding on how the intra-articular environment affects the healing capacity of certain ACL tears [23,24,25,26, 39,40,41].
There are several technical advantages of this technique over other proposed procedures. There is no graft harvest, which is advantageous as it avoids donor site morbidity. Concerns of inadequate graft dimensions are also not a concern [18, 20, 34]. Despite a transphyseal technique, the femoral and tibial tunnel diameters are much smaller than a conventional ACL reconstruction. Animal studies have shown for transphyseal ACL reconstruction, the prevalence of physeal arrest increases when physeal damage involves more than 7% of the total physeal volume [19]. Evidence from an MRI-based study suggests that less than 3% of the total physeal volume was damaged when an 8-mm tunnel was drilled across the physis [15]. These small tunnels are technically advantageous because they obviate the need for intra-operative fluoroscopic all-epiphyseal femoral and/or tibial tunnel creation and there is little to no concern about the obliquity of the tunnel across either physis [4, 30]. With that said, we prefer to violate the physes in a central position as possible [9, 11]. We have not experienced any growth disturbance to date. All paediatric patients undergoing ACL repair have annual clinical follow-up with serial long leg radiographs as indicated to ensure deformity does not develop.
Despite the above advantages, it should be noted that there is a steep learning curve in performing this procedure. Paediatric ACL repairs should be performed in centres with surgeons who have a specialist interest and training in the management of paediatric knee injuries with the capacity for regular monitoring post-operatively.
Even with advances in surgical techniques to avoid open physes, there are factors which are out of the surgeon’s control. The four-strand hamstring graft is the most common autograft used and improved clinical outcome is directly dependent on the diameter of the hamstring graft. Magnussen et al. evaluated hamstring autograft diameter as a predictor for graft failure and its need for revision. Grafts of less than 7-mm diameter had an overall revision rate of 33% [18].
Augmentation via internal bracing of ligament repairs about the musculoskeletal system is a new and interesting concept that has led to favourable early clinical results [2, 7, 22, 28]. Heusdens et al. [12] and Jonkergouw et al. [14] have published their series of acute ACL repairs and short-term outcomes demonstrating favourable subjective and objective scoring with low re-rupture rates, predominantly in an adult population. Hoogeslag et al. [13] reported a prospective randomised controlled trial comparing the outcomes of ACL repair with ACL reconstruction and found that dynamic augmented ACL suture repair, utilising the Ligamys system, was not inferior to the ACL reconstruction group in terms of subjective PROMs. There was a higher, non-significant, number of adverse events leading to repeat surgery. This was for reasons other than revision ACL surgery for re-rupture. This dynamic system is a different philosophy to the system adopted in this series and caution should be used when creating a 10-mm diameter outside-in tibial socket to accommodate the monobloc tibial fixation device in a skeletally immature patient. The mean age for the repair group was 21 years.
Gagliardi et al. [10] reported the results of a comparative single surgeon series which followed a cohort of adolescent patients who underwent ACL repair and to compare the outcomes with those who underwent ACL reconstruction. They found the cumulative incidence of graft failure in the first 3 years after ACL repair was 48.8% and the hazard to failure in the repair group was 10.6 times that of the reconstruction group. However, the major difference is the surgical technique adopted. A double-bundle repair technique with two independent femoral drill tunnels and one or two independent tibial tunnels were created which undoubtedly would sacrifice the native ACL fibres and footprints. Four millimetre drill tunnels were created; therefore, the cumulative damage to the underlying footprint would be a concern. An all-epiphyseal technique was used for skeletally immature patients. The outcomes were questionnaire based and dynamic examination with the KT-1000 was only performed in 9% of the repair cohort.
From a physeal tethering perspective, the amount of force needed for physeal arrest is 530 N [29] and the ultimate load to failure of the internal brace is approximately 300 N. Although the brace should fail prior to the occurrence of growth disturbance, prophylactic removal of the internal brace, to keep any potential growth disturbance risk at a minimum, was performed.
There are several limitations to the study. Despite its prospective nature, this is currently a short-term follow-up study; however, long-term longevity of the repair with monitoring of growth disturbance continues. Further, almost 50% of the cohort did not have pre-operative outcome data and, therefore, were excluded resulting in the small sample size.
The clinical relevance of this study has shown direct ACL repair in the paediatric population is a surgical safe option which can be performed to prevent recurrent instability and chondromeniscal injury.
Conclusion
In conclusion, this surgical technique avoids potential pitfalls commonly seen with paediatric ACL reconstruction and has very reliable healing at short-term follow-up. No growth disturbance, leg length discrepancy or growth arrest was encountered in this series. High return to athletic and pre-injury activity level was recorded.
Change history
18 May 2020
Authors would like to update the full author names
References
Berruto M, Uboldi F, Gala L, Marelli B, Albisetti W (2013) Is triaxial accelerometer reliable in the evaluation and grading of knee pivot-shift phenomenon? Knee Surg Sports Traumatol Arthrosc 21(4):981–985
Byrne PA, Hopper GP, Wilson WT, Mackay GM (2018) Acromioclavicular joint stabilisation using the internal brace principle. Surg Technol Int 20(33):294–298
Christino MA, Tepolt FA, Sugimoto D, Micheli LJ, Kocher MS (2018) Revision ACL reconstruction in children and adolescents. J Pediatr Orthop. https://doi.org/10.1097/BPO.0000000000001155
Cruz AI Jr, Lakomkin N, Fabricant PD, Lawrence JT (2016) Transphyseal ACL reconstruction in skeletally immature patients does independent femoral tunnel drilling place the physis at greater risk compared with transtibial drilling? Orthop J Sports Med 4(6):2325967116650432
DeFrancesco CJ, Storey EP, Shea KG, Kocher MS, Ganley TJ (2018) Challenges in the management of anterior cruciate ligament ruptures in skeletally immature patients. J Am Acad Orthop Surg 26(3):e50–e61
DiFelice GS, van der List JP (2018) Clinical outcomes of arthroscopic primary repair of proximal anterior cruciate ligament tears are maintained at mid-term follow-up. Arthroscopy 34(4):1085–1093
DiFelice GS, Villegas C, Taylor S (2015) Anterior cruciate ligament preservation: early results of a novel arthroscopic technique for suture anchor primary anterior cruciate ligament repair. Arthroscopy 31(11):2162–2171
Fleming BC, Carey JL, Spindler KP, Murray MM (2008) Can suture repair of ACL transection restore normal anteroposterior laxity of the knee? An ex vivo study. J Orthop Res 26:1500–1505
Frosch KH, Stengel D, Brodhun T, Stietencron I, Holsten D, Jung C, Reister D, Voigt C, Niemeyer P, Maier M, Hertel P, Jagodzinski M, Lill H (2010) Outcomes and risks of operative treatment of rupture of the anterior cruciate ligament in children and adolescents. Arthroscopy 26(11):1539–1550
Gagliardi AG, Carry PM, Parikh HB, Traver JL, Howell DR, Albright JC (2019) ACL repair with suture ligament augmentation is associated with a high failure rate among adolescent patients. Am J Sports Med 47(3):560–566
Hamrin SE, Svantesson E, Spindler KP, Alentorn-Geli E, Sundemo D, Westin O, Karlsson J, Samuelsson K (2018) Ten-year risk factors for inferior knee injury and osteoarthritis outcome score after anterior cruciate ligament reconstruction: A Study of 874 Patients From the Swedish National Knee Ligament Register. Am J Sports Med 46(12):2851–2858
Heusdens CHW, Hopper GP, Dossche L, Roelant E, Mackay GM (2019) Anterior cruciate ligament repair with Independent Suture Tape Reinforcement: a case series with 2-year follow-up. Knee Surg Sports Traumatol Arthrosc 27(1):60–67
Hoogeslag RAG, Brouwer RW, Boer BC, de Vries AJ, In’t Veld R. HR (2019) Acute anterior cruciate ligament rupture: repair or reconstruction? Two-year results of a randomized controlled clinical trial. Am J Sports Med 47(3):567–577
Jonkergouw A, van der List JP, DiFelice GS (2019) Arthroscopic primary repair of proximal anterior cruciate ligament tears: outcomes of the first 56 consecutive patients and the role of additional internal bracing. Knee Surg Sports Traumatol Arthrosc 27(1):21–28
Kercher J, Xerogeanes J, Tannenbaum A, Al-Hakim R, Black JC, Zhao J (2009) Anterior cruciate ligament reconstruction in the skeletally immature: an anatomical study utilizing 3-dimensional magnetic resonance imaging reconstructions. J Pediatr Orthop 29(2):124–129
Kim SJ, Shim DW, Park KW (2012) Functional outcome of transphyseal reconstruction of the anterior cruciate ligament in skeletally immature patients. Knee Surg Relat Res 24(3):173–179
Lopomo N, Zaffagnini S, Signorelli C, Bignozzi S, Giordano G, Marcheggiani Muccioli GM, Visani A (2012) An original clinical methodology for non-invasive assessment of pivot-shift test. Comput Methods Biomech Biomed Eng 15(12):1323–1328
Magnussen RA, Lawrence JT, West RL, Toth AP, Taylor DC, Garrett WE (2012) Graft size and patient age are predictors of early revision after anterior cruciate ligament reconstruction with hamstring autograft. Arthroscopy 28:526–531
Mäkelä EA, Vainionpää S, Vihtonen K, Mero M, Rokkanen P (1988) The effect of trauma to the lower femoral epiphyseal plate. An experimental study in rabbits. J Bone Jt Surg Br. 70(2):187–191
Mariscalco MW, Flanigan DC, Mitchell J et al (2013) The influence of hamstring autograft size on patient-reported outcomes and risk of revision after anterior cruciate ligament reconstruction: a Multicenter Orthopaedic Outcomes Network (MOON) Cohort Study. Arthroscopy 29:1948–1953
Mauch C, Arnold MP, Wirries A, Mayer RR, Friederich NF, Hirschmann MT (2011) Anterior cruciate ligament reconstruction using quadriceps tendon autograft for adolescents with open physes—a technical note. Sports Med Arthrosc Rehabil Ther Technol 3:7
McWilliam JR, Mackay G (2016) The internal brace for midsubstance achilles ruptures. Foot Ankle Int 37(7):794–800
Murray MM (2009) Current status and potential of primary ACL repair. Clin Sports Med. 28(1):51–61
Murray MM, Fleming BC (2013) Biology of anterior cruciate ligament injury and repair: Kappa delta ann doner vaughn award paper 2013. J Orthop Res 31(10):1501–1506
Murray MM, Flutie BM, Kalish LA, Ecklund K, Fleming BC, Proffen BL, Micheli LJ (2016) The Bridge-Enhanced Anterior Cruciate Ligament Repair (BEAR) procedure: an early feasibility cohort study. Orthop J Sports Med. 4(11):2325967116672176
Murray MM, Magarian EM, Harrison SL, Mastrangelo AN, Zurakowski D, Fleming BC (2010) The effect of skeletal maturity on functional healing of the anterior cruciate ligament. J Bone Jt Surg Am 92(11):2039–2049
Nakamura K, Koga H, Sekiya I, Watanabe T, Mochizuki T, Horie M, Nakamura T, Otabe K, Muneta T (2017) Evaluation of pivot shift phenomenon while awake and under anaesthesia by different manoeuvres using triaxial accelerometer. Knee Surg Sports Traumatol Arthrosc 25(8):2377–2383
Regauer M, Mackay G, Lange M, Kammerlander C, Böcker W (2017) Syndesmotic InternalBrace for anatomic distal tibiofibular ligament augmentation. World J Orthop. 8(4):301–309
Shapiro F (2001) ‘Lower extremity length discrepancy’. Elsevier, Boston, Massachusetts, USA
Shea KG, Apel PJ, Pfeiffer RP, Traughber PD (2007) The anatomy of the proximal tibia in pediatric and adolescent patients: implications for ACL reconstruction and prevention of physeal arrest. Knee Surg Sports Traumatol Arthrosc 15(4):320–327
Sherman MF, Lieber L, Bonamo JR, Podesta L, Reiter I (1991) The long-term followup of primary anterior cruciate ligament repair. Defining a rationale for augmentation. Am J Sports Med 19(3):243–255
Smith JO, Yasen SK, Palmer HC, Lord BR, Britton EM, Wilson AJ (2016) Paediatric ACL repair reinforced with temporary internal bracing. Knee Surg Sports Traumatol Arthrosc 24(6):1845–1851
Sonnery-Cottet B, Rezende FC, Martins Neto A, Fayard JM, Thaunat M, Kader DF (2014) Arthroscopically confirmed femoral button deployment. Arthrosc Tech 3(3):309–312
Spragg L, Chen J, Mirzayan R, Love R, Maletis G (2016) The effect of autologous hamstring graft diameter on the likelihood for revision of anterior cruciate ligament reconstruction. Am J Sports Med 44:1475–1481
Tanner JM, Whitehouse RH, Takaishi M (1966) Standards from birth to maturity for height, weight, height velocity, and weight velocity: British children, 1965. I. Arch Dis Child 41(219):454–471
Tanaka T, Hoshino Y, Miyaji N, Ibaragi K, Nishida K, Nishizawa Y, Araki D, Kanzaki N, Matsushita T, Kuroda R (2018) The diagnostic reliability of the quantitative pivot-shift evaluation using an electromagnetic measurement system for anterior cruciate ligament deficiency was superior to those of the accelerometer and iPad image analysis. Knee Surg Sports Traumatol Arthrosc 26(9):2835–2840
van der List JP, Di Felice GS (2017) Range of motion and complications following primary repair versus reconstruction of the anterior cruciate ligament. Knee 24(4):798–807
van Eck CF, Limpisvasti O, ElAttrache NS (2018) Is there a role for internal bracing and repair of the anterior cruciate ligament? A systematic literature review. Am J Sports Med 46(9):2291–2298
Vavken P, Fleming BC, Mastrangelo AN, Machan JT, Murray MM (2012) Biomechanical outcomes after bioenhanced anterior cruciate ligament repair and anterior cruciate ligament reconstruction are equal in a porcine model. Arthroscopy 28(5):672–680
Vavken P, Murray MM (2011) The potential for primary repair of the ACL. Sports Med Arthrosc Rev. 19(1):44–49
Vavken P, Proffen B, Peterson C, Fleming BC, Machan JT, Murray MM (2013) Effects of suture choice on biomechanics and physeal status after bioenhanced anterior cruciate ligament repair in skeletally immature patients: a large-animal study. Arthroscopy 29(1):122–132
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Adrian Wilson is a paid consultant for Arthrex and James Lee Pace is a paid consultant for Arthrex. John Dabis, Sam Yasen and Aaron Foster have no conflicts of interest.
Funding
The authors are grateful to the department of Trauma and Orthopaedics at Basingstoke and North Hampshire Hospital for the funding of the data collection, statistical analysis and manuscript preparation.
Ethical Approval
All patents proved informed consent for their use fo their data for research and publication. The study was approved by the institutional review board of Basingstoke and North Hampshire Hospital (ORTHOEVA10). All subjects gave their written informed consent to participate in this investigation. All procedures performed in this study were in accordance with the ethical standard of the institution and with the 1964 Helsinki declaration and its later amendments.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised: Full version of author names updated in author group.
Rights and permissions
About this article
Cite this article
Dabis, J., Yasen, S.K., Foster, A.J. et al. Paediatric proximal ACL tears managed with direct ACL repair is safe, effective and has excellent short-term outcomes. Knee Surg Sports Traumatol Arthrosc 28, 2551–2556 (2020). https://doi.org/10.1007/s00167-020-05872-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-05872-2