Abstract
Purpose
The purpose of this study was to compare the clinical results, radiographic loosening and early complications between patients undergoing primary knee arthroplasty (TKA) with tibial short stem extension and those with standard stem for gross varus deformities at minimum two years after surgery.
Methods
From a prospective TKA database of 4216 patients, patients with a primary TKA with a tibial short stem extension (30 mm) for severe varus deformity (hip-kneeankle angle, HKA < 170°) and a minimum follow-up of 2 years, were reviewed and compared to a matched control group with tibial components with a standard stem, in a
1:3 ratio. Demographics, surgical parameters, pre- and postoperative alignment and outcome parameters were collected for all patients. The primary outcome was aseptic loosening of the tibial component. Secondary outcomes were knee society scores (KSS), postoperative HKA, general postoperative complications and implant survival rates.
Results
Forty-five patients with tibial short stem extensions (mean HKA 166.2°) were compared in a 1:3 ratio to a matched case–control group of 135 patients with standard stems (mean HKA 167.1°) at a mean follow-up of 57 and 64 months respectively after primary TKA. In the extension stem group, 4 patients encountered complications
(8.9%) versus 12 patients in the standard stem group (8.9%). There were no cases of tibial component loosening in the short extension stem versus four cases in the standard stem group (3%). This difference was significant between groups, p = 0.04.
Conclusion
In patients with varus deformities > 10°, undergoing primary total knee arthroplasty, prophylactic use of a tibial short extension stem may lead to less loosening of the tibial component. In this study, 3% of patient with big varus deformity without stemmed TKA had a tibial implant loosening versus 0% in the stemmed TKA group.
Level of evidence
Level III, case–control study
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Reported TKA revision rates in literature are low and range between 4.9 and 7.8% at 10-years [11], with infection and aseptic loosening being the most frequently encountered complications [14]. Preoperative malalignment increases the risk of aseptic loosening of particularly the tibial component [13], with severe varus deformity being the most important risk factor [8, 15].
In order To distribute load transmission and reduce forces in the proximal tibia, prostheses may be equipped with pegs, keels or stems. Tibial stems further increase the mechanical stability of the tibial component by transmitting forces over the metaphysis and thereby reducing micromotion and tibial lift-off [10, 15].
Several studies have underlined the better mechanical stability of the tibial component with the use of stems, but the focus of these studies has either been on revision surgery or on complex primary cases with gross metaphyseal bone deficiency or the need for constraint [2, 10].
The implant studied here, was a posterior stabilised implant with a third condyle. This implant is known to better distribute load charge on the tibial implant [5]. For this kind of implant, is it necessary to have a stemmed TKA to decrease the tibial loosening implant rate?
The purpose of this study is to compare extension stemmed versus standard tibial components used during primary TKA in gross varus population.
The hypothesis presented is that extension stemmed TKA significantly decrease the rate of tibial loosening in gross varus population thus decreasing strength on medial compartment.
Materials and methods
Population
This single-centre retrospective study was based on prospectively collected data of a cohort of 4216 consecutive primary TKAs performed in the same department between November 1987 and March 2015, by multiple surgeons all of whom used the same surgical technique.
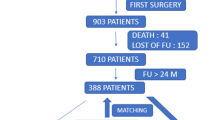
For this study two groups were compared. The first case group consisted of primary TKA’s with tibial short extension stems and then a matched control group with tibial components with a standard stem. Inclusion criteria for both groups were preoperative hip knee ankle angle (HKA) < 170°, first knee surgery and minimum of 24 months follow-up (FU). Groups were matched concerning age, HKA, BMI, and sex in a 1:3 ratio. Total population for this case group consisted of 45 patients and the control group counted 135 patients (Fig. 1).
The mean FU was 57 ± 27 [27–171] months in the extension stem group, and 64 ± 37 [24–215] months in the standard stem group (p = ns).
There were no significant differences between groups regarding age, BMI, preoperative HKA and gender (Table 1).
Ethical considerations
All patients agreed to participate in this study and provided written informed consent. The French advisory committee on health research data processing (Comité Consultatif sur le Traitement de l’Information en matière de Recherche dans le domaine de la Santé, CCTIRS) approved this study on 24 January 2012 and then on 9 March 2015 (approval #11-681).
Operative technique
Since 1996 the technique of a medial parapatellar approach has been systematically used for varus knee.
In this study a posterior referencing technique was used, beginning with the tibial cut and followed by the posterior femoral cut (balancing performed in flexion, then checked in extension and balanced with a distractor before the distal femoral cut). All patella were resurfaced. All the tibial implants were cemented. Instrumentation used was consistent using the same intramedullary technique. Tibial cut angle was 90°; slope was adjusted at 5°. Cutting height for tibia was adjusted at 9 mm related to the medial compartment.
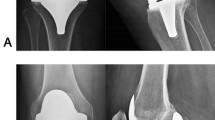
Since 1987, all implants have been designed and fabricated by the same manufacturer (Wright-Tornier-Corin, Montbonnot-Saint-Martin, France). All implants are similarly designed, with a posterior stabilization (HLS family implants). Tibial short extension stems measure 10 mm in diameter and 30 mm in length (Fig. 2).
Follow-up and evaluation of tibial loosening
Clinical outcomes were assessed by determining the international knee society knee and function scores (KSS, 1989) [7]. Radiographic outcomes were assessed on weight-bearing antero-posterior, lateral, 45° patello-femoral and long-leg views. Patients underwent clinical and radiological evaluation after one year and two years, and then every two years postoperatively.
The initial diagnosis of implant loosening was made clinically and radiographically (Fig. 3). Any patient with a suspicion of implant loosening underwent blood testing (CRP and leucocytes); a CT scan to confirm loosening; bone scintigraphy searching for a focus of increased radioactive tracer uptake and a bacteriological biopsy during surgery. If the bacteriological biopsy came back negative, aseptic loosening of the tibial implant was confirmed.
Statistical analysis
The statistical data was analysed using the Chi-square test for the comparison of categorical variables between the two groups and the student t-test for the continuous variables, using the software R (R Foundation for Statistical Calculation, https://www.R-project.org). Survival curves were created according to Kaplan–Meier and compared with a Log Rank test, using the Technical University from Denmark’s online site (https://www.statcom.dk). The statistical significance threshold was set at p < 0.05.
The sample size calculation showed that with a power of 80% (two sized testing at a significant level of p < 0.05) a sample size of 31 patients was needed to show a difference between extension stemmed and standard stemmed group.
Results
Postoperative results (Table 2)
Postoperatively, there were no differences in tourniquet time, KSS knee scores or postoperative coronal angles between the extension stem group and standard stem group.
Postoperative complications (Table 3)
In the short extension stem group, no cases of tibial loosening were encountered.
In the standard stem group, 12 patients presented with a complication (8.9%). Four patients of the standard stem group (3%) had tibial loosening. BMI, postoperative HKA and ATm concerning those four tibial loosening are summarized Table 4.
The difference concerning tibial loosening appeared to be statistically significant (p = 0.04) between both groups. Details of the other complications are summarized in Table 3.
Implant Survival Rate
In the standard stem group, the survival rate with regards to tibial component loosening is 99% at 24 months of follow-up, and 96% at 41 months of follow-up (Fig. 4).
In the extension stem group, the survival rate with regards to tibial component loosening is 100% (Fig. 5).
Using Log Rank test, no significant difference was found in survival rates of the tibial implant between both groups.
Discussion
The most important finding of this study was that prophylactic use of a tibial short extension stem, in patients with gross varus deformities undergoing primary TKA, leads to less loosening of the tibial component when compared to using a tibial component with a standard stem in these cases.
However, the use of stem during primary TKA may have some disadvantages. These may include stem tip pain, risk of periprosthetic fracture or difficulty on revision if needed. However, using a short stem extension instead of a long stem extension may be considered to reduce these disadvantages by providing less bone removal.
In this study, stems used were short stems—30 mm, and stem-dependent complication was not observed in any patient. Indeed, most of stem-dependent complications observed were caused by contact with cortical bone. With short stems, no contact to cortical bone is observed.
Clinical results and complication rates appeared to be similar for both groups. These findings confirm principal hypothesis and are in accordance with literature.
Sorrells et al. [16] found that arthroplasties in patients with severe preoperative varus deformities (HKA < 170°) are more likely to fail than in neutrally aligned knees. However, they also stated that severe preoperative varus leads to postoperative malalignment, possibly contributing to failure independent of preoperative alignment. Ritter et al. [13] subsequently found that neutral postoperative alignment does improve but not eliminate the risk of failure in patients with gross preoperative malalignment (HKA < 172°), thereby directly relating severe preoperative varus deformities to a poorer outcome.
In order To improve mechanical stability and outcomes, the use of tibial stems has been extensively investigated and described. Most studies have mainly focused on revision surgery and/or secondary prostheses [2, 4, 10, 17], but only recently attention has been drawn to the use of tibial short extension stems in primary cases.
With the use of a tibial short extension stem, Lachiewicz and Soileau [6] described excellent fixation of the tibial component. Their study did however focus on knee revision arthroplasty. Angers-Goulet et al. [1] used tibial short extension stems in 91 complex primary cases and described good radiologic and clinical results for up to seven years follow-up in a case series without control group. More recently, Park et al. [12] conducted a study amongst 88 patients (of which a bias of 87 females) with varus deformities (of less than 8°) undergoing primary TKA with a tibial short extension stem and compared their radiological results to a matched control group. They concluded that using a short extension stem for the tibial component in primary TKA in patients with varus deformity (> 8°) may reduce the rate of loosening of the tibial side and increase the longevity of the implant. The results described by Park et al. are much in accordance with results found in the present study [12]. The present study however included patients with slightly larger deformities (> 10°, greater than substantial deformity according to de Muylder classification [3]), and compared gender-heterogeneous matched samples and presented both radiological and clinical results for the total cohort of 180 patients.
Clinical results and complications appeared similar between groups and are in accordance with literature. Noteworthy is the relative high patellar fracture rate in both groups (2.2% tibial extension stem group versus 3.7% in the standard stem group, p = ns). This is something that was also noted by Mouton et al. [9] (2.9% patellar fractures in varus knees > 15°) and they also attributed high patella fracture rate to—devascularization during (more extensive) soft tissue release, increased constraint on the extensor mechanism after correcting varus and relative preoperative patella baja in varus knees.
There are some limitations to this study that need to be acknowledged. By nature of the retrospective study design some degree of bias could have been introduced since patients were not randomized and indication bias for the use of tibial short extension stems may have occurred. Matched control group in a 1:3 ratio was used to try to minimize bias, but not all potential confounding factors could be accounted for in the matching process (e.g. postoperative HKA).
This study has several advantages, including an important study cohort size with a significant mean follow-up of 60 months, concerning the same implant.
The authors would recommend using stem TKA for patients with severe varus deformities, for primary TKA.
Conclusion
In patients with varus deformities > 10°, undergoing primary total knee arthroplasty, prophylactic use of a tibial short extension stem may lead to less loosening of the tibial component. In this study, 3% of the patients without extension stem presented a tibial loosening versus 0% with an extension stem (p = 0.04). No clinical difference was found.
References
Angers-Goulet M, Bedard M (2017) Up to seven years’ follow-up of short cemented stems in complex primary total knee arthroplasty: a prospective study. Knee 24:1166–1174
Barlow BT, Oi KK, Lee YY, Joseph AD, Alexiades MM (2017) Incidence, indications, outcomes, and survivorship of stems in primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 25:3611–3619
De Muylder J, Victor J, Cornu O, Kaminski L, Thienpont E (2015) Total knee arthroplasty in patients with substantial deformities using primary knee components. Knee Surg Sports Traumatol Arthrosc 23:3653–3659
Fleischman AN, Azboy I, Fuery M, Restrepo C, Shao H, Parvizi J (2017) Effect of stem size and fixation method on mechanical failure after revision total knee arthroplasty. J Arthroplasty 32:S202–S208 (e201)
Gaillard R, Lustig S, Peltier A, Villa V, Servien E, Neyret P (2016) Total knee implant posterior stabilised by a third condyle: design evolution and post-operative complications. Orthop Traumatol Surg Res 102:1061–1068
Lachiewicz PF, Soileau ES (2015) A 30-mm cemented stem extension provides adequate fixation of the tibial component in revision knee arthroplasty. Clin Orthop Relat Res 473:185–189
Lingard EA, Katz JN, Wright RJ, Wright EA, Sledge CB, Kinemax Outcomes G (2001) Validity and responsiveness of the Knee Society Clinical Rating System in comparison with the SF-36 and WOMAC. J Bone Joint Surg Am 83:1856–1864
Marcovigi A, Zambianchi F, Giorgini A, Digennaro V, Catani F (2016) The impact of bone deformity on osteoarthritic varus knee correctability. J Arthroplasty 31:2677–2684
Mouton J, Gaillard R, Bankhead C, Batailler C, Servien E, Lustig S (2018) Increased patellar fracture rate in total knee arthroplasty with preoperative varus greater than 15 degrees : a case-control study. J Arthroplasty 33:3685–3693
Nadorf J, Kinkel S, Gantz S, Jakubowitz E, Kretzer JP (2017) Tibial revision knee arthroplasty with metaphyseal sleeves: the effect of stems on implant fixation and bone flexibility. PLoS ONE 12:e0177285
Pabinger C, Berghold A, Boehler N, Labek G (2013) Revision rates after knee replacement. Cumulative results from worldwide clinical studies versus joint registers. Osteoarthr Cartil 21:263–268
Park MH, Bin SI, Kim JM, Lee BS, Lee CR, Kwon YH (2018) Using a tibial short extension stem reduces tibial component loosening after primary total knee arthroplasty in severely varus knees: long-term survival analysis with propensity score matching. J Arthroplasty 33:2512–2517
Ritter MA, Davis KE, Davis P, Farris A, Malinzak RA, Berend ME et al (2013) Preoperative malalignment increases risk of failure after total knee arthroplasty. J Bone Joint Surg Am 95:126–131
Sadoghi P, Liebensteiner M, Agreiter M, Leithner A, Bohler N, Labek G (2013) Revision surgery after total joint arthroplasty: a complication-based analysis using worldwide arthroplasty registers. J Arthroplast 28:1329–1332
Scott CE, Biant LC (2012) The role of the design of tibial components and stems in knee replacement. J Bone Joint Surg Br 94:1009–1015
Sorrells RB, Murphy JA, Sheridan KC, Wasielewski RC (2007) The effect of varus and valgus deformity on results of cementless mobile bearing TKA. Knee 14:284–288
Wang C, Pfitzner T, von Roth P, Mayr HO, Sostheim M, Hube R (2016) Fixation of stem in revision of total knee arthroplasty: cemented versus cementless-a meta-analysis. Knee Surg Sports Traumatol Arthrosc 24:3200–3211
Funding
There is no funding source.
Author information
Authors and Affiliations
Contributions
GF: study design, data collection, statistical analysis, literature review and manuscript writing. BM: literature review and manuscript writing. RG: study design and manuscript editing. CB: manuscript editing and literature review. SL: study design and manuscript editing. ES: study design, supervision, literature review and manuscript editing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article. GF, BM, CB and RG declare that they have no conflict of interest. SL: consultant for Smith and Nephew, Stryker, Medacta, Heraeus, Depuy Synthes, Groupe Lepine, institutional research support from Corin and Amplitude. ES: institutional research support from Corin.
Ethical approval
All the procedures performed in the study were in accordance with the ethical standards of the institutional review board/international ethics commitee for each center and with the 1964 Helsinki Declaration and its later amendments.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fournier, G., Muller, B., Gaillard, R. et al. Increased survival rate for primary TKA with tibial short extension stems for severe varus deformities at a minimum of 2 years follow-up. Knee Surg Sports Traumatol Arthrosc 28, 3780–3786 (2020). https://doi.org/10.1007/s00167-020-05848-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-020-05848-2